Abstract
Background
Whereas the epidemiological association between lung cancer and chronic obstructive pulmonary disease (COPD), a chronic inflammatory respiratory disease, is well known, limited studies have examined the association between lung cancer and non-cystic fibrosis bronchiectasis, a representative chronic airway inflammatory disease. This study evaluated the association between bronchiectasis and lung cancer in patients with COPD.
Methods
A matched case–control study was conducted in a referral hospital in South Korea. Among COPD patients with moderate to very severe airflow limitation (forced expiratory volume in one second/forced vital capacity <0.7 and forced expiratory volume in one second ≤70% [% predicted]) who underwent chest computed tomography (CT) between January 1, 2010 and May 30, 2013, patients with lung cancer and controls matched for age, sex, and smoking history were selected. The risk of lung cancer was assessed according to the presence of underlying bronchiectasis confirmed by chest CT.
Results
The study enrolled 99 cases and 198 controls. Combined bronchiectasis on chest CT was inversely associated with the risk of lung cancer compared with controls (odds ratio [OR] 0.25, 95% confidence interval [CI] 0.12–0.52, P<0.001). Significant associations were found in patients with squamous cell carcinoma (OR 0.11, 95% CI 0.03–0.49, P=0.001) and history of smoking (OR 0.27, 95% CI 0.12–0.57, P<0.001). However, the severity and location of bronchiectasis were not associated with the risk of lung cancer.
Conclusion
Interestingly, the concomitant presence of bronchiectasis in COPD patients was associated with a lower risk of lung cancer.
Introduction
Lung cancer is the leading cause of cancer death in both males and females worldwide.Citation1 In 2011, it caused 22% of all cancer-related deaths in South Korea. The prognosis is poor, with a 5-year survival rate of less than 21%.Citation1,Citation2 Major risk factors and their mechanisms of carcinogenesis have been studied extensively, including cigarette smoking.Citation3 As one of the mechanisms, chronic inflammation, has been recognized in cancers associated with liver cirrhosis, inflammatory bowel disease, burns of the skin, and dental prostheses.Citation4 Rounds of disordered necrotic cell death with subsequent epithelial proliferation resulting in suppressed immunity might contribute to the development of chronic inflammation associated with carcinogenesis.Citation5
Chronic obstructive pulmonary disease (COPD) is a chronic inflammatory disease involving the airways. Inflammation-mediated pathways might involve immune and non-immune systems, producing chemical mediators such as eicosanoids, cytokines, growth factors, and reactive oxygen species.Citation6 Therefore, chronic inflammation is likely to play a key role in the pathogenesis of lung cancer in COPD patients.Citation7–Citation9 The epidemiological evidence of associations between lung cancer and COPD supports this hypothesis.Citation10 Recently, it was reported that respiratory diseases, especially bronchitis and emphysema, increase the risk of lung cancer.Citation11
However, the lack of studies evaluating the association between lung cancer and chronic inflammatory lung diseases other than COPD means that the evidence for this mechanism is still weak. COPD itself is regarded as a chronic inflammatory airway disease and it is often accompanied by destruction of the bronchioles or bronchiectasis causing chronic local and systemic inflammation.Citation3,Citation7 Non-cystic fibrosis (non-CF) bronchiectasis is a representative chronic airway inflammatory disease, which is characterized by abnormal, permanent dilatation of the bronchi accompanied by high levels of inflammatory cytokines.Citation12 However, most of the mechanism of airway inflammation in bronchiectasis remains unclear. Furthermore, the association between bronchiectasis and lung cancer has been rarely studied.
Interestingly, one study reported elevated serum TGF-β1 levels in patients with bronchiectasis; TGF-β1 potentially protects against carcinogenesis.Citation12–Citation14 In patients with CF, an autosomal recessive disease with radiological features of bronchiectasis, the CF gene mutation is inversely associated with malignancies such as melanoma, breast cancer, colon cancer, and prostate cancer.Citation15 These reports suggest that the association between non-CF bronchiectasis and lung cancer might not be consistent with the positive association between chronic bronchitis/emphysema and lung cancer, and on the basis of these findings, we assumed that non-CF bronchiectasis could be associated with lower risk of lung cancer in COPD patients. Therefore, this study was aimed to evaluate the association between non-CF bronchiectasis and lung cancer in patients with COPD, who are thought to be susceptible to lung cancer.
