Abstract
Aim
To determine the efficacy and usefulness of a chronic obstructive pulmonary disease (COPD) care bundle designed for the initial management of acute exacerbations of COPD and to assess whether it improves quality of care and provides better outcomes.
Introduction
The level of care provided in the emergency department (ED) for COPD exacerbations varies greatly, and there is a need for a more systematic, consistent, evidence-based quality improvement approach to improve outcomes and costs.
Methods
A prospective before and after study was carried out in a university teaching hospital. Fifty consecutive patients were identified in the ED with COPD exacerbations and their management was reviewed. Following the education of ED staff and the implementation of a COPD care bundle, the outcome for 51 consecutive patients was analyzed. This COPD care bundle consisted of ten elements considered essential to the management of COPD exacerbations and was scored 0–10 according to the number of items on the checklist implemented correctly.
Results
Following implementation, the mean bundle score out of 10 improved from 4.6 to 7 (P<0.001). There was a significant decrease in the unnecessary use of intravenous corticosteroids from 60% to 32% (P=0.003) and also a marked improvement in the use of oxygen therapy, with appropriate treatment increasing from 76% to 96% (P=0.003). Prophylaxis for venous thromboembolism also improved from 54% to 73% (P=0.054). The 30-day readmission rate did not significantly improve.
Conclusion
The use of a bundle improves the delivery of care for COPD exacerbations in the ED. There is more appropriate use of therapeutic interventions, especially oxygen therapy and intravenous corticosteroids.
Keywords:
Introduction
Acute exacerbations of chronic obstructive pulmonary disease (COPD) account for a considerable number of acute medical admissions, with the majority being admitted through the emergency department (ED). There were 10,863 admissions in Ireland for COPD in 2010, which account for 2.3% of all hospital inpatients, excluding maternity services, and COPD exacerbations were the most common single reason for hospital admission.Citation1 The mean length of stay was 9.5 days, creating a considerable burden on health services. There is a high mortality rate associated with exacerbations of COPD, and many patients are readmitted within 90 days of discharge.Citation2–Citation4 Many studies have commented on the varying levels of care and outcomes of these admissions and highlighted the need for more systematic, consistent, evidence-based quality improvement approaches to improving outcomes from COPD exacerbations.Citation5,Citation6 In an analysis of almost 70,000 admissions with exacerbations of COPD in the United States, Lindenauer et alCitation6 noted that only 66% of patients received the entire set of recommended care processes. A similar study from Canada showed deficits in the administration of bronchodilators, steroids, antibiotics, and oxygen in the care of patients hospitalized with acute exacerbations of COPD.Citation7 Inappropriate high-flow oxygen administration prior to hospital admission may give rise to hypercapnia, respiratory acidosis, and increased mortality compared with titrated oxygen in patients with exacerbations of COPD.Citation8
With the increasing complexity of management and pressure on time in delivering acute medical care, critical components of appropriate care may be overlooked. One approach to the issue of ensuring adequate delivery of good-quality, safe health care has been the utilization of checklists or bundles of care. These provide in pro forma form a series of key steps that should not be overlooked in the assessment and management of a clinical condition. They have been demonstrated in surgery and in the management of indwelling catheters to improve safety.Citation9,Citation10 Recently, Robb et alCitation11 have used a series of bundles for a number of medical conditions to improve overall hospital mortality.
This study aimed to develop and implement a COPD admission bundle for use in the ED and assess whether it improved overall care in the acute setting. A COPD bundle was developed based on best international evidence and practice. The care and outcome of patients with COPD exacerbations before and after the implementation of the bundle were measured.
Methods
Study design and patient demographics
The study was carried out in the ED of a university teaching hospital in Dublin, Ireland. Inclusion criteria were any patient admitted through the ED with a diagnosis of COPD and evidence of an acute exacerbation with no other acute medical issue at the time of presentation. A diagnosis of COPD was made on the available clinical information, including general practitioner referral letters, spirometry, if available, and clinical assessment. An exacerbation was defined on clinical assessment by the ED physician as the presence of at least one of the following: increased dyspnea, increased sputum volume, or increased sputum purulence.
