Abstract
Purpose
Chronic obstructive pulmonary disease (COPD) poses a significant global health burden despite being largely preventable and treatable. Despite the availability of guidelines, COPD care remains suboptimal in many settings, including high-income countries (HICs) and upper-middle-income countries (UMICs), with varied approaches to diagnosis and management. This study aimed to identify common and unique barriers to COPD care across six countries (Australia, Spain, Taiwan, Argentina, Mexico, and Russia) to inform global policy initiatives for improved care.
Methods
COPD care pathways were mapped for each country and supplemented with epidemiological, health-economic, and clinical data from a targeted literature review. Semi-structured interviews with 17 respiratory care clinicians were used to further validate the pathways and identify key barriers. Thematic content analysis was used to generate the themes.
Results
Six themes were common in most HICs and UMICs: “Challenges in COPD diagnosis”, “Strengthening the role of primary care”, “Fragmented healthcare systems and coordination challenges”, “Inadequate management of COPD exacerbations”, “Limited access to specialized care” and, “Impact of underfinanced and overloaded healthcare systems”. One theme, “Insurance coverage and reimbursement challenges”, was more relevant for UMICs. HICs and UMICs differ in patient and healthcare provider awareness, primary care involvement, spirometry access, and availability of specialized care. Both face issues with healthcare fragmentation, guideline adherence, and COPD exacerbation management. In addition, UMICs also grapple with resource limitations and healthcare infrastructure challenges.
Conclusion
Many challenges to COPD care are the same in both HICs and UMICs, underscoring the pervasive nature of these issues. While country-specific issues require customized solutions, there are untapped possibilities for implementing global respiratory strategies that support countries to manage COPD effectively. In addition to healthcare system-level initiatives, there is a crucial need for political prioritization of COPD to allocate the essential resources it requires.
Introduction
Chronic obstructive pulmonary disease (COPD) is a respiratory condition characterized by irreversible airflow limitation and symptoms such as dyspnoea, cough, and sputum production. The development of COPD is influenced by both environmental and genetic factors, with smoking and air pollution being primary environmental contributors.Citation1 Genetic predispositions also play a crucial role, with various gene polymorphisms linked to increased risk or disease progression.Citation2 COPD most commonly affects older adults, with a notable increase in prevalence, morbidity, and mortality as age advances.Citation3 While COPD has traditionally been associated with men, its prevalence among women is growing due to rising smoking rates among women, occupational exposures, and possibly greater vulnerability of women’s lungs to smoking and other environmental pollutants.Citation4
Despite being preventable and treatable,Citation5 according to the Global Burden of Disease Study, in 2019, COPD accounted for 3.3 million deaths globally.Citation6 COPD is already the third leading cause of death globally, which is seven years ahead of the World Health Organisation’s (WHO) prediction of 2030.Citation7 By 2060, deaths from COPD are expected to rise to 5.4 million.Citation8
The highest age-standardized COPD prevalence is in high-income countries (HICs), where it persists as a significant public health issue due to the considerable healthcare, economic and societal burden.Citation6 It is also an important issue in upper-middle-income countries (UMICs), which are expected to experience an increasing disease burden as their economies grow and populations age.Citation7 Moreover, compared to HICs, UMICs may have more limited resources to respond to increased demands on their health systems, including fewer healthcare facilities and limited availability of essential medications and technologies.Citation9
The Global Initiative for Obstructive Lung Disease (GOLD) provides guidance on a universal and standardized approach to COPD care.Citation8 Despite this widely available guidance, COPD is often suboptimally managed in practice, and guidelines are not followed.Citation10–12 The reasons may include a lack of awareness or familiarity with the guidelines among healthcare professionals, resource constraints, as well as challenges with the implementation of guidelines into routine clinical practice. This is linked to variation in how COPD care is delivered between settingsCitation13–15 and leads to heterogeneity in patient outcomes and quality of life (QoL).Citation16
Currently, no well-established and widely recognized method exists for mapping practical aspects of care delivery to identify deviations from the guideline provisions. One approach is reported by Meiwald et al for COPD Evidenced Care Pathways, which collates and illustrates the steps involved in delivering COPD care across four healthcare settings.Citation17 These Evidenced Care Pathways were developed based on clinical guidelines, peer-reviewed articles, and clinician perspectives, providing a qualitative assessment of differences between clinical practice and guidelines.
A granular understanding of barriers to providing guideline-adherent care in COPD and how they differ across countries with diverse healthcare systems could provide useful insights for policymakers and healthcare providers. This insight could improve policy planning, effective resource allocation and the successful implementation of initiatives to improve care.Citation18
This study seeks to identify common and unique barriers preventing optimal COPD care in three HICs (Australia, Spain and Taiwan) and three UMICs (Argentina, Mexico and Russia) to better inform global policy initiatives that tackle shared barriersCitation19 while ensuring that unique issues are addressed through more tailored approaches.