Materials and methods
Study design and subjects
A matched case–control study was conducted at Seoul National University Boramae Medical Center, a referral hospital in South Korea. We screened COPD patients older than 40 years who had moderate to very severe airflow limitation with a post-bronchodilator forced expiratory volume in one second (FEV1) ≤70% and FEV1/forced vital capacity (FVC) <0.7 and who underwent chest computed tomography (CT) between January 1, 2010 and May 30, 2013.Citation16
From among the screened patients, the case group included patients who were diagnosed with lung cancer pathologically. Patients were excluded if they had bronchiectasis secondary to mechanical obstruction with lung cancer. Matched controls were selected from the screened patients with no evidence of lung cancer on chest CT. Two matched controls were chosen per case with lung cancer after matching for age (range ±5 years), sex, and amount smoked in pack-years (range ±10 pack-years). This study was approved by the Institutional Review Board of Seoul National University Hospital Boramae Medical Center (IRB No 16-2014-137).
Demographic data were evaluated in all cases and controls, including smoking history, baseline spirometric measurements, duration of COPD before the CT evaluation, Charlson comorbidity index, and previous bronchiectasis.Citation17
Bronchiectasis was defined based on the chest CT findings.Citation18 A radiologist (K-N Jin) and a pulmonologist (YW Kim) analyzed the CT independently, and arrived at a consensus decision after a discussion if their evaluations were inconsistent. The numbers and location of affected lobes were also analyzed. The severity of the bronchiectasis in each affected patient was evaluated according to the modified Bhalla scoring system.Citation19
Data analysis
The data are presented as medians and interquartile ranges (IQRs) for age and as means and standard deviations (SDs) for other continuous variables. Fisher’s exact test and the chi-squared test were used to compare categorical variables. Odds ratios (ORs) were presented with 95% confidence intervals (CIs) and P<0.05 was considered statistically significant. All analyses were performed using the SPSS software, version 19.0 (IBM Corporation, Armonk, NY, USA).
Results
Baseline characteristics of the study population
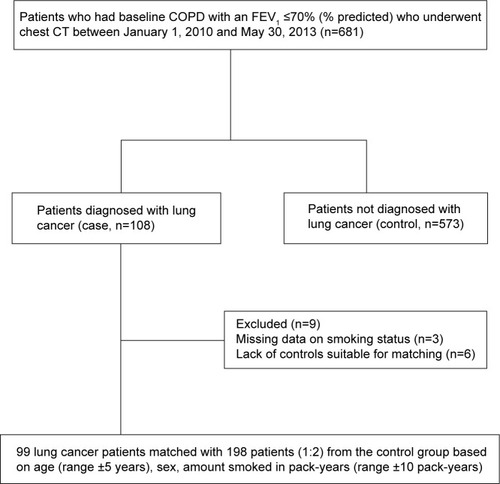
Of the 108 screened lung cancer patients with underlying COPD, three eligible patients were subsequently excluded due to missing demographic data, and six were excluded during the matching procedure due to lack of matched controls. The flow chart for patient enrollment and exclusion/matching is outlined in . Ultimately, 99 COPD patients with lung cancer and 198 matched COPD patients without lung cancer were selected. The baseline characteristics of the study population are summarized in .
Table 1 Baseline characteristics of study population
Figure 1 Flow diagram of the study population.
The median age of the study population was 71 (IQR 64–75) years and males were predominant (94.3%). Only 10% of the study population comprised COPD patients with no smoking history. There were no significant differences in age, sex, amount of smoked measured in pack-years, spirometry results, duration of COPD, and Charlson comorbidity index between the two groups.