The study consisted of two separate periods. The initial phase involved a 3-month period to analyze all COPD admissions during this time and retrospectively review the management in the ED and the eventual outcomes. The second phase of the study consisted of a prospective analysis of the management and outcomes in patients with COPD following the implementation of a care bundle designed for patients with COPD exacerbations. This was a pilot feasibility study, as no power calculation was performed; instead, an arbitrary 3-month period was used to assess the use of a care bundle preimplementation and postimplementation.
The design of the COPD bundle consisted of selecting items based on national and international guidelines, a systematic literature review, and input from a multidisciplinary project team.Citation12,Citation13 The goal of the bundle was to be accurate, inclusive, and simple to follow. The COPD bundle from Robb et alCitation11 was modified to incorporate ten elements that should all be implemented within 24 hours of admission. Items were selected for the bundle based on their importance in the management of COPD exacerbations but particularly if they were perceived as being poorly implemented in usual care. Examples of poorly implemented components of acute COPD care were noted from the literature and input from the multidisciplinary team. The clinical advisory group to the COPD program of the Clinical Strategy and Programmes Directorate of the Health Service Executive, Dublin, Ireland, was also canvassed for input.
The ten elements selected for inclusion in the bundle were:
Correct administration of supplemental oxygen
Checking an arterial blood gas
Administration of bronchodilators
Reviewing laboratory results
Obtaining a chest radiograph
Administration of oral antibiotics if no evidence of pneumonia
Administration of oral corticosteroids
Consideration for COPD outreach program
Referral to respiratory service
Commencement of venous thromboembolism prophylaxis.
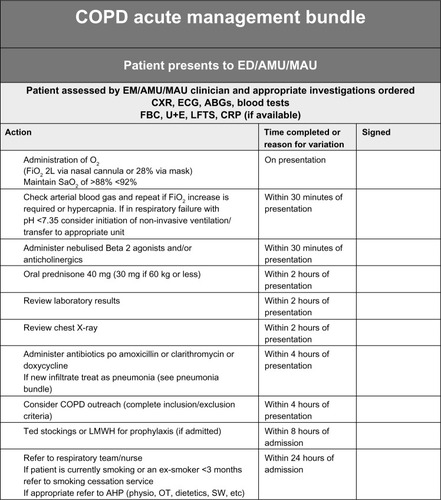
The elements of the bundles were made available to clinicians in a printed bundle, which was attached to the ED notes (see ).
Figure 1 COPD bundle.
Abbreviations: AMAU, acute medical assessment unit; ABGs, arterial blood gases; AHP, allied health professional; AMU, acute medical unit; COPD, chronic obstructive pulmonary disease; CXR, chest X-ray; ECG, electrocardiogram; ED, emergency department; EM, emergency medicine; FiO2, fraction of inspired oxygen; LMWH, low-molecular-weight heparin; MAU, medical assessment unit; O2, oxygen; OT, occupational therapist; SaO2, saturation level of oxygen in hemoglobin; SW, social worker; LFTs, liver function tests; CRP, C-reactive protein; FBC, full blood count; U+E, urea and electrolytes.
This study involved the closure of an audit loop. One of the authors was chairman of the local audit committee and was involved with development of the study from the outset. Ethical approval was consequently not required. The Standards for Quality Improvement Reporting Excellence (SQUIRE)Citation14 guidelines were utilized in the framing of this report.
The COPD outreach program is a service designed to provide a safe, planned, early discharge home from hospital or the ED for patients with an acute exacerbation of COPD. Suitable patients (approximately 20%–25% of patients) are discharged and visited at home by members of the outreach team over the following days until stable. Inclusion and exclusion criteria are outlined in . This service is designed to reduce length of stay and also provides a support service for COPD patients through the provision of pulmonary rehabilitation and education.
