Abstract
Background
Acute respiratory failure (ARF) is a life-threatening event, which is frequently associated with the severe exacerbations of chronic obstructive pulmonary disease (COPD). Hypoalbuminemia is associated with increased mortality in patients with COPD. However, to date, little is known regarding whether or not hypoalbuminemia is a risk factor for developing ARF in COPD.
Methods
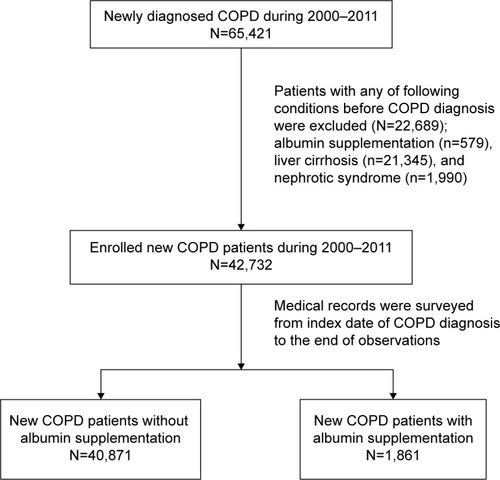
We conducted a retrospective cohort study using data from the National Health Insurance system of Taiwan. A total of 42,732 newly diagnosed COPD patients (age ≥40 years) from 1997 to 2011 were enrolled. Among them, 1,861 (4.36%) patients who had received albumin supplementation were defined as hypoalbuminemia, and 40,871 (95.6%) patients who had not received albumin supplementation were defined as no hypoalbuminemia.
Results
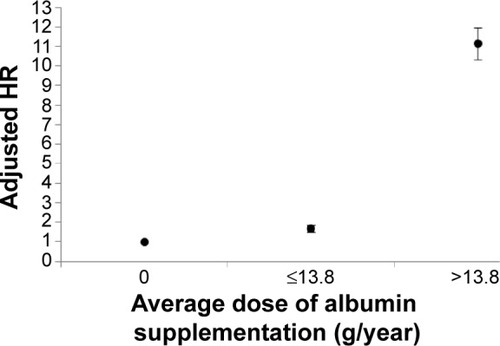
Of 42,732 newly diagnosed COPD patients, 5,248 patients (12.3%) developed ARF during the 6 years follow-up period. Patients with hypoalbuminemia were older, predominantly male, had more comorbidities, and required more steroid treatment and blood transfusions than patients without hypoalbuminemia. In a multivariable Cox regression analysis model, being elderly was the strongest independent risk factor for ARF (adjusted hazard ratio [HR]: 4.63, P<0.001), followed by hypoalbuminemia (adjusted HR: 2.87, P<0.001). However, as the annual average dose of albumin supplementation was higher than 13.8 g per year, the risk for ARF was the highest (adjusted HR: 11.13, 95% CI: 10.35–11.98, P<0.001).
Conclusion
Hypoalbuminemia is a strong risk factor for ARF in patients with COPD. Therefore, further prospective studies are required to verify whether or not albumin supplementation or nutritional support may help to reduce the risk of ARF in patients with COPD.
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by progressive, partially reversible airflow obstruction and lung hyperinflation with significant extra-pulmonary manifestations and comorbid conditions.Citation1–Citation3 It is the fourth leading cause of chronic morbidity and mortality in the USCitation4 and is projected to rank fifth in 2020 in terms of burden of disease worldwide.Citation5,Citation6 The natural course of COPD includes progressively declining lung function and a number of episodic exacerbations, which is defined as a worsening of respiratory symptoms requiring treatment with oral corticosteroids or antibiotics.Citation7 Acute exacerbation (AE) is highly correlated with increased emergency department (ED) visits, respiratory failure, hospitalizations, and deaths in patients with COPD.Citation8,Citation9
Acute respiratory failure (ARF) is a common and life-threatening event, which is frequently associated with severe AE of COPD.Citation10 Short-term or long-term outcomes following ARF in COPD are poor, with a 2-year mortality rate of 49% and quite frequent intervals of readmission.Citation11 In addition, several patients with COPD develop prolonged invasive ventilation following ARF, which is another critical issue in terms of health care in cases of COPD.Citation12 Therefore, greater effort with regards to the prevention and recognition of COPD at risk of ARF is needed to decrease its ever-increasing impact.