Characteristics of lung cancer and bronchiectasis
Of the 99 COPD patients with lung cancers, 80 (80.8%) were diagnosed with non-small cell lung cancer: squamous cell carcinoma (49.5%) was the most common, followed by adenocarcinoma (23.2%), and poorly differentiated carcinoma (6.0%). Of these 80 patients, 38 (47.5%) had advanced disease (stage IV) at the time of diagnosis. Of the 19 patients diagnosed with small-cell lung cancer, ten were at an advanced stage with extensive disease. The detailed histological types and stages of the patients with lung cancer are described in .
Table 2 Histologic types, tumor size, and staging of diagnosed lung cancer
Bronchiectasis was found in 71 patients (10/99 patients with lung cancer [10.1%] versus 61/198 patients without lung cancer [30.8%]). The mean FEV1/FVC and FEV1 % predicted (± SD) were 50.6 (±11.2) and 50.9 (±13.4), respectively. The spirometric results were not different from those of patients without bronchiectasis (P>0.05). In addition, when evaluating the 71 patients with bronchiectasis, spirometric results of patients were not different according to the presence of lung cancer ().
Table 3 Characteristics of concomitant bronchiectasis
Overall, the mean number of bronchiectasis-involved lobes was two. The distribution of affected lobes did not differ according to the presence of lung cancer. In both groups, bronchiectasis most commonly involved the right upper lobe, right lower lobe, and left upper lobe (). Of the ten patients with concomitant bronchiectasis and lung cancer, lung cancer and bronchiectasis were found in the same lobe in two patients (one each in the right upper and left lower lobes). In the remaining patients, lung cancer and bronchiectasis were located separately.
When classifying 71 COPD patients with combined bronchiectasis by smoking status, 62 patients (87.3%) were current or former smokers. There was no statistically significant difference in the distribution of bronchiectasis between current/former smokers and never-smokers (P=0.90). In both groups, the bronchiectasis most commonly involved the right upper lobe (25.0% and 31.0%), left upper lobe (31.3% and 23.0%), and right lower lobe (18.8% and 23.0%).
Association between bronchiectasis and lung cancer
On analyzing the association between bronchiectasis and lung cancer in patients with lung cancer and the controls, concomitant bronchiectasis was inversely associated with the risk of lung cancer in COPD patients with FEV1 (% predicted) ≤70 (OR 0.25, 95% CI 0.12–0.52, P<0.001).
When the risk was assessed by histological type of lung cancer and smoking status of the patients, concomitant bronchiectasis was associated with a lower risk of lung cancer in patients with squamous cell carcinoma (OR 0.11, 95% CI 0.03–0.49, P=0.001) and no significant association was seen in other histological types of lung cancer. When analyzing only COPD patients with current or former smoking status, concomitant bronchiectasis was significantly associated with lower risk of lung cancer (OR 0.27, 95% CI 0.12–0.57, P<0.001), and histological type of squamous cell carcinoma (OR 0.13, 95% CI 0.03–0.61, P=0.009) ().
Table 4 The effect on concomitant bronchiectasis on the risk of lung cancer
Discussion
Through this study, we found that the concomitant presence of bronchiectasis in advanced COPD patients with FEV1 ≤70% (% predicted) was associated with a lower risk of lung cancer. The association was prominent in patients with squamous cell lung cancer and current or former smokers. To our knowledge, this is the first report describing an association between bronchiectasis and lung cancer in COPD patients.
Although there is no other evidence supporting our results that suggests a pathophysiological mechanism, there is indirect biological plausibility supporting our findings. CF is a life-limiting autosomal recessive disorder involving the CFTR mutation and shows the radiological features of bronchiectasis. In CF patients, the CF gene mutation is inversely associated with the incidence of melanoma, breast cancer, colon cancer, and prostate cancer.Citation15,Citation20 Furthermore, a case–control study suggested that the ∆F508 deletion in the CFTR gene is an important protective variant for lung cancer risk.Citation15 This finding concurs with our results for patients with non-CF bronchiectasis. In addition, the chronic inflammation caused by bronchiectasis might act in a different way and produce different cytokines compared to the inflammation caused by COPD, such as TGF-β1.Citation12 The different mechanism of inflammation and cytokines would be a key clue to the protective effect of bronchiectasis against carcinogenesis seen in COPD patients. However, more research is needed to determine mechanisms underlying our findings.