Table 1 Demographics of patients pre- and post bundle implementation
Table 2 Inclusion and exclusion criteria for chronic obstructive pulmonary disease (COPD) outreach program
Phase 1 of study: initial assessment of COPD care in the ED
Fifty consecutive patients with an exacerbation of COPD during the initial period from October to December 2010 were reviewed in the ED following admission. Patients were assessed as having an exacerbation of COPD by the ED staff. An alternative diagnosis made in the ED excluded patients who, for example, presented with congestive cardiac failure or pneumonia. A small number of patients may have had an alternative diagnosis made later in their hospitalization. The patients had been assessed and a management plan decided by the admitting medical team when they were reviewed. Demographic data were collected, including age, sex, and forced expiratory volume in 1 second (FEV1). The triage notes, ED physician notes, and medication records were reviewed for evidence of comorbidities of COPD. Documentation in the notes of a comorbidity or record of prescribed medication for one was accepted as evidence supporting the presence of comorbidity. Specifically, records were evaluated for hypertension, ischemic heart disease, congestive cardiac failure, diabetes, osteoporosis, depression, and lung cancer. The smoking status documented in the notes was recorded. A retrospective analysis was carried out on the number of elements involved in the COPD bundle that were correctly followed. Assessment of compliance was made by a specialist respiratory nurse. Subsequently, the length of stay was noted along with the rate of readmission within 30 days and the number of deaths.
Phase 2 of study: assessment of COPD care and outcomes following implementation of the COPD care bundle
To ensure that the COPD bundle would be effectively implemented, an education session for all staff in the ED was held to communicate the reasons for implementing it. This was conducted by a respiratory physician and the respiratory clinical nurse specialists and highlighted evidence of deficits in care of COPD exacerbation in the literature and local experience and the resultant rationale for the components of the COPD bundle. The management of COPD and the rationale for the bundle were also presented and discussed at medical grand rounds. Following this the COPD care bundle was implemented in the ED. Fifty-one consecutive patients with an exacerbation of COPD during the 3-month period from March to May 2011 were suitable for inclusion. Again, all relevant patient demographics were gathered and analyzed in an identical manner to phase 1. Analysis of the implementation of all elements of the bundle was carried out. Similarly, the outcome measures, including length of stay and 30-day readmission rate, were assessed.
Statistical analysis
The differences in both appropriate management and outcomes before and after implementation of the COPD bundle were analyzed using Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) and SPSS (version 17.0.1, IBM Corporation, Armonk, NY, USA). Data were nonparametric in distribution, and the Mann–Whitney U test and χ2 tests were performed. P-values and 95% confidence intervals were calculated. A P-value of <0.05 was considered as representing statistical significance.
Results
There were 50 patients in the preimplementation group and 51 patients in the postimplementation group. The mean age was similar in the two groups at 70 years (range 42–90 years) and 72 years (46–89 years). The sex distribution was similar in both groups: 52% males in the preimplementation group and 59% in the postimplementation group (see ).
There was a slight difference in the mean FEV1 between the two groups; however, this was not statistically significant. The preimplementation group had a mean FEV1 of 1.23 L (53% predicted) and the postimplementation group had a mean FEV1 of 1.01 L (43% predicted). There was no significant difference noted in the comorbidities between both groups, and many of the patients had multiple comorbidities (see ).
Table 3 Comorbidities in pre- and post bundle cohorts
The improvement in appropriate management of COPD exacerbations was evident following implementation of the bundle use. Of the ten elements essential to the initial assessment and management of each exacerbation, initially the mean number of elements addressed was 4.6 (range one to seven). However, following the use of the care bundle, this improved to seven (range three to ten), which was statistically significant (P<0.001) ().