Materials and Methods
This study used a previously reported mixed-method approachCitation17 to generate Evidenced Care Pathways. A qualitative analysis of the clinician interviews was conducted to evaluate each country’s themes. A narrative synthesis was used to compare themes in HICs and UMICs. The definition of HICs and UMICs was based on the World Bank classification.Citation20
Development of Evidenced Care Pathways: Pragmatic searches were conducted on PubMed and Google Scholar to identify: 1) international and national guidelines for the diagnosis and management of COPD and 2) economic, epidemiological and clinical data about COPD in the study settings. See Supplement 1 for the search strategy. The literature review findings informed the pathway mapping and the discussion guides for the clinician interviews.
Initially, a generic pathway outlining the steps to COPD care was drafted for each country based on the GOLD recommendations. It was further refined using country-specific guidelines.Citation21–26 The pathways were then used as a visual aid in the clinician interviews to assess how current care delivery deviates from guideline provisions. Further changes to the pathways to reflect current care delivery were made following clinicians’ input, using an iterative approach until the final structure of the Evidenced Care Pathway was achieved.
Qualitative analysis of barriers to optimal COPD care: Semi-structured interviews with 17 clinicians were used to develop and validate the structure of the COPD Evidenced Care Pathways and understand clinician-perceived barriers to optimal COPD care. The qualitative analysis followed the consolidated criteria for reporting qualitative research (COREQ) checklist.Citation27
The Research Team and Reflexivity
A summary of the characteristics of the research team and their relationship with the participants is provided in .
Table 1 Characteristics of the research team and their the relationship with the participants
Participant Selection
A total of 39 potential participants were approached through an email invitation, and 17 agreed to participate in the study. The participants met the following criteria: 1) healthcare professionals (HCPs) working in Argentina, Australia, Mexico, Spain, Russia, or Taiwan at the time of the study; and 2) played an active role in diagnosing or managing COPD in any healthcare setting (primary, secondary or tertiary). Purposive sampling was used in all the countries. The choice of the countries was guided by the need to ensure diversity in geography and healthcare systems.
Data Collection
Interviews took place between April – September 2021 online via Microsoft Teams®. All participants were provided with documentation outlining the nature and purpose of the study and how the data would be used, stored and shared (the use of recordings, an external agency for the transcription process and any future uses of the data). Participants provided informed written consent to participate, including consent to quote their words to substantiate the findings, either verbatim or edited for improved clarity. Participants were informed of the estimated length of the discussion. All communications with the healthcare professionals who participated in the study were managed online, including initial contact, scheduling, and conducting the interviews via emails and virtual meetings. This method ensured consistent and effective engagement with participants across the diverse regions represented in the study.
An example of an interview discussion guide is provided in Supplement 2. Two interviewers were present in each call: a lead and a notetaker. An interpreter was present in three interviews. In these cases, only the English translation was transcribed. Seven interviews were conducted in Spanish (both interviewer and interviewee were native speakers), and certified translators later translated the transcripts into English for the thematic analysis. Transcripts were not returned to participants for correction. All participants consented to receive follow-up emails with clarifying questions regarding the Evidenced Care Pathways and were asked to validate the final structure. They were offered the option to receive an honorarium at the end of the process.
Data Analysis
The interview data were analyzed using a mix of deductive and inductive approaches.Citation28 Transcripts were coded using an existing framework (deductive component).Citation17 Data within each theme was then coded line by line to create sub-categories (inductive component). Particular attention has been paid to identifying both common and unique barriers. A note was made if the subtheme implied some form of improvement in COPD care. AS coded the transcripts. OS double-coded 20% of the data (four transcripts) (). Discrepancies were resolved through discussion. Results were anonymized before reporting.
A narrative synthesis was deployed to compare the themes and subthemes across the countries. A note was made where themes or subthemes were not applicable to a country, and details of the country-specific nuances were captured separately.
Ethics
No personal or patient-specific information was collected during the interviews. Participants were asked questions regarding the healthcare services for COPD in their country. Therefore, the project was deemed a service evaluation, and no ethics approval or review was necessary. Any data collected before, during and after the interview was handled following the European Union’s General Data Protection Regulation (GDPR) legislation.
Results
Evidenced Care Pathways
The detailed Evidenced Care Pathways for Argentina, Australia, Mexico, Spain, Russia and Taiwan are presented in Supplement 3. shows an example of an overview page for an Evidenced Care Pathway. The pathways for all countries showed consistency in the organization and care delivery for COPD. They split across three key touchpoints with the healthcare system : pre-diagnosis, diagnosis, and management.
Figure 1 Top-level presentation of the Evidenced Care Pathway. Example from the Argentinian pathway.
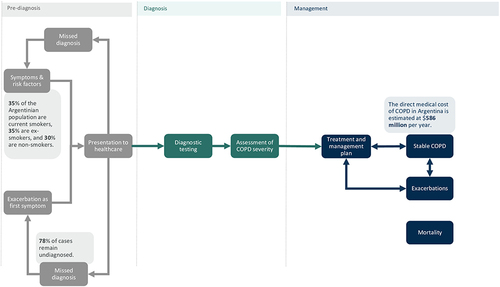
However, differences between the Evidenced Care Pathways were observed. These were mainly related to how patients access specialist care, the tests used for COPD diagnosis, differences in the treatment algorithms, guidelines for managing COPD, and treatment reimbursement.
