Abstract
Background
In patients with acute hypercapnic respiratory failure (AHRF) during exacerbations of COPD, mortality can be high despite noninvasive ventilation (NIV). For some, AHRF is terminal and NIV is inappropriate. However there is no definitive method of identifying patients who are unlikely to survive. The aim of this study was to identify factors associated with inpatient mortality from AHRF with respiratory acidosis due to COPD.
Methods
COPD patients presenting with AHRF and who were treated with NIV were studied prospectively. The forced expiratory volume in 1 second (FEV1), World Health Organization performance status (WHO-PS), clinical observations, a composite physiological score (Early Warning Score), routine hematology and biochemistry, and arterial blood gases prior to commencing NIV, were recorded.
Results
In total, 65 patients were included for study, 29 males and 36 females, with a mean age of 71 ± 10.5 years. Inpatient mortality in the group was 33.8%. Mortality at 30 days and 12 months after admission were 38.5% and 58.5%, respectively. On univariate analysis, the variables associated with inpatient death were: WHO-PS ≥ 3, long-term oxygen therapy, anemia, diastolic blood pressure < 70 mmHg, Early Warning Score ≥ 3, severe acidosis (pH < 7.20), and serum albumin < 35 g/L. On multivariate analysis, only anemia and WHO-PS ≥ 3 were significant. The presence of both predicted 68% of inpatient deaths, with a specificity of 98%.
Conclusion
WHO-PS ≥ 3 and anemia are prognostic factors in AHRF with respiratory acidosis due to COPD. A combination of the two provides a simple method of identifying patients unlikely to benefit from NIV.
Background
An estimated 3.7 million people in the UK have chronic obstructive pulmonary disease (COPD),Citation1 with acute exacerbations of COPD (AECOPD) being the commonest cause for emergency medical admissions. Inpatient mortality rates can reach 25% and may be as high as 50% within 12 months of admission for AECOPD.Citation2,Citation3
Patients with acute hypercapnic respiratory failure (AHRF) and acidosis have the highest mortality rate and need for invasive mechanical ventilation (IMV). Several controlled clinical trials have shown that noninvasive ventilation (NIV) in AHRF significantly reduces both mortality and the need for IMV.Citation4 Ward-based NIV is now standard practice in the management of AHRF in the UK, but mortality rate remains high. A recent UK national audit of COPD admissions reported inpatient and 90-day mortality rates of 25% and 33%, respectively, for patients receiving NIV.Citation5 Furthermore, only 5% of patients with respiratory acidosis received IMV, and only 4% of those who died following NIV administration were given IMV.
This lack of escalation of care suggests that patient selection for NIV in clinical practice is problematic and needs improvement. Whilst IMV may be appropriate for some patients with severe acidosis, AHRF may be the terminal manifestation in a significant proportion. Identifying such patients would reduce futile interventions and enable timely introduction of palliative care.
Several prognostic indicators for patients admitted to hospital with AHRF due to AECOPD have been identified. These include age, severity of acidosis (particularly pH < 7.25), impaired consciousness, a high acute physiology and chronic health evaluation (APACHE) II score, hyperglycemia, and the development of concurrent nonrespiratory organ failure.Citation2,Citation6–Citation11 Identification of high-risk patients may enable appropriate stratification of treatment, including NIV and IMV. However, identifying patients at the terminal stages of their disease is difficult and is usually a matter of clinical judgment.
In a previous study, we showed that performance status in combination with bedside physiological measurements from routine clinical assessment were highly predictive of mortality in patients admitted to hospital with AECOPD.Citation12 The aim of this study was to identify factors associated with inpatient mortality for AHRF with respiratory acidosis due to COPD.
Methods
Study design and patient population
This prospective cohort study was performed in the Respiratory Unit at the Sunderland Royal Hospital, UK. Patients admitted and treated with NIV for AHRF due to AECOPD, between September 2009 and July 2010, were included if a diagnosis of COPD had been previously confirmed by clinical symptoms and spirometry. AECOPD was defined by the presence of two or more of the following features: worsening dyspnea, cough, increased sputum production, and change in sputum color. Exclusion criteria included: (1) a history of asthma, bronchiectasis or other concomitant respiratory diseases; (2) a diagnosis of advanced malignancy; and (3) pulmonary edema or pneumonia on admission.