Hypoalbuminemia is the result of the combined effects of inflammation and inadequate protein and caloric intake in patients with chronic disease.Citation13 Several studies have shown that hypoalbuminemia is associated with increased mortality in patients with COPDCitation11,Citation14,Citation15 and is also an independent risk factor for a prolonged length of stay in AE of COPD.Citation16 However, whether or not hypoalbuminemia is a risk factor for developing ARF in COPD remains known.Citation17
This study attempts to determine if hypoalbuminemia is a risk factor for developing ARF in COPD. We conducted a retrospective cohort study using nationwide population-based data, the National Health Insurance Research Database (NHIRD) of Taiwan.
Materials and methods
Data source
Data in the present study were retrieved from LHID2000, a part of Taiwan’s NHIRD. The NHIRD stores the claim data of Taiwan’s National Health Insurance (NHI), which is a NHI program implemented by Taiwanese government in 1995. Enrollment in the NHI program is compulsory for all Taiwanese citizens and those residents with an Alien Resident Certificate. The NHI covers >98% of the population in Taiwan and provides a broad range of comprehensive medical services. The NHIRD comprises information about diagnoses (coded in International Classification of Diseases, Version 9, Clinical Modification [ICD-9-CM]), clinical procedures, and medications for outpatient and inpatient visits as well as patients’ sociodemographic status. LHID2000 is a randomized sample of one-million out of 23-million beneficiaries in Taiwan’s NHIRD in 2000. By use of an encrypted unique identification number for each of the individuals, the claim data of the one-million patients from 1997 to 2011 were linked.
Study population and study design
We identified 65,421 incident COPD patients (aged >40 years) in LHID2000 from 1997 to 2011. They were first diagnosed as COPD (ICD-9-CM code: 491, 492, or 496) either based on their outpatient records as more than twice within the 365 days or at least once in inpatient records from 2000 to 2011.
Definition of hypoalbuminemia
As we could not obtain the serum albumin level from the NHIRD, we used the frequency of albumin supplementation to define the severity of hypoalbuminemia in this study. Albumin supplementation is covered by our health insurance program when a patient’s serum albumin level is <2.5 g/dL with underlying disease, such as liver cirrhosis, nephrotic syndrome, severe burn, or shock. However, in actual clinical practice, many physicians prescribe albumin to patients only because of low serum albumin level (<2.5 g/dL), but do not consider the underlying disease.
To avoid baseline inequity of albumin level, we excluded those who had been supplied with albumin before a COPD diagnosis was made. To focus on the role of malnutrition to the development of respiratory failure in COPD patients, patients with prior histories of liver cirrhosis or nephritic syndrome were excluded (). A total of 42,732 newly diagnosed COPD patients were enrolled into the data analysis. Among them, 1,861 (4.36%) patients who had been supplied with albumin during their follow-up period and were classified as the hypoalbuminemia group; 40,871 (95.6%) patients had never been supplied with albumin were classified as control group. The annual cumulative amount of albumin injections was also calculated. Patients in hypoalbuminemia group were further classified into two groups (≤13.8 g per year, >13.8 g per year; 13.8 g per year is the median amount of albumin supplementation) according to the amount of albumin they received. Severe hypoalbuminemia was defined as patients receiving albumin supplementation of 1,250 mg per year or more. The follow-up period of this study started from the date of a first diagnose of COPD (index date) to the date of the occurrence of ARF, attrition from NHI, or December 31, 2011, whichever came first.