Themes from Qualitative Analysis of Interviews
Seven themes were identified, covering barriers to COPD care across the six countries. lists the universal primary themes, level two sub-themes, and quotes supporting them. shows where there was variation between countries for the primary themes and pinpoints if there were country-specific nuances within the subthemes.
Table 2 Themes, Subthemes and Quotes Identified from Analyzing 17 Interview Transcripts in Six Countries: Argentina, Australia, Mexico, Russia, Spain, and Taiwan
Table 3 The Variation in Primary Themes Between Countries and Indications Where Country-Specific Nuances Were Identified at the Subtheme Level
Unique features observed in some settings within a given theme are provided, in .
Box 1 Country-Specific Nuances Within Theme 1, Challenges in COPD Diagnosis
Box 2 Country-Specific Features Within Theme 2, Strengthening Primary Care in COPD
Box 3 Country-Specific Features Within Theme 3, Fragmented Healthcare Systems and Coordination Challenges
Box 4 Country-Specific Features Within Theme 4, Inadequate Management of COPD Exacerbations
Box 5 Country-Specific Features Within Theme 5, Limited Access to Specialized Care
Box 6 Country-Specific Features Within Theme 6, Insurance Coverage and Reimbursement Challenges
Box 7 Country-Specific Features Within Theme 6, Insurance Coverage and Reimbursement Challenges
Theme 1: Challenges in COPD Diagnosis
Clinicians identified COPD diagnosis as a significant challenge affecting both patients and healthcare systems. The impact on healthcare systems refers to increased healthcare resource utilization (HCRU), including avoidable hospitalizations, and additional pressures on emergency departments (ED). Not having a COPD diagnosis hinders patients from entering the diagnostic pathway, leading to prolonged periods without treatment. Clinicians expressed concerns about the high prevalence of undiagnosed COPD cases, particularly in countries with a high prevalence of smoking or exposure to biomass fuels, such as Russia, Argentina, and Mexico.
Low awareness about COPD among patients was mentioned as a key factor leading them to adapt to or tolerate the disease without seeking proper medical attention. Clinicians observed that patients often presented with advanced stages of the disease, suggesting reasons such as delays in seeking healthcare, failure to consider COPD by clinicians, lack of spirometry to diagnose it and the lack of timely interventions.
“But, I think a substantial number of patients are undiagnosed in Taiwan, because (…) sometimes we see patients (with) very advanced the COPD (sic). They are not diagnosed before.” - Respiratory specialist, Taiwan.
They also noted that COPD symptoms frequently went unrecognized during multiple visits to healthcare providers before a formal diagnosis was made. Most importantly, clinicians explained how exacerbations are often the driver for initiating the diagnosis process. shows where clinicians reported country-specific nuances for this theme.
Theme 2: Strengthening the Role of Primary Care in COPD
Clinicians emphasized the missed opportunities to enhance the role of primary care in improving COPD diagnosis. They expressed concerns about the limited consideration of COPD by primary care physicians (PCPs), who are typically patients’ first point of contact. Difficulties differentiating COPD symptoms from other conditions, particularly asthma, were highlighted as contributing to misdiagnosis and underdiagnosis.
They even forget how [to interpret] lung function test[s] because they are more familiar with diabetes, more familiar with hypertension (…)”, Respiratory specialist, Taiwan.
Clinicians also identified the lack of access and inconsistent use of spirometry and PCPs’ lack of confidence in interpreting results as significant barriers to timely COPD diagnosis.
Inconsistent use of spirometry in primary care settings adds to the diagnostic challenges. Subsequently, bottlenecks are created in the system if patients rely only on respiratory specialists for diagnosis (Theme 3 and 4). below shows some specific efforts around the guidelines that were raised in the interviews with the Australian physicians.
Theme 3: Fragmented Healthcare Systems and Coordination Challenges Add to the Complexity of Managing COPD
COPD management depends on various factors, including interactions between healthcare providers and patients, healthcare infrastructure availability, and access to treatment options. The healthcare services that COPD patients need are divided between primary care, specialists (in secondary care) and emergency departments. Clinicians reported some disconnect between these services, often leaving patients without adequate management.
Clinicians emphasized the need for effective coordination between patients, primary care physicians, and specialists in managing the complex nature of COPD. They recognized opportunities for clarifying the roles of general practitioners (GPs) and specialists in treatment initiation and follow-up. GPs’ lack of confidence and training in initiating treatment for mild cases was highlighted, reflecting missed opportunities for alleviating the excess burden on secondary care and reducing waiting times, which are important determinants in the patient journey (Theme 2, 5 and 7).
Poor understanding and adherence to pharmacological treatment guidelines were highlighted (mainly among PCPs but in some cases among specialists too). Clinicians expressed concerns about the inadequate understanding of treatment options among healthcare providers, leading to underusing or misusing pharmacological and non-pharmacological interventions.
“70% of [of COPD patients] in Mexico aren’t receiving adequate treatment. Because there’s steroid overuse. Things are the other way around here. A COPD patient is given a bunch of steroids, and an asthma patient is given a bunch of SABA. Things are upside down.”- Respiratory specialist, Mexico.