All patients were given controlled oxygen therapy, corticosteroids, and nebulized bronchodilators. None required hemodynamic support with inotropes or vasopressors. NIV was initiated if there was evidence of AHRF and acidosis (pH < 7.35 and partial pressure of CO2 (pCO2) >45 mmHg) on arterial blood gases (ABGs). NIV was delivered by nurses experienced in NIV, using bilevel positive airway pressure ventilators (BiPAP® Vision®; Royal Philips Electronics, Amsterdam, The Netherlands) with full face masks. Initial settings of inspiratory positive airways pressure (IPAP) and expiratory positive airways pressure (EPAP) were 12 and 4 cm H20, respectively. IPAP was adjusted upwards by 2 cm H2O increments according to the response and patient tolerance. Oxygen was entrained through the mask to maintain peripheral oxygen saturation (SpO2) in the range of 88%–92%. The response to NIV was assessed by ABGs between 1–2 hours after commencing treatment and as clinically indicated thereafter.
The end points of the study were inpatient mortality and mortality at 30 days and 12 months after admission.
Data collection
The severity of COPD was determined by the most recent spirometry reading taken when the patient was clinically stable. This was graded according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) staging classification.Citation13 Other clinical data collected included the use of long-term oxygen therapy, number of hospital admissions for AECOPD in the preceding year, and previous documented episodes of AHRF. Patients’ comorbidities were recorded and quantified using the index of Charlson et al.Citation14
An assessment of patients’ functional status was made using the World Health Organization performance status scale (WHO-PS) (0 = Asymptomatic with normal activity; 1 = Symptomatic on physically strenuous activity but able to carry out work of a light or sedentary nature; 2 = Symptomatic: some limitation of normal activity but up and about >50% of time during day, self-caring; 3 = Symptomatic: in bed/chair >50% of time during the day, requires some help with self-care; and 4 = Chair/Bedbound, cannot carry out any self-care).Citation15
The Glasgow Coma Scale and a composite score of physiological impairment, the Early Warning Score (EWS), were recorded upon admission.Citation16 The EWS is derived from heart rate, systolic blood pressure, respiratory rate, temperature, and AVPU score (consciousness level, based on patients’ being alert, responding to voice, responding to pain, or being unresponsive) ().
Table 1 The Early Warning Score (EWS)
Laboratory measurements included the worst (lowest pH) ABGs prior to commencement of NIV, full blood count, albumin, urea, and C-reactive protein (CRP).
Data analysis
Data was analyzed using SPSS software (SPSS Inc, Chicago, IL, USA). Numeric data are presented as means and standard deviation (SD), unless otherwise stated. Continuous variables were compared by t-test and analysis of variance (ANOVA). A Chi-squared test was used to compare categorical variables in bivariate analysis. Receiver operating characteristic (ROC) analysis was used to identify the cutoff values for continuous variables significantly associated with mortality. Variables significant on univariate analysis (P < 0.05) were included in a stepwise (forward conditional) logistic regression analysis, and association with death was expressed as the odds ratio (OR) (95% confidence interval). The 12-month survival was analyzed using the Kaplan–Meier method and groups compared by log rank test.
Results
There were 65 patients included (55% female) for study. The mean age was 71 (10.5) years. The majority of patients had severe or very severe COPD. Over half (57%) had at least one previous admission with AHRF. The overall inpatient mortality rate was 33.8% (22/65). Mortality was greater in males compared with females (41.4% versus 27.8%) but this was not statistically significant (P = 0.18). The mortality rates at 30 days and at 12 months after admission were 38.5% and 58.5%, respectively.
Mortality was associated with the severity of COPD, longterm oxygen therapy use, and performance status (). Ninety-one percent of nonsurvivors had a WHO-PS ≥ 3. The frequency of hospital admissions for AECOPD and previous episodes of AHRF were not associated with an increased risk of death. There was no difference in the severity of comorbidities between survivors and nonsurvivors.
Table 2 Inpatient demographics, COPD severity, comorbidities, and performance statusTable Footnote¶
shows baseline physiological measurements and the EWS. Nonsurvivors had significantly greater perturbations of respiratory rate, diastolic blood pressure, and the Glasgow Coma Scale. Several laboratory variables were associated with increased inpatient mortality, including severity of acidosis and degree of hypercapnia (). Anemia and hypoalbuminemia were both associated with inpatient death. Urea was increased in 55.4% of cases but was not associated with mortality.