Since previous studies reported a positive association between the chronic inflammation in COPD and an increased risk of squamous cell carcinoma, it is also notable that the statistical association between bronchiectasis and lung cancer was most prominent in patients with squamous cell carcinoma in our study.Citation7,Citation21 Squamous cell carcinoma of the lung is associated with exposure to smoking. In this study, the protective effect of bronchiectasis against lung cancer was obvious in patients with a history of smoking. These findings constitute indirect evidence of a biologically plausible inverse association between bronchiectasis and lung cancer.
The fact that there was only one lung cancer patient diagnosed among COPD patients without exposure to cigarette smoking in our study makes it hard to conclude or compare the relationship between bronchiectasis and lung cancer in patients without cigarette smoking. Since COPD in never-smokers is known to have different characteristics from COPD among smokers, there is possibility that bronchiectasis may also effect the never-smoker population in a different way.Citation22 As expected, the results of patients with exposure to cigarette smoking were in accordance with the results of all COPD patients, showing lower risk of overall lung cancer and squamous cell carcinoma among patients with concomitant bronchiectasis.
It is also generally accepted that bronchiectasis is a long-standing condition that follows infection in childhood or adolescence, while lung cancer usually develops within 5 years of the time of diagnosis.Citation23,Citation24 Therefore, it is reasonable to think that any bronchiectasis preceded the development of lung cancer. This suggests a temporal relationship between the two diseases, rather than a coincidental finding.
To date, most of the mechanisms of airway inflammation in bronchiectasis, and the association between bronchiectasis and lung cancer remains unclear. Recently, a nationwide cohort study from Taiwan reported that patients with underlying bronchiectasis had a 2.36-fold increased risk of lung cancer compared to patients without bronchiectasis. However, the study had limitations in confirming the disease status only by diagnosis codes provided from the registered hospitals. Moreover, the database used in the study did not contain information of smoking history, a possible strong confounding factor when evaluating risk of lung cancer.Citation25 In comparison with the recent large study, our study had strengths in accuracy of diagnosis, information of smoking status, and temporal relationship.
Although our study population was small, we attempted to minimize possible biases. First, bronchiectasis was evaluated based on CT findings, enabling us to confirm the disease objectively and obtain detailed data on its extent and location in the lung. Second, missing data were minimized by reviewing all available medical records. The effects of potential confounding factors in lung cancer, such as age, sex, amount smoked, duration of COPD, and severity of airflow limitation, were controlled by matching or adjustment. In addition, by selecting the controls from the patients with COPD who underwent chest CT, there was no chance of including patients with undetected lung cancer during the interval until the most recent chest CT taken after the patient was diagnosed with COPD.
Despite its interesting findings, there were several limitations to this study. As we selected a cancer-susceptible population and restricted it to COPD patients with more severe airflow limitation, the final sample size was small. However, our well-matched case–control study showed consistent results. Another concern is that since bronchiectasis is frequently associated with mild obstructive patterns shown in spirometry, the inclusion of COPD patients using spirometric results may have been confounded by the impact of bronchiectasis. Moreover, since the relationship between bronchiectasis and smoking is unclear, analyzing bronchiectasis patients with or without smoking history together may also have confounding effects. However, the fact that no differences were observed in the spirometric results between patients with and without bronchiectasis, and that distribution of bronchiectasis in current or former smokers and never-smokers was similar supports the validity of our results. In addition, selecting patients with COPD who underwent chest CT might have resulted in selection bias, enrolling COPD patients with severe airflow limitation or a high risk of cancer. This might make it difficult to generalize the inverse association between bronchiectasis and lung cancer to the general population. Further studies evaluating the protective effect of concomitant bronchiectasis on lung cancer in various populations, including a large cohort, are mandatory.