They acknowledged the impact of poor patient compliance, adherence, and self-management on treatment outcomes, which they believed is sometimes linked to insufficient resources dedicated to patient education. Substantial variation in guideline adherence was reported, particularly among GPs (Theme 1, subtheme 4). below shows distinct elements about this theme that were applicable only to some of the countries.
Theme 4: Inadequate Management of COPD Exacerbations
Clinicians recognized the challenges in effectively managing COPD exacerbations. They observed frequent underreporting, delayed reporting, and misclassification of exacerbations.
“I think that up to 40% of the exacerbations don’t even get to be seen by a specialized physician or at the emergency care unit.”- Respiratory specialist, Argentina.
Inadequate notification systems and a lack of information sharing between healthcare providers reportedly contributed to the ineffective management of exacerbations.
“We are now doing some steps in this direction [setting up a notification system for exacerbations], but usually we know about the situation from our patient.” – Respiratory specialist, Russia.
Clinicians repeatedly emphasized the importance of patient education to enable early identification and appropriate response to exacerbations. They highlighted the need for action plans to be promptly set up or revised following exacerbations to optimize treatment outcomes. Discharged patients may not receive treatment reviews, further perpetuating the cycle of poor management.
Following discharge, patients reportedly need to wait a long time to see a specialist who can review their treatment plan. Clinicians mentioned all the above lead to high readmission rates, which drives costs up and increases pressure on healthcare systems. Comorbidities among COPD patients were also noted as an important determinant of hospitalization, even in mild cases that otherwise would not have led to hospitalization. below shows country-specific nuances within this theme.
Theme 5: Limited Access to Specialized Care
Clinicians highlighted limited access to specialized care as a significant barrier to quality COPD care. They expressed concerns about the shortage of specialists to meet the demands of the COPD patient population, resulting in long waiting times for consultations. This is linked to the over-reliance on specialists to diagnose and manage COPD patients (Theme 2). This theme did not apply to Taiwan, which has generally good access to specialist care.
The concentration of specialists in urban areas was identified as leaving COPD patients in smaller towns and remote locations without access to vital services. Clinicians noted that patients from rural or remote settings may travel long distances to see a specialist. They felt this discouraged these patients from seeking care, reduced compliance, and introduced financial burdens.
”It’s because the number of specialists [in the big cities] is higher than in the rest parts of Russia (sic) historically. I believe that patients might have access to more types of treatment in these two cities [Moscow and St Peterburg] compared to other parts of Russia.”- Respiratory specialist, Russia.
Clinicians mentioned that the increased waiting times to see a specialist can be particularly detrimental to COPD patients because they are either not receiving any treatment or they remain on the wrong treatment regimen, leaving patients at a higher likelihood of experiencing exacerbations.
”I would say if I refer the patient into our public outpatient, I would be warning the patient that it could be anywhere between three to six months before they’ll get seen.”- GP, Australia.
shows country-specific nuances about this theme.
Theme 6: Insurance Coverage and Reimbursement Challenges
This theme applies to Argentina, Mexico, and Russia.
Clinicians highlighted the impact of insurance coverage and reimbursement on COPD management. They observed challenges in drug reimbursement for mild and moderate COPD cases, as coverage often focuses on severe cases. In Russia, deliberate misdiagnosis as asthma reportedly occurs to ensure reimbursement.
Restricted availability and affordability of medications were recognized as factors directly influencing clinical decision-making and leading to inadequate disease management. Moreover, in some countries, clinicians emphasized the challenges patients face in public systems compared to private systems and the negative impact of poor insurance coverage on access to quality COPD care. shows some unique challenges within this theme that were applicable only to some of the countries.
Theme 7: Impact of Underfinanced and Overloaded Healthcare Systems
Clinicians identified underfinanced and overloaded healthcare systems as directly impacting the quality of COPD care. They highlighted system weaknesses that hindered timely diagnosis, comprehensive assessments, and regular monitoring of COPD patients. One example they stated is that short appointments do not allow for a thorough assessment, inhaler technique check, patient education, etc.
”Usually, a physician has to do that [inhaler technique check] during the patient visit. But as far as we know, sometimes the physician is very pressed for time during the visit and, unfortunately, this very important part of the consultation is absent.”- Respiratory specialist, Russia.
Clinicians observed that COPD receives fewer resources within healthcare systems compared to other conditions, such as diabetes or cardiovascular diseases, indicating a need for increased attention and resource allocation. One frequently cited example was the need to have more COPD-dedicated specialised nurses.
”For example, primary care has [specialized] nurses, but I think that they’re not really involved with COPD patients, for instance (sic). I don’t know whether to call this tradition or if they are more used to following up on hypertensive or diabetic patients than on COPD patients.”- GP, Australia.
Even when the clinicians’ understanding of the available treatment options is sufficient, they often report restrictions regarding what they can prescribe or where to refer patients. They mentioned the lack of essential services such as pulmonary rehabilitation, smoking cessation, counselling, patient education, etc. Furthermore, affordability issues were seen to push clinicians to alter treatment plans based on reimbursement options rather than guideline-based care (Theme 6).