Table 3 Physiological measurements on admission
Table 4 Laboratory variables on admission
Dichotomous variables were determined as described above, for the WHO-PS score, EWS score, diastolic blood pressure, and pH. The univariate analysis of variables associated with inpatient death is shown in . Anemia was associated with increased in-hospital mortality, particularly in female patients: mortality if anemic was 57.1% vs 9.1% (P = 0.003) for females and was 53.8% vs 31.3% (P = 0.18) for males.
Table 5 Univariate analysis of variables associated with inpatient death
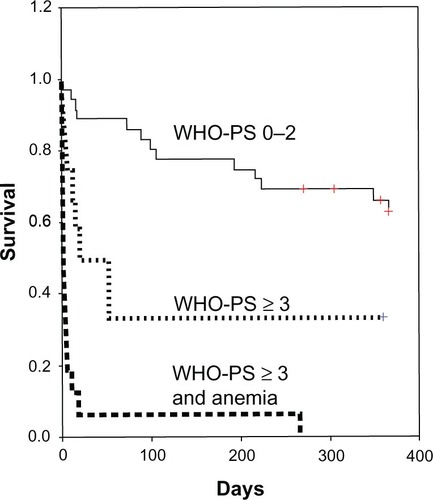
Multivariate analysis of factors associated with inpatient death showed that only WHO-PS ≥ 3 (OR 39.0 [6.83–2 23.6]) (P < 0.0001) and anemia (OR 5.86 [1.28–26.8]) (P < 0.03) were significant. The presence of both predicted 68% of inpatient deaths, with a specificity of 98%. illustrates the effect of combining the WHO-PS and anemia on survival up to 12 months after hospital admission (log rank test P < 0.001).
Discussion
In routine clinical practice, the mortality from AHRF with respiratory acidosis due to COPD is considerable despite treatment with NIV. This study shows that patients who are unlikely to respond to NIV may be identified by a combination of poor performance status (WHO-PS ≥ 3) and anemia.
The inpatient mortality rate in this study is comparable to that of the UK national COPD audit of patients receiving NIV (which showed an inpatient mortality rate of 25%).Citation5 In another study, comparing intensive care–delivered NIV with IMV, the inpatient mortality was similar (NIV 26%).Citation17 But these compare unfavorably with mortality rates observed in other studies of NIV for AHRF.Citation8,Citation9,Citation11 In particular, the inpatient mortality in the YONIV study was only 10% for patients on NIV.Citation8
The differences in mortality rates are probably a reflection of patient selection. Although the YONIV trial was described as a “real world” study, inclusion required pH in the range of 7.25–7.34. In the present study, 50.8% of our patients had pH < 7.25, similar to that of the UK national COPD audit.Citation5 Patients in the studies of Chakrabarti et alCitation9 and Confalonieri et alCitation11 were also significantly less acidotic.
As with previous studies, inpatient mortality was associated with more severe acidosis on admission. However, pH was not independently predictive of inpatient death in our study. Similar observations were reported by Chakrabarti et al.Citation9 One explanation may be that ABGs on admission do not necessarily reflect disease severity. Admission acidosis is often partly iatrogenic. Furthermore, some patients may initially respond to treatment, only to later deteriorate.Citation18 In the UK national COPD audit, the highest mortality was seen in patients who were nonacidotic on admission but who became acidotic later.Citation5 In a previous study, we showed that inpatient deaths from COPD exhibit a bimodal distribution, with early deaths (within 7 days of admission) being related to admission acidosis, whereas later deaths were not.Citation12
Combinations of routine physiological observations have been shown to be of value in predicting survival for patients requiring NIV. One score chart, that includes the Glasgow Coma Scale, APACHE II score, respiratory rate, and pH, identified patients at >50% risk of NIV failure.Citation11 In another study, a combination of baseline respiratory rate, random glucose, and admission APACHE II score was highly (100%) predictive of NIV success.Citation9 However, the APACHE II score is rarely used outside the intensive care unit, and a more straightforward assessment tool is required for routine clinical use.
Simple measurements of functional limitation alone may be more useful in this respect. In the present study, performance status was highly predictive of inpatient death (mortality if WHO-PS ≥ 3 was 69% vs 5.6%) and concurs with our previous observations.Citation12 A UK COPD audit of outcomes for AECOPD showed that performance status was the best predictor of mortality (38% if bed/chairbound vs 2% if normal activity).Citation19 Morretti et al demonstrated that late NIV failure was associated with worse activities of daily living scores.Citation18 Patients with a 6-minute walking distance of <100 m have a 1-year mortality of up to 60%.Citation20 In the study by Chu et al,Citation21 only the MRC dyspnea score was independently predictive of death.