Definitions of comorbidities
The occurrence of ARF was defined as diagnosis of ARF (ICD-9-CM code: 518.81) and use of invasive or noninvasive mechanical ventilations during hospitalization. Other potential confounding factors were also identified, including sociodemographic characteristics (ie, age, sex, occupation, and urbanization level of living area), comorbidities related to the risk of ARF (ie, end-stage renal disease [ESRD], diabetes mellitus, hypertension, ischemic heart disease [IHD], stroke, Parkinson’s disease, malignancies), and treatments such as use of steroid and blood transfusion. The occupations of patients were presented as four types according to the classification of beneficiaries in NHI; type I included civil servants, most employees, employers, and independently practicing professionals or technicians; type II included workers without particular employers or those who were self-employed, seamen or master mariners serving on foreign vessels; type III were mostly farmers and fishermen; type IV–VI mainly included members of low-income families, veterans and their families, and others. An index of the urbanization level of Taiwan’s townships, which was essentially developed for large-scale surveys in Taiwan, was applied in this study. ESRD and malignancies were identified as a patient registered in catastrophic illness database in NHIRD for dialysis (ICD-9-CM code: 585.xx) or for broad range of malignancies (ICD-9-CM codes: 140.xx–239.xx), respectively. Diabetes (ICD-9-CM code: 250.xx), hypertension (ICD-9-CM codes: 401.xx or 402.xx), IHD (ICD-9-CM codes: 410.xx–414.xx), stroke (ICD-9-CM codes: 430.xx–438.xx), and Parkinson’s disease (ICD-9-CM code: 232.xx) were identified if they were presented as diagnoses in patients’ outpatient records more than twice within the 365 days or at least once in inpatient records from index date to the end of follow-up. In addition, we also counted the annual number of ED visits and hospitalizations of study patients. The annual number of ED visits and hospitalizations were dichotomized by median. Use of steroid and blood transfusion were also identified by surveying the patients’ medication records in NHIRD.
Statistical analysis
Sociodemographic characteristics, comorbidities, and clinical procedures including medications were compared between albumin group and control group; similar comparisons were also performed between the group with and without development of ARF. Categorical variables were compared by using chi-square test, and continuous variables were compared by Student’s t-test. Cox proportional hazard regression model was performed to elucidate the associations of albumin supplementation and other risk factors with the risk of developing ARF. Univariable and multivariable regression analyzes were both performed to yield the crude hazard ratios (HRs), adjusted HRs, and their 95% of confidence intervals. Adjusted HR of albumin supplementation on the risk of ARF was estimated after adjustment for aforementioned risk factors including sociodemographic characteristics, comorbidities, use of steroid, receive of blood transfusion. Finally, a Cox regression analysis was further presented to delineate how the adjusted HR varied with the dose of albumin supplementation compared with those who had never been supplied with albumin. Data management and data analyzes were performed by using SAS/STAT® software, version 9.3 for Windows (SAS Institute Inc., Cary, NC, USA.).
Results
A total of 42,732 newly diagnosed COPD patients (57% male, mean age: 66 years) were enrolled in this study. Among them, 12.3% of the patients (n=5,248) developed ARF during the 6-year follow-up period.
The mean follow-up period of hypoalbuminemia group was 5.6 years, which was shorter than the control group (6.2 years). shows that patients with hypoalbuminemia were older and more likely to be male, have a type-III occupation (ie, farmers, fishermen, low-income family, veterans and families, and others), and live in less urbanized areas. They also had more chronic diseases (including diabetes, hypertension, IHD, stroke, Parkinson’s disease, and malignancies) and were more likely to receive treatments such as steroids and blood transfusion as compared with the control group. However, despite these differences, the crude mortality rates were similar between two groups.
Table 1 Demographic and clinical characteristics of COPD patients with and without hypoalbuminemia
presents the cumulative risk and crude HR of ARF for patients in different subgroups. In the univariable analysis, patients with hypoalbuminemia during the follow-up period were 5.35 times more likely to develop ARF than controls. Other covariates listed in were also associated with the risk of ARF.