The contribution of unrecognized social disparities to poor treatment outcomes among certain COPD patients was emphasized. Addressing these disparities and promoting equity in access to care were identified as crucial steps to enhance COPD management. Variations between regions, particularly in countries with extensive geographical spreads, were noted. shows country-specific nuances within this theme.
Discussion
Main Findings
This research indicated that barriers to optimal care for COPD patients are very similar across all countries, with five out of the seven themes identified in this research applying to all of them: Challenges in COPD diagnosis; Strengthening the role of primary care; Fragmented healthcare systems and coordination challenges; Inadequate management of COPD exacerbations; and, Impact of underfinanced and overloaded healthcare systems. This implies that the challenges faced in delivering effective COPD care are not limited to specific countries and are shared across different contexts. The presence of similar barriers suggests that these issues are pervasive and need to be addressed globally to improve COPD management. It also highlights that COPD continues to be under-prioritized, irrespective of a country’s economic development status and the resilience of its healthcare systems.
Only one theme (Theme 6 - Insurance coverage and reimbursement challenges;) was reportedly more relevant to the UMICs included in this study (Argentina, Mexico and Russia) and was not reported as a barrier by clinicians in HICs (Australia, Spain and Taiwan). Another difference was that Theme 5, Limited access to specialized care, did not apply to Taiwan, where patients have better access to specialists and have short waiting times to see them.Citation29
The development of the Evidenced Care Pathways offered a clear and concise overview of how COPD care is currently delivered across six diverse healthcare settings, depicting the complex interplay of various stakeholders, interventions, and transitions involved in the care process.
Comparing the Findings with Previous Similar Work
Although broadly similar, the theme structure identified in this research differs from that reported by Meiwald et alCitation17 where only four HICs were included (Canada, England, Germany and Japan). The key differences are linked to the emergence of two new themes (Themes 6 and 7) that explain how structural issues across healthcare systems affect COPD care. This difference in the theme structure emphasizes the importance of including countries with less resilient healthcare systems, such as Argentina, Mexico, and Russia.Citation30 Through this inclusive approach, this research provides a better understanding of shared and unique challenges in COPD care in UMICs and HICs.
The themes identified in this study are consistent with another publication that recommends several quality standards in COPD care.Citation31 Four out of five quality standards suggested by clinical experts and patient representatives (timely diagnosis, patient awareness, availability of treatment options and adequate management of exacerbations) overlap with the themes reported here.
Kayyali et al mapped and compared the COPD care delivery pathways in five European countries and, similarly to our findings, reported that most challenges were shared in all countries despite pathway variation.Citation13 These included different manifestations of healthcare system fragmentation, which we also identified as a theme (Theme 3). Kayyali et al emphasized the lack of a specialized role for pharmacists and informal carers,Citation13 which the clinicians interviewed in our study did not report. However, this does not necessarily mean that these issues are not relevant to the countries we studied; instead, they might reflect differences in the discussion guides.
Interpretation of the Findings
Clinicians in both HICs and UMICs face similar barriers, but the scale of the problem described in each theme varies (as outlined in ). Our results suggest UMICs experience a higher burden of COPD and associated challenges.Citation32
Clinicians’ observations revealed a notable difference in the role of exacerbations as drivers of COPD diagnosis between HICs and UMICs. In UMICs, clinicians reported that over 50% of COPD diagnoses are made following an exacerbation. In contrast, this was substantially lower in HICs (10–20%), consistent with other literature on exacerbations.Citation33,Citation34 These perspectives suggest that in UMICs, there might be an even greater delay in recognizing and diagnosing COPD, which could impact timely intervention and disease management.
There were disparities in the perceived availability of services and treatment options for non-pharmacological therapy between HICs and UMICs. Clinicians in Spain, Australia, and Taiwan report better availability of non-pharmacological therapies than clinicians in the UMICs. However, even in these HICs, clinicians acknowledge that existing services are still inadequate to meet the needs of COPD patients. This emphasizes the importance of improving non-pharmacological therapy options across all countries and is consistent with other publications.Citation35,Citation36
Pulmonary rehabilitation was reportedly more accessible in Taiwan and Australia compared to Argentina, Mexico, and Russia, likely reflecting better infrastructure in HICs. Patient management programmes, inhaler technique education, and smoking cessation services were also reportedly more available in HICs. However, HICs and UMICs may face different challenges in these services.Citation37
Treatment availability and affordability reportedly pose greater challenges in UMICs (Argentina, Mexico, Taiwan) than in HICs (Australia, Spain). This indicates the importance of addressing affordability and expanding access to essential treatments and preventive measures in UMICs.Citation38 Given that clinicians in Russia are deliberately misdiagnosing COPD patients with asthma so patients can get reimbursed, it indicates that despite COPD’s high burden, it may not receive the same prioritization and financial support as other noncommunicable diseases (NCDs).Citation39
There were notable differences between public and private healthcare provision in Mexico and Argentina, manifested as stark disparities in COPD care depending on the health insurance individuals can afford. The prominent role of private healthcare was not reported in other countries.
Strengths and Limitations
Interviews with clinicians from six countries facilitated a comprehensive analysis that provides a broader perspective on challenges in diverse healthcare settings. It also enabled us to compare and contrast barriers to the guideline-directed management of COPD in HICs and UMICs. To the best of our knowledge, this comparison has not been previously reported.