There was a significant improvement in the appropriate early performance of arterial blood gases from 36% to 98% of patients (P<0.001) but no change in the documentation of laboratory or chest X-ray results. With regard to the delivery of appropriate therapy, there was significant improvement with more appropriate prescription of the fraction of inspired oxygen given to each patient. This increased from 76% of patients to 96% receiving the correct oxygen concentration (P=0.003). Similarly, the number of patients given intravenous steroids decreased considerably from 60% of patients to 32% postimplementation (P=0.003). However, there was no significant change in the number of patients receiving intravenous antibiotics, the proportion of patients being 32% preimplementation and 33% postimplementation (P=0.72).
The rate of patients receiving appropriate venous thromboembolism prophylaxis also improved from 54% to 73%. This was not statistically significant but approached significance (P=0.054).
There was no significant change in the 30-day readmission rate: 12% prior to the bundle implementation versus 14% postimplementation (P=0.75). There was no statistically significant difference in the median length of stay: 6 days (range 0–123 days) preimplementation as opposed to 7 days (range 0–60 days) following the bundle implementation (P=0.3779).
Discussion
This study provides further evidence supporting a role for the use of bundles in certain aspects of health care delivery. The results demonstrate that the use of a care bundle to assess and manage patients with acute exacerbations of COPD in the ED is associated with an improvement in the delivery of care. The use of a bundle is simple, easy to follow, and decreases inappropriate management decisions.
The education of emergency staff is vital to improving COPD management, and the use of a bundle augments this type of management.Citation5 The bundle used in this study has ten simple steps and was easy to follow. This study has demonstrated that of the ten elements in the bundle, the average number of elements that were correctly implemented significantly increased from 4.6 to seven. This is a significant increase; however, there is still room for improvement, and ideally all ten elements of the care bundle should always be implemented. Seemingly mundane and simple tasks are often overlooked in the emergency setting, and the use of a bundle helps reduce oversights such as these. Something as simple as referral to a respiratory service within 24 hours should improve care and appropriateness of treatment and allows more efficient long-term follow-up.
An improvement in the 30-day readmission rate and length of stay in hospital in the COPD study population was anticipated. There was no statistically significant improvement in either the readmission rate or length of stay following implementation of the bundle. This may relate to the numbers studied or to the difference in lung function and comorbidities between the two groups. Most likely the relatively small number of patients in both periods contributed to the observed lack of improvement in length of stay following implementation of the bundle. The second group tended to have a lower average FEV1 in both liters and percent predicted. The preimplementation group had a better FEV1 of 1.27 L (60% predicted) compared with an FEV1 of 0.68 L (32% predicted) in the postimplementation group. This may help explain the equivalent readmission rates in the two groups, as although overall care was improved in the second group, they may have been a more severe cohort and had a higher likelihood of experiencing another exacerbation in a short period of time.
The decreased use of intravenous corticosteroids is important, as it decreases the potential side effects from intravenous use compared with the safer oral route of administration. Hyperglycemia in COPD exacerbations has been associated with poor outcomes,Citation15 and previous studies have demonstrated that use of oral corticosteroids is not inferior to intravenous treatment.Citation6,Citation16 In the current environment, where cost is so fundamental to appropriate delivery of care, the increased expenditure from unnecessary treatments is unacceptable. Improving the cost-effectiveness of treatment of COPD exacerbations is vital to further enhance COPD services overall.Citation6,Citation17,Citation18
Although we demonstrated an improvement in quality of care of patients with COPD exacerbations following the introduction of a COPD bundle, it is difficult to be certain that the bundle alone was responsible for this. Any improvement could have been related to the general increased awareness of the need to improve the care of COPD following the demonstration of indices of poor-quality care. It would not have been possible or ethical to do a randomized study in the same institution, and having a prestudy and a post-study does raise the possibility of other factors producing the observed improvement in care. Although this study was carried out in a single center, we believe that with local adaptation this type of COPD bundle could be used widely, as the acute presentation of COPD exacerbations is similar worldwide. This study supports the hypothesis that correct management of acute exacerbations of COPD can be improved with the use of a care bundle, and the results should be widely applicable, as the fundamental elements of management are universal.