Table 2 Demographic and clinical characteristics of COPD patients with (n=5,248) and without (n=37,484) developing ARF
Adjusted HR estimated in the multivariable Cox regression analysis is presented in . After adjustment for sociodemographic factors, comorbidities, treatment of steroid and blood transfusion, the HR of ARF related to hypoalbuminemia attenuated but was still statistical significant (AHR: 2.87 [95% CI: 2.65–3.10]). In addition, older age, male sex, treatment of steroid, less urbanized living areas, comorbid with ESRD, diabetes, Parkinson’s disease, and stroke were related to a higher risk of ARF; nevertheless, patients who were comorbid with hypertension, IHD, and malignancies and had received blood transfusion were less likely to develop ARF after adjustment for other risk factors.
Table 3 Adjusted hazard ratio of ARF related to patient’s characteristics
shows that adjusted HR of ARF increased with the annual average dose of albumin supplementation. If the average dose of albumin injection was lower than 13.8 g per year, the adjusted HR slightly increased to 1.69 (95% CI: 1.52–1.87). If the annual average dose was higher than 13.8 g per year, which was defined as severe hypoalbuminemia, the risk was even higher (AHR: 11.13, [95% CI: 10.35–11.98]) than no supplementation of albumin.
Discussion
To the best of our knowledge, this is the largest cohort of data concerning the risk of hypoalbuminemia in the development of ARF in patients with COPD. Our data showed that being elderly was the strongest independent risk factor for ARF (adjusted HR: 4.63, P<0.001), followed by hypoalbuminemia (adjusted HR: 2.87, P<0.001). However, as the annual average dose of albumin supplementation was higher than 13.8 g per year, which was defined as severe hypoalbuminemia, the risk for ARF was the highest (AHR:11.13, 95% CI: 10.35–11.98, P<0.001).
The outcome is poor when a COPD patient develops ARF during an AE.Citation18 Over one-third of patients died during hospitalizationCitation19 and survival is particularly reduced (50%) when mechanical ventilation is required.Citation18,Citation20 Furthermore, the long-term survival is still poor in patients receiving noninvasive ventilation, showing that the 5-year survival rate is only 23.7%.Citation21 Thus, the prevention of exacerbations or ARF is now recognized as a primary goal of maintenance therapy for COPD.Citation22 According to the Global Initiative for Chronic Obstructive Lung Disease guideline, vaccinations and several pharmacotherapies, such as long acting bronchodilators and inhaled corticosteroid, have been proved to be effective in the prevention of exacerbation of COPD.Citation23,Citation24 Nutrition has been the topic of extensive scientific research in COPD; however, clinical awareness of the impact of dietary habits and nutritional status on COPD progression and outcome is relatively limited.Citation25 Based on the findings of this study, we suggest that COPD patients should have a routine nutritional assessment and consultant once their diagnosis has been made. However, it may require further prospective study to verify whether albumin supplementation or nutritional support may reduce the risk of ARF in patients with COPD.
The prevalence and features of COPD patients with AE have been studied extensively,Citation26–Citation29 but the risk factors for ARF are poorly identified. In the current study, we showed that the comorbidities related to the risk of ARF included ESRD, diabetes mellitus, stroke, Parkinson’s disease and stroke, which is compatible with previous studies.Citation30 In addition, COPD patients requiring systemic steroid or blood transfusion represent more severe disease condition, which is reasonably associated with higher risks of ARF.Citation31,Citation32
Serum albumin level is one of the assessment tests for malnutrition in COPD.Citation33 However, few studies have focused on the role of serum albumin level as it relates to the development of ARF in COPD. There have been a number of studies investigating the association between albumin level and disease outcomes. For general hospitalized patients, lower serum albumin levels correlate with an increased risk of morbidity and mortality.Citation34 Hypoalbuminemia has also been shown as an important prognostic factor among a variety of diseases, such as severe sepsis, burns,Citation35 and regional enteritis (Crohn disease).Citation36 It is also associated with an increased risk of reintubation in postanesthetic general surgical patients.Citation37 In the current study, we confirmed that hypoalbuminemia is a strong risk factor for ARF in COPD.