Including the graphic presentations of care pathways in the interviews facilitated meaningful discussions with clinicians, as they could see a comprehensive overview of COPD care in their respective countries when considering barriers and deviations from guidelines. However, no African countries were included in this research, and that poses a limitation and suggests it as an area for future research. Expanding the comparative analysis to include African countries would enrich the understanding of variations in COPD care and contribute to a more comprehensive global health perspective.
Another limitation is that interviews occurred in different periods and by multiple researchers, which may have introduced inconsistencies in how questions were asked. Nevertheless, all researchers utilized the same discussion guides, minimizing potential inconsistencies. Additionally, some interviews required interpretation and translation of the transcripts, which may have resulted in the loss of certain subtleties. However, since the analysis did not focus on nuances behind clinicians’ statements, this limitation is of lesser concern.
Lastly, when comparing the barriers between the countries, the differences may not be attributable to real variations in care provision but rather to the information the interviewee gave. It is possible some of their views were not expressed due to a lack of probing by the interviewer.
Policy Implications
The implications of our findings extend beyond this study. Policymakers can utilize the insights from the themes to identify areas where healthcare systems need strengthening for COPD patients. Furthermore, given that most barriers are similar across healthcare settings, there are opportunities for concerted efforts in COPD care through international policy initiatives. While there are many overarching strategies for NCDs generally,Citation40 there is no coordinated strategy to encourage countries to prioritize the prevention and management of COPD (e.g. improved diagnosis through better use of spirometry and guideline-adherent therapy), which is one of the main NCDs driving up global mortality and morbidity rates.Citation41 The findings of this research can inform efforts to develop funded national respiratory strategies, like the ones available for several other NCDs.Citation42,Citation43
Policymakers can leverage the visual presentation of the Evidenced Care Pathways to facilitate discussions, align goals, and encourage interdisciplinary cooperation, leading to better coordination of care, reduced fragmentation, and improved patient outcomes.Citation44
For future research, exploring approaches that further unify and systematize care pathway mapping would be valuable, ensuring academic rigour while informing policy action. The replication of the Evidenced Care Pathways in other countries could be a starting point.
Conclusion
HICs and UMICs differ regarding patient and HCP awareness levels, primary care involvement, spirometry access, and specialized care availability. While both face challenges related to fragmented healthcare systems, guideline adherence, and COPD exacerbation management, UMICs struggle with additional issues stemming from limited resources and healthcare infrastructure.
Most barriers to COPD care are similar across HICs and UMICs, indicating that COPD remains a persistent challenge. While unique issues need to be addressed through tailored approaches, missed opportunities exist to implement international respiratory strategies that encourage countries to take measures to manage COPD adequately. Alongside efforts at the healthcare system level, there is a need for political prioritization of COPD to ensure it is allocated the necessary resources, even in HICs.
Author Contributions
All authors made a significant contribution to the work reported. Anne Meiwald, Elisabeth Adams, Orjola Shahaj and Rupert Gara Adams were involved in the conception, study design, and execution. Krishnan Puri Sudhir was involved with the acquisition of data and interpretation of themes. Peter Wark, Alexis Cazaux, Abelardo Elizondo Rios, and Sergey Avdeev were involved in the conception, analysis and interpretation of themes. All coauthors took part in drafting, revising or critically reviewing the article; agreed on the journal to which the article will be submitted; gave final approval of the version to be published; and agreed to take responsibility and be accountable for the contents of the article.
Disclosure
Orjola Shahaj, Anne Meiwald, Krishnan Puri-Sudhir, Rupert Gara Adams, and Elisabeth Adams worked at Aquarius Population Health at the time of the project. Aquarius Population Health receives consultancy and research fees from other pharmaceutical and MedTech companies that are unrelated to this work. Abelardo Elizondo Rios has served on boards for trials sponsored by AstraZeneca, Bayern, Novartis and GSK. Alexis Cazaux has no conflict of interest concerning the topic of this research. Outside of the submitted work, Sergey Avdeev reports receiving consulting fees and/or fees for attending lectures, meetings and conferences and/or travel expenses and/or research grants from AstraZeneca, Novartis, GSK, Teva, Sanofi, and Chiesi. Peter Wark has no conflict of interest concerning the topic of this research.
Acknowledgments
We want to thank all participants who contributed valuable insight to depict current care for COPD. Many thanks go to Alice Sinclair for coding the transcripts and Mathilde Vankelegom, Nuri Ahmed, Paddy Goddard-Watts, and Aleix Rowlandson for leading some interviews. Lastly, we would like to express our gratitude to Marta Wanat for providing her qualitative expertise to improve the design and reporting of this research. This paper has been uploaded to MedRxiv as a preprint: https://www.medrxiv.org/content/10.1101/2023.11.13.23298474v1.
Additional information
Funding
References
- Marginean C, Popescu M, Vladaia M, Tudorascu D, Pirvu D, Petrescu F. Involvement of Oxidative Stress in COPD. Curr Health Sci J. 2018;44:48–55. doi:10.12865/CHSJ.44.01.08
- Bossé Y. Updates on the COPD gene list. Int J Chron Obstruct Pulmon Dis. 2012;7:607–631. doi:10.2147/COPD.S35294
- Silva Rodriguez ME, Silveyra P. Air pollution exposure as a relevant risk factor for chronic obstructive pulmonary disease exacerbations in male and female patients. Eur Med J. 2022;2022:1.