Conclusion
This study demonstrates that a simple bundle can improve care of COPD exacerbations. This can help rectify commonly missed elements of care and augment best evidence-based treatments. The use of this bundle not only streamlines care but also has the potential to reduce the risk of adverse effects from unnecessary medications or treatments. Implementing a care bundle could possibly lead to a decrease in the length of stay and reduce readmission rates, but this will require further study. Furthermore, as shown in this study, the use of a bundle can alter prescribing practices and subsequently may have implications in improving costs through reduction of unnecessary medications. Education of all staff involved in the assessment and treatment of COPD exacerbations is essential to further improve COPD care.
Disclosure
The authors report no conflicts of interest in this work.
References
- The Economic and Social Research InstituteActivity in Acute Public Hospitals in Ireland, 2010 Annual ReportDublin, IrelandThe Economic and Social Research Institute Available from: http://www.esri.ie/health_information/latest_hipe_nprs_reports/2010_hipe_report/Accessed October 3, 2013
- RobertsCMBarnesSLoweDPearsonMGEvidence for a link between mortality in acute COPD and hospital type and resourcesThorax2003581194794914586045
- PriceLCLoweDHoskerHSAnsteyKPearsonMGRobertsCMUK National COPD Audit 2003: impact of hospital resources and organisation of care on patient outcome following admission for acute COPD exacerbationThorax2006611083784216449268
- RobertsCMLoweDBucknallCERylandIKellyYPearsonMGClinical audit indicators of outcome following admission to hospital with acute exacerbation of chronic obstructive pulmonary diseaseThorax200257213714111828043
- SenBWoollardMDesiraNLDoes the introduction of a COPD proforma improve the standards of care delivered by junior doctors in the emergency departmentCOPD20107319920320486819
- LindenauerPKPekowPGaoSCrawfordASGutierrezBBenjaminEMQuality of care for patients hospitalized for acute exacerbations of chronic obstructive pulmonary diseaseAnn Intern Med20061441289490316785478
- FitzGeraldJMHaddonJMBradly-KennedyCKuramotoLFordGTRUSIC Study GroupResource use study in COPD (RUSIC): a prospective study to quantify the effects of COPD exacerbations on health care resource use among COPD patientsCan Respir J200714314515217464378
- AustinMAWillsKEBlizzardLWaltersEHWood-BakerREffect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trialBMJ2010341c546
- BerwickDMCalkinsDRMcCannonCJHackbarthADThe 100,000 lives campaign: setting a goal and a deadline for improving health care qualityJAMA2006295332432716418469
- PronovostPNeedhamDBerenholtzSAn intervention to decrease catheter-related bloodstream infections in the ICUN Engl J Med2006355262725273217192537
- RobbEJarmanBSuntharalingamGHiggensCTennantRElcockKUsing care bundles to reduce in-hospital mortality: quantitative surveyBMJ2010340c123420360220
- RabeKFHurdSAnzuetoAGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med200717653255517507545
- CelliBRMacNeeWStandards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paperEur Respir J200423693294615219010
- OgrincGMooneySEEstradaCThe SQUIRE (Standards for QUality Improvement Reporting Excellence) guidelines for quality improvement reporting: explanation and elaborationQual Saf Health Care20081017Suppl 1i1332 PMID: 1883606218836062
- BakerEHJanawayCHPhilipsBJHyperglycaemia is associated with poor outcomes in patients admitted to hospital with acute exacerbations of chronic obstructive pulmonary diseaseThorax200661428428916449265
- de JongYPUilSMGrotjohanHPPostmaDSKerstjensHAvan den BergJWOral or IV prednisolone in the treatment of COPD exacerbations: a randomized, controlled, double-blind studyChest200713261741174717646228
- PatilSPKrishnanJALechtzinNDietteGBIn-hospital mortality following acute exacerbations of chronic obstructive pulmonary diseaseArch Intern Med2003163101180118612767954
- DanielsJMSnijdersDde GraaffCSVlaspolderFJansenHMBoersmaWGAntibiotics in addition to systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2010181215015719875685