This study had both strengths and limitations. Major strengths include the large number of COPD patients as well as a long follow-up period (average 6 years) in the NHIRD cohort. A limitation of the study is that information about COPD diagnosis was derived from ICD-9-CM and may not be completely accurate. Second, although we have adjusted the potential confounding factors and comorbidities related to the risk of ARF, the other confounding factors, such as body mass index, pulmonary function test were not available from this dataset. Third, the policy of albumin supplementation is offered by national health system in Taiwan, which limits the generalizability of such study to other health care systems.
In conclusion, hypoalbuminemia is a strong risk factor for ARF in patients with COPD. Severe hypoalbuminemia, which is defined as annual average dose of albumin supplementation higher than 13.8 g per year, is the strongest risk factor. Therefore, further prospective studies are needed to verify whether albumin supplementation or nutritional support may reduce the risk of ARF in patients with COPD.
Disclosure
The authors report no conflicts of interest in this work.
References
- ScholsAMSlangenJVolovicsLWoutersEFWeight loss is a reversible factor in the prognosis of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1998157179117979620907
- MaltaisFSimardAASimardCJobinJDesgagnésPLeBlancPOxidative capacity of the skeletal muscle and lactic acid kinetics during exercise in normal subjects and in patients with COPDAm J Respir Crit Care Med19961532882938542131
- Garcia-RioFMiravitllesMSorianoJBEPI-SCAN Steering CommitteeSystemic inflammation in chronic obstructive pulmonary disease: a population-based studyRespir Res2010116320500811
- AdamsPFMaranoMACurrent estimates from the National Health Interview Survey, 1994Vital Health Stat199510261520
- ManninoDMKirizVAChanging the burden of COPD mortalityInt J Chron Obstruct Pulmon Dis2006121923318046859
- MurrayCJLopezADMortality by cause for eight regions of the world: Global Burden of Disease StudyLancet1997349126912769142060
- BurgePSCalverleyPMJonesPWSpencerSAndersonJAMaslenTKRandomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trialBMJ20003201297130310807619
- WedzichaJASeemungalTACOPD exacerbations: defining their cause and preventionLancet200737078679617765528
- MacIntyreNHuangYCAcute exacerbations and respiratory failure in chronic obstructive pulmonary diseaseProc Am Thorac Soc2008553053518453367
- CalverleyPMRespiratory failure in chronic obstructive pulmonary diseaseEur Respir J Suppl20034726s30s14621114
- ConnorsAFJrDawsonNVThomasCOutcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to understand prognoses and preferences for outcomes and risks of treatments)Am J Respir Crit Care Med19961549599678887592
- QuinnellTGPilsworthSShneersonJMSmithIEProlonged invasive ventilation following acute ventilatory failure in COPD: weaning results, survival, and the role of noninvasive ventilationChest200612913313916424423
- DonBRKaysenGSerum albumin: relationship to inflammation and nutritionSemin Dial20041743243715660573
- HasegawaWYamauchiYYasunagaHFactors affecting mortality following emergency admission for chronic obstructive pulmonary diseaseBMC Pulm Med20141415125253449
- Haja MydinHMurphySClagueHSridharanKTaylorIKAnemia and performance status as prognostic markers in acute hypercapnic respiratory failure due to chronic obstructive pulmonary diseaseInt J Chron Obstruct Pulmon Dis2013815115723658480