- Somayaji R, Chalmers JD. Just breathe: a review of sex and gender in chronic lung disease. Eur Respir Rev. 2022;;31:210111.
- Buist S. COPD: a common disease that is preventable and treatable. Prim Care Respir J. 2006;15:7–9. doi:10.1016/j.pcrj.2005.12.004
- Safiri S, Carson-Chahhoud K, Noori M, et al. Burden of chronic obstructive pulmonary disease and its attributable risk factors in 204 countries and territories, 1990-2019: results from the global burden of disease study 2019. BMJ. 2022;378:e069679.
- Quaderi SA, Hurst JR. The unmet global burden of COPD. Glob Health Epidemiol Genomics. 2018;3:e4.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2022 Report); 2021:77. Available from: https://goldcopd.org/. Accessed August 10, 2022.
- Preker AS, Cotlear D, Kwon S, Atun R, Avila C. Universal health care in middle-income countries: lessons from four countries. J Glob Health. 11:16004. doi:10.7189/jogh.11.16004
- Glaab T, Banik N, Rutschmann OT, Wencker M. National survey of guideline-compliant COPD management among pneumologists and primary care physicians. COPD j chronic obstr pulm dis. 2006;3:141–148. doi:10.1080/15412550600829299
- Ragaišienė G, Kibarskytė R, Gauronskaitė R, et al. Diagnosing COPD in primary care: what has real life practice got to do with guidelines? Multidiscip Respir Med. 2019;14:28. doi:10.1186/s40248-019-0191-6
- Ruparel M, López-Campos JL, Castro-Acosta A, Hartl S, Pozo-Rodriguez F, Roberts CM. Understanding variation in length of hospital stay for COPD exacerbation: European COPD audit. ERJ Open Res. 2. doi:10.1183/23120541.00034-2015.
- Kayyali R, Odeh B, Frerichs I, et al. COPD care delivery pathways in five European Union countries: mapping and health care professionals’ perceptions. Int J Chron Obstruct Pulmon Dis. 2016;11:2831–2838. doi:10.2147/COPD.S104136
- Utens C, Maarse J, Schayck O V, Maesen B, Mölken MR V, Smeenk F. Care delivery pathways for chronic obstructive pulmonary disease in England and the Netherlands: a comparative study. Int J Integr Care. 2012;12. doi:10.5334/ijic.811
- Laue J, Melbye H, Halvorsen PA, et al. How do general practitioners implement decision-making regarding COPD patients with exacerbations? An international focus group study. Int J Chron Obstruct Pulmon Dis. 2016;11:3109–3119. doi:10.2147/COPD.S118856
- Quint JK, O’Leary C, Venerus A, et al. Prescribing pathways to triple therapy: A multi-country, retrospective observational study of adult patients with chronic obstructive pulmonary disease. Pulm Ther. 2020;6:333–350. doi:10.1007/s41030-020-00132-7
- Meiwald A, Gara-Adams R, Rowlandson A, et al. Qualitative Validation of COPD evidenced care pathways in japan, Canada, England, and Germany: common barriers to optimal COPD care. Int J Chron Obstruct Pulmon Dis. 2022;17:1507–1521. doi:10.2147/COPD.S360983
- Lennox L, Green S, Howe C, Musgrave H, Bell D, Elkin S. Identifying the challenges and facilitators of implementing a COPD care bundle. BMJ Open Respir Res. 2014;1:e000035.
- Young M, Villgran V, Ledgerwood C, Schmetzer A, Cheema T. Developing a multidisciplinary approach to the COPD care pathway. Crit Care Nurs Q. 2021;44:121–127. doi:10.1097/CNQ.0000000000000345
- World Bank Country and Lending Groups – World Bank Data Help Desk. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Accessed October 27, 2023.
- Cheng SL, Lin CH, Chu KA, et al. Update on guidelines for the treatment of COPD in Taiwan using evidence and GRADE system-based recommendations. J Formos Med Assoc Taiwan Yi Zhi. 2021;120:1821–1844. doi:10.1016/j.jfma.2021.06.007
- México, CENETEC. Diagnóstico y Tratamiento de la Enfermedad Pulmonar Obstructiva Crónica [Diagnosis and Treatment of Chronic Obstructive Pulmonary Disease. Practical Clinical Guide: Evidence and Recommendations]. Guía de Práctica Clínica: Evidencias y Recomendaciones. 2021. Available from: http://www.cenetec-difusion.com/CMGPC/GPC-IMSS-037-21/ER.pdf. Accessed May 16, 2024.
- Ministerio de Salud de la Nación. Guía de Práctica Clínica para el Diagnóstico y Tratamiento de la EPOC [The National Ministry of Health. Practical Clinical Guide to Diagnose and Treat COPD]; 2016:156. Available from: https://bancos.salud.gob.ar/recurso/guia-de-practica-clinica-para-el-diagnostico-y-tratamiento-de-la-epoc. Accessed May 16, 2024.