Our observation that anemia is a significantly important predictor of inpatient mortality is also of particular interest. Although COPD is traditionally associated with polycythemia, the prognostic importance of anemia in this population is increasingly recognized. Cote et alCitation22 demonstrated that anemic COPD patients had significantly shorter median survival (49 versus 74 months) compared with nonanemics. In a study of patients requiring IMV, the overall 90-day mortality among anemic COPD patients was 57.1% versus 25% for nonanemics.Citation23 The mechanism of anemia in COPD and its impact on survival are unclear, but it has been suggested that the prognostic importance of COPD-related anemia may be its association with systemic inflammation in severe disease.Citation24 There is increasing evidence of the importance of systemic inflammation in COPD.Citation25 A relationship between mortality and the magnitude of CRP rise during exacerbations has been reported.Citation12,Citation26 Our findings in the present study, of an association between CRP level and death in AHRF due to COPD, were similar.
Patients with COPD that have frequent exacerbations have an increased risk of death.Citation27 However, the frequency of admissions or previous episodes of AHRF were of no prognostic significance in this study. The presence of comorbidities is also of prognostic importance in COPD — in a study of 71,130 patients admitted to hospital with AECOPD, a Charlson score of 5 was associated with a fivefold increase in death in hospital.29 In our previous study, the Charlson score was significantly higher in patients that died, but it was not an independent predictor of mortality.Citation12 It is therefore likely that the differences in performance status between survivors and those that died reflect COPD severity and its systemic effects rather than additional comorbidity.
Follow up of patients surviving an episode of AHRF requiring NIV indicates poor long-term prognosis. In this study, 37% of patients who survived admission died within 12 months. In a similar study of survivors of AHRF treated with NIV, 49% had died within 12 months of discharge from hospital.Citation21 Thus, the probability of medium-term survival needs to be considered prior to commencing NIV. The BODE Index, that comprises markers of disease severity in stable COPD, including forced expiratory volume in 1 second (FEV1), body mass index, exercise capacity, and dyspnea, has been found to be helpful in predicting long-term prognosis.Citation28 However a BODE score in the upper quartile is associated with a 12-month mortality of only 5% and is therefore of little utility in predicting short- to medium-term survival.
We acknowledge the limitations in this observational study from a single unit. However, we have controlled for potentially confounding variables through multivariate analysis. Many of our findings reflect the observations of other studies. We have deliberately included only variables that are measured in routine clinical practice and are therefore easily replicable and of potential clinical utility.
Conclusion
WHO-PS ≥ 3 and anemia are prognostic factors in AHRF with respiratory acidosis due to COPD. A combination of the two provides a simple method of identifying patients unlikely to benefit from NIV. This study showed that mortality remained high despite treatment with NIV, a reflection of the fact that AHRF with respiratory acidosis can be a manifestation of the terminal stage of disease for patients with COPD. Whilst NIV is undoubtedly effective in the majority of patients with AHRF, a substantial proportion are subjected to a futile intervention that may be unpleasant and distressing, when end of life care may be more appropriate. Our study indicates that patients who are unlikely to respond to NIV may be identified by routine clinical assessment, but further studies are required to validate these findings.
Authors’ contributions
All authors had full access to the original data and take responsibility for the integrity of the data and the accuracy of the analysis. HHM led the data collection, and SM led the data analysis. All authors made critical revisions and approved the final version of the submitted report.
Disclosure
The authors report no conflicts of interest in this work.