- WangYStavemKDahlFAHumerfeltSHaugenTFactors associated with a prolonged length of stay after acute exacerbation of chronic obstructive pulmonary disease (AECOPD)Int J Chron Obstruct Pulmon Dis201499910524477272
- LaabanJPKouchakjiBDoreMFOrvoen-FrijaEDavidPRochemaureJNutritional status of patients with chronic obstructive pulmonary disease and acute respiratory failureChest1993103136213688486011
- Ai-PingCLeeKHLimTKIn-hospital and 5-year mortality of patients treated in the ICU for acute exacerbation of COPD: a retrospective studyChest200512851852416100133
- UcgunIMetintasMMoralHAlatasFYildirimHErginelSPredictors of hospital outcome and intubation in COPD patients admitted to the respiratory ICU for acute hypercapnic respiratory failureRespir Med2006100667415890508
- ChuCMChanVLLinAWWongIWLeungWSLaiCKReadmission rates and life threatening events in COPD survivors treated with non-invasive ventilation for acute hypercapnic respiratory failureThorax2004591020102515563699
- TitlestadILLassenATVestboJLong-term survival for COPD patients receiving noninvasive ventilation for acute respiratory failureInt J Chron Obstruct Pulmon Dis2013821521923650445
- AaronSDManagement and prevention of exacerbations of COPDBMJ2014349g523725245156
- PoolePJChackoEWood-BakerRWCatesCJInfluenza vaccine for patients with chronic obstructive pulmonary diseaseCochrane Database Syst Rev20002006CD00273311034751
- KarnerCChongJPoolePTiotropium versus placebo for chronic obstructive pulmonary diseaseCochrane Database Syst Rev20127CD00928522786525
- ScholsAMFerreiraIMFranssenFMNutritional assessment and therapy in COPD: a European Respiratory Society statementEur Respir J2014441504152025234804
- HurstJRDonaldsonGCWilkinsonTMPereraWRWedzichaJAEpidemiological relationships between the common cold and exacerbation frequency in COPDEur Respir J20052684685216264045
- WilkinsonTMHurstJRPereraWRWilksMDonaldsonGCWedzichaJAEffect of interactions between lower airway bacterial and rhinoviral infection in exacerbations of COPDChest200612931732416478847
- SapeyEStockleyRACOPD exacerbations. 2: aetiologyThorax20066125025816517585
- YangCYChenCJAir pollution and hospital admissions for chronic obstructive pulmonary disease in a subtropical city: Taipei, TaiwanJ Toxicol Environ Health A2007701214121917573635
- FunkGCBauerPBurghuberOCPrevalence and prognosis of COPD in critically ill patients between 1998 and 2008Eur Respir J20134179279923018915
- ZilberbergMDSternLSWiederkehrDPDoyleJJShorrAFAnemia, transfusions and hospital outcomes among critically ill patients on prolonged acute mechanical ventilation: a retrospective cohort studyCrit Care200812R6018442375
- CoteCZilberbergMDModySHDordellyLJCelliBHaemoglobin level and its clinical impact in a cohort of patients with COPDEur Respir J20072992392917251227
- GirónRMatesanzCGarcía-RíoFNutritional state during COPD exacerbation: clinical and prognostic implicationsAnn Nutr Metab200954525819252400
- Alonso MartinezJLAbinzano GuillénMLMartínez VelascoCGarcía MourizME[Morbidity and mortality among the hospitalized aged. Identification of prognostic factors]An Med Interna199512420424 Spanish8924545
- Aguayo-BecerraOATorres-GaribayCMacías-AmezcuaMDSerum albumin level as a risk factor for mortality in burn patientsClinics (Sao Paulo)20136894094523917657
- YangSSYuCSYoonYSYoonSNLimSBKimJCRisk factors for complications after bowel surgery in Korean patients with Crohn’s diseaseJ Korean Surg Soc20128314114822977760
- RujirojindakulPGeaterAFMcNeilEBRisk factors for reintubation in the post-anaesthetic care unit: a case-control studyBr J Anaesth201210963664222777658