In conclusion, the concomitant presence of bronchiectasis in COPD patients with moderate to very severe airflow limitation was inversely associated with the risk of lung cancer. This association was prominent in patients with squamous cell carcinoma and current or former smokers. Based on our results, it would be necessary to explore the possible protective effect of bronchiectasis on lung cancer in a large cohort.
Disclosure
The authors report no conflicts of interest in this work.
References
- PirozynskiM100 years of lung cancerRespir Med2006100122073208417056245
- JungKWWonYJKongHJCancer statistics in Korea: incidence, mortality, survival, and prevalence in 2011Cancer Res Treat201446210912324851102
- de TorresJPBastarrikaGWisniveskyJPAssessing the relationship between lung cancer risk and emphysema detected on low-dose CT of the chestChest200713261932193818079226
- TakiguchiYSekineIIwasawaSKurimotoRTatsumiKChronic obstructive pulmonary disease as a risk factor for lung cancerWorld J Clin Oncol20145466066625300704
- VakkilaJLotzeMTInflammation and necrosis promote tumour growthNat Rev Immunol20044864164815286730
- FischerBMVoynowJAGhioAJCOPD: balancing oxidants and antioxidantsInt J Chron Obstruct Pulmon Dis20151026127625673984
- RavivSHawkinsKADeCampMMJrKalhanRLung cancer in chronic obstructive pulmonary disease: enhancing surgical options and outcomesAm J Respir Crit Care Med201118391138114621177883
- BallazSMulshineJLThe potential contributions of chronic inflammation to lung carcinogenesisClin Lung Cancer200351466214596704
- ArdiesCMInflammation as cause for scar cancers of the lungIntegr Cancer Ther20032323824615035887
- HoughtonAMMoudedMShapiroSDCommon origins of lung cancer and COPDNat Med200814101023102418841139
- DenholmRSchuzJStraifKIs previous respiratory disease a risk factor for lung cancer?Am J Respir Crit Care Med2014190554955925054566
- MakJCHoSPLeungRYElevated levels of transforming growth factor-beta(1) in serum of patients with stable bronchiectasisRespir Med200599101223122816140222
- Vendramini-CostaDBCarvalhoJEMolecular link mechanisms between inflammation and cancerCurr Pharm Des201218263831385222632748
- MassagueJTGFbeta in CancerCell2008134221523018662538
- LiYSunZWuYCystic fibrosis transmembrane conductance regulator gene mutation and lung cancer riskLung Cancer2010701142120116881
- VestboJHurdSSAgustiAGGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2013187434736522878278
- CharlsonMEPompeiPAlesKLMacKenzieCRA new method of classifying prognostic comorbidity in longitudinal studies: development and validationJ Chronic Dis19874053733833558716
- PasteurMCBiltonDHillATBritish Thoracic Society Bronchiectasis non-CF Guideline GroupBritish Thoracic Society guideline for non-CF bronchiectasisThorax201065Suppl 1i1i5820627931
- HabesogluMATercanFOzkanUEffect of radiological extent and severity of bronchiectasis on pulmonary functionMultidiscip Respir Med20116528429022958727
- PaduaRAWarrenNGrimshawDThe cystic fibrosis delta F508 gene mutation and cancerHum Mutat199710145489222759
- PapiACasoniGCaramoriGCOPD increases the risk of squamous histological subtype in smokers who develop non-small cell lung carcinomaThorax200459867968115282388
- ZhangJLinXFBaiCXComparison of clinical features between non-smokers with COPD and smokers with COPD: a retrospective observational studyInt J Chron Obstruct Pulmon Dis20149576324426780
- BarkerAFBronchiectasisN Engl J Med2002346181383139311986413
- McShanePJNaureckasETTinoGStrekMENon-cystic fibrosis bronchiectasisAm J Respir Crit Care Med2013188664765623898922
- ChungWSLinCLHsuWHKaoCHIncreased risk of lung cancer among patients with bronchiectasis: a nationwide cohort studyQJM Epub20141130