References
- ShahabLJarvisMJBrittonJWestRPrevalence, diagnosis and relation to tobacco dependence of chronic obstructive pulmonary disease in a nationally representative population sampleThorax200661121043104717040932
- ConnorsAFJrDawsonNVThomasCOutcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments)Am J Respir Crit Care Med19961544 Pt 19599678887592
- SteerJGibsonGJBourkeSCPredicting outcomes following hospitalization for acute exacerbations of COPDQJM20101031181782920660633
- RamFSPicotJLightowlerJWedzichaJANon-invasive positive pressure ventilation for treatment of respiratory failure due to exacerbations of chronic obstructive pulmonary disease [review]Cochrane Database Syst Rev20043CD004104
- RobertsCMStoneRABuckinghamRJPurseyNALoweDNational Chronic Obstructive Pulmonary Disease Resources and Outcomes Project implementation groupAcidosis, non-invasive ventilation and mortality in hospitalised COPD exacerbationsThorax2011661434821075776
- UcgunIMetintasMMoralHAlatasFYildirimHErginelSPredictors of hospital outcome and intubation in COPD patients admitted to the respiratory ICU for acute hypercapnic respiratory failureRespir Med20061001667415890508
- AfessaBMoralesIJScanlonPDPetersSGPrognostic factors, clinical course, and hospital outcome of patients with chronic obstructive pulmonary disease admitted to an intensive care unit for acute respiratory failureCrit Care Med20023071610161512130987
- PlantPKOwenJLElliottMWEarly use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicentre randomised controlled trialLancet200035592191931193510859037
- ChakrabartiBAngusRMAgarwalSLaneSCalverleyPMHyperglycaemia as a predictor of outcome during non-invasive ventilation in decompensated COPDThorax2009641085786219454410
- LiuHZhangTTYeJAnalysis of risk factors for hospital mortality in patients with chronic obstructive pulmonary diseases requiring invasive mechanical ventilationChin Med J (Engl)2007120428729317374279
- ConfalonieriMGarutiGCattaruzzaMSItalian noninvasive positive pressure ventilation (NPPV) study groupA chart of failure risk for noninvasive ventilation in patients with COPD exacerbationEur Respir J200525234835515684302
- MurphySAHaja MydinHFatahSAntunesGPredicting end-of-life in patients with an exacerbation of COPD by routine clinical assessmentRespir Med2010104111668167420537518
- Spirometry for Health Care Providers: Quick Guide. Global Initiative for Chronic Obstructive Lung Disease (GOLD) http://www.goldcopd.orgAccessed February 1, 2013
- CharlsonMEPompeiPAlesKLMacKenzieCRA new method of classifying prognostic comorbidity in longitudinal studies: development and validationJ Chronic Dis19874053733833558716
- OkenMMCreechRHTormeyDCToxicity and response criteria of the Eastern Cooperative Oncology GroupAm J Clin Oncol1982566496557165009
- SubbeCPKrugerMRutherfordPGemmelLValidation of a modified Early Warning Score in medical admissionsQJM2001941052152611588210
- ContiGAntonelliMNavalesiPNoninvasive vs conventional mechanical ventilation in patients with chronic obstructive pulmonary disease after failure of medical treatment in the ward: a randomized trialIntensive Care Med200228121701170712447511
- MorettiMCilioneCTampieriAFracchiaCMarchioniANavaSIncidence and causes of non-invasive mechanical ventilation failure after initial successThorax2000551081982510992532
- RobertsCMLoweDBucknallCERylandIKellyYPearsonMGClinical audit indicators of outcome following admission to hospital with acute exacerbation of chronic obstructive pulmonary diseaseThorax200257213714111828043
- Pinto-PlataVMCoteCCabralHTaylorJCelliBRThe 6-min walk distance: change over time and value as a predictor of survival in severe COPDEur Respir J2004231283314738227
- ChuCMChanVLLinAWWongIWLeungWSLaiCKReadmission rates and life threatening events in COPD survivors treated with non-invasive ventilation for acute hypercapnic respiratory failureThorax200459121020102515563699
- CoteCZilberbergMDModySHDordellyLJCelliBHaemoglobin level and its clinical impact in a cohort of patients with COPDEur Respir J200729592392917251227
- RasmussenLChristensenSLenler-PetersenPJohnsenSPAnemia and 90-day mortality in COPD patients requiring invasive mechanical ventilationClin Epidemiol201031521326654
- SimilowskiTAgustíAMacNeeWSchönhoferBThe potential impact of anaemia of chronic disease in COPDEur Respir J200627239039616452598
- GanWQManSFSenthilselvanASinDDAssociation between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysisThorax200459757458015223864
- Ruiz-GonzálezALacastaDIbarzMMartínez-AlonsoMFalgueraMPorcelJMC-reactive protein and other predictors of poor outcome in patients hospitalized with exacerbations of chronic obstructive pulmonary diseaseRespirology20081371028103318945322
- Soler-CataluñaJJMartínez-GarcíaMARomán SánchezPSalcedoENavarroMOchandoRSevere acute exacerbations and mortality in patients with chronic obstructive pulmonary diseaseThorax2005601192593116055622
- CelliBRCoteCGMarinJMThe body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary diseaseN Engl J Med2004350101005101214999112