- Russian Respiratory Society. Chronic obstructive pulmonary disease. Clinical guidelines; 2021. Available from: https://www.spulmo.ru/upload/kr/HOBL_2021.pdf. Accessed May 16, 2024.
- Soler-Cataluña JJ, Piñera P, Trigueros JA, et al. Actualización 2021 de la guía española de la EPOC (GesEPOC). Diagnóstico y tratamiento del síndrome de agudización de la EPOC [The 2021 update of the Spanish guideline on COPD (GesEPOC). Diagnosis and treatment of exacerbation syndrome for COPD]. Arch Bronconeumol. 2022;58:159–170. doi:10.1016/j.arbres.2021.05.011
- Yang IA, Brown JL, George J, et al. COPD-X Australian and New Zealand guidelines for the diagnosis and management of chronic obstructive pulmonary disease: 2017 update. Med J Aust. 2017;207:436–442. doi:10.5694/mja17.00686
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–357. doi:10.1093/intqhc/mzm042
- Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health. 2019;11:589–597. doi:10.1080/2159676X.2019.1628806
- Wu TY, Majeed A, Kuo KN. An overview of the healthcare system in Taiwan. Lond J Prim Care. 2010;3:115–119. doi:10.1080/17571472.2010.11493315
- Ng M, Fullman N, Dieleman JL, Flaxman AD, Murray CJL, Lim SS. Effective coverage: a metric for monitoring universal health coverage. PLOS Med. 2014;11:e1001730.
- Bhutani M, Price DB, Winders TA, et al. Quality standard position statements for health system policy changes in diagnosis and management of COPD: a global perspective. Adv Ther. 2022;39:2302–2322. doi:10.1007/s12325-022-02137-x
- Menezes AMB, Perez-Padilla R, Jardim JB, et al. Chronic obstructive pulmonary disease in five Latin American cities (the PLATINO study): a prevalence study. Lancet. 2005;366:1875–1881. doi:10.1016/S0140-6736(05)67632-5
- Soler-Cataluña JJ, Izquierdo JL, Juárez Campo M, Sicras-Mainar A, Nuevo J. Impact of COPD exacerbations and burden of disease in Spain: AVOIDEX Study. Int J Chron Obstruct Pulmon Dis. 2023;18:1103–1114. doi:10.2147/COPD.S406007
- Naranjo L, Torres-Duque CA, Colodenco D, et al. Highlights of an expert advisory board on acute exacerbations of chronic obstructive pulmonary disease (AE-COPD) in Latin America. Int J Chron Obstruct Pulmon Dis. 2020;15:1919–1929. doi:10.2147/COPD.S261258
- Ur Rehman A, Hassali MAA, Abbas S, et al. Pharmacological and non-pharmacological management of COPD; limitations and future prospects: a review of current literature. J Public Health. 2020;28:357–366. doi:10.1007/s10389-019-01021-3
- Corhay JL, Dang DN, Van Cauwenberge H, Louis R. Pulmonary rehabilitation and COPD: providing patients a good environment for optimizing therapy. Int J Chron Obstruct Pulmon Dis. 2014;9:27–39. doi:10.2147/COPD.S52012
- Desveaux L, Janaudis-Ferreira T, Goldstein R, Brooks D. An international comparison of pulmonary rehabilitation: a systematic review. COPD J Chronic Obstr Pulm Dis. 2015;12:144–153. doi:10.3109/15412555.2014.922066
- Jardim JR, Stirbulov R, Moreno D, Zabert G, Lopez-Varela MV, Montes de Oca M. Respiratory medication use in primary care among COPD subjects in four Latin American countries. Int J Tuberc Lung Dis off J Int Union Tuberc Lung Dis. 2017;21:458–465. doi:10.5588/ijtld.16.0633
- Chuchalin AG, Khaltaev N, Antonov NS, et al. Chronic respiratory diseases and risk factors in 12 regions of the Russian Federation. Int J Chron Obstruct Pulmon Dis. 2014;9:963–974. doi:10.2147/COPD.S67283
- Dugani S, Gaziano TA. Achieving global reduction in cardiovascular mortality. Curr Cardiol Rep. 2016;18:10. doi:10.1007/s11886-015-0679-4
- Halpin DMG, Celli BR, Criner GJ, et al. It is time for the world to take COPD seriously: a statement from the GOLD board of directors. Eur Respir J. 2019;54:1900914. doi:10.1183/13993003.00914-2019
- Jailobaeva K, Falconer J, Loffreda G, Arakelyan S, Witter S, Ager A. An analysis of policy and funding priorities of global actors regarding noncommunicable disease in low- and middle-income countries. Glob Health. 2021;17:68. doi:10.1186/s12992-021-00713-4
- Jackson-Morris A, Nugent R. Tailored support for national NCD policy and programme implementation: an over-looked priority. BMJ Glob Health. 2020;5:e002598.
- Vargas I, AS M-P, Eguiguren P, et al. Lessons learnt from the process of designing care coordination interventions through participatory action research in public healthcare networks of six Latin American countries. Health Res Policy Syst. 2023;21:39.
