 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
Exercise intolerance is a major issue affecting many people with COPD. Six-minute walking distance (6MWD) is a widely used indicator of exercise capacity in patients with COPD. The process is strenuous and time-consuming, especially for patients who have muscle wasting. Anthropometric indicators that reflect body lean mass, such as body mass index (BMI), mid-arm circumference (MAC), and calf circumference (CC), may have value in predicting exercise intolerance.
Purpose
This study attempted to determine the abilities of simple anthropometric indicators including BMI, MAC, and CC in reflecting the exercise intolerance of COPD patients.
Methods
We recruited 136 nonhospitalized ambulatory COPD patients without acute conditions from a general hospital in Taiwan. Each subject’s BMI, MAC, and CC were measured, and they were examined with pulmonary function tests and a 6-minute walk test.
Results
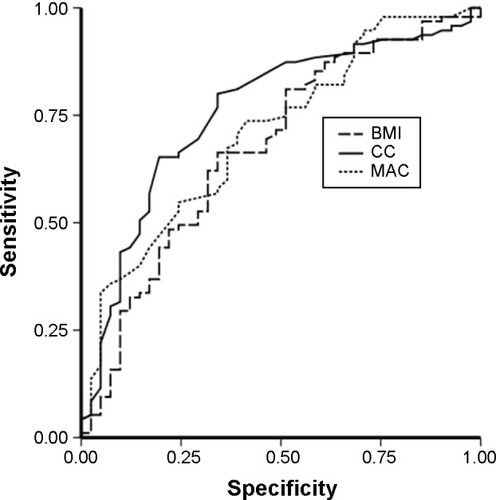
Among the three anthropometric indicators examined, CC showed the strongest correlation with the 6MWD, followed by MAC and BMI. CC was also strongly associated with functional capacity, followed by MAC, according to the receiver operating characteristic curves. CC and MAC, but not BMI, were significantly associated with exercise intolerance according to logistic regression models that controlled for potential confounders.
Conclusion
Among the three variables examined, CC and walking distance may have the strongest association in COPD patients. CC may have value in serving as an adjunct to 6MWD in evaluating exercise intolerance of patients with COPD.
Introduction
COPD is a major public health problem. In 2020, COPD is predicted to be the fifth leading cause of death in the world.Citation1 Exercise intolerance is a major disability in persons with COPD.Citation2,Citation3 The disease severely affects their ability to perform activities of daily living and their quality of life.Citation3,Citation4 The causes and mechanisms of exercise intolerance in these patients are complex and involve ventilator and respiratory mechanic impairments, gas exchange limitations, and muscle mass reductions in the extremities.Citation5 Thus, the ability to perform exercise is an important indicator of the severity of COPD, and an exercise test is an important component in routine clinical assessment of patients with this disease.
The 6-minute walk test (6MWT) is the most commonly used test for rating the functional capacity of persons with COPD. It is a reliable, valid, and responsive test measuring the functional exercise capacity of patients with COPD. To reduce the variability between test subjects and to improve the reproducibility in a given individual, the test standard specifies that the 6MWT must be conducted on a 30 m straight path.Citation6 The 6MWT measures four functional indicators: 6-minute walking distance (6MWD), self-perceived dyspnea, oxygen saturation, and heart rate.Citation7 Among these indicators, 6MWD is probably the most frequently used or studied. A 6MWD <350 m is often considered the threshold for poor prognosis.Citation8,Citation9
In addition to the 6MWT space consideration, we should also consider that older patients with severe COPD and dyspnea with exercise have some limitations. Some studies found that the exercise capacity of COPD patients is related to lung function as well as anthropometric indicators such as body mass index (BMI), fat-free mass index, and status of systemic inflammation.Citation10 The 6MWD and dyspnea Borg scores are associated with fat-free mass indexCitation11 and BMI and are positively associated with exercise capacity in COPD patients.Citation11,Citation12 In non-COPD elderly population, mid-arm circumference (MAC) and calf circumference (CC) have been observed to be better indicators of physical functional ability than BMI.Citation13 Bonnefoy et al have suggested that circumferences of the extremities may provide valuable information on muscle-related disabilities and physical functional capacity in these patients.Citation14 Recent studies have also shown that circumferences of the extremities, such as CC and MAC, might be better indicators of exercise capacity.Citation15,Citation16
However, the ability of these anthropometric indicators to reflect exercise capacity in COPD patients has not been examined. Thus, this study attempted to examine the anthropometric indicators and 6MWT in relation to the assessment of exercise capacity in patients with COPD.
Methods
Study design and patients
We conducted a cross-sectional study in persons with COPD who were recruited from the pulmonary outpatient unit of a medical center in northern Taiwan from November 2009 to August 2011. The diagnosis of COPD and the stage of the severity of the disease were based on the 2007 version of the Global Initiative for Chronic Obstructive Lung Disease guidelines.Citation2 COPD patients with a forced expiratory volume in 1 second (FEV1)/forced vital capacity ratio of <70% of the predicted value and aged 40–85 years were qualified to participate. Exclusion criteria included acute infection or acute exacerbation within 3 months prior to the study (no requirement for antibiotic or oral corticosteroid therapy and no change in respiratory symptoms), requirement for oxygen therapy during exercise (because these patients were different at baseline on the 6MWT), and severe systemic disease (malignancy, systemic lupus erythematosus, end-stage renal disease, and severe liver cirrhosis). A total of 136 patients (131 men and five women) were qualified and agreed to participate. All participants were ambulatory, in stable condition, and undergoing standard pharmacological treatment for COPD. The study protocol was approved by the Ethics Committee of the Chang-Gung Memorial Hospital (98-3601B and 100-0002C), and all subjects gave written informed consent before participating in the study.
Procedures and measurements
Each patient was interviewed face-to-face by well-trained researchers (Ho and Hsu) to elicit demographic, lifestyle, and disease-related data. The participants’ weight, height, MAC, and CC were measured, and all patients’ physical functional capacity was evaluated by a well-trained therapist (Ho or Chen) with the 6MWT and pulmonary function tests.
Weight, height, MAC, and CC were measured according to standard methods.Citation17 Body weight was measured to the nearest 0.1 kg with the subjects standing barefoot with light indoor clothing. Height was measured to the nearest 0.1 cm. BMI was calculated according to kg/m2. MAC and CC were measured to the nearest 0.1 cm with a flexible but non-stretching measuring tape.Citation17 MAC was measured at the midpoint of the nondominant arm (between the olecranon and acromion) and CC was measured at the largest point of the left calf in a sitting position.
Pulmonary function tests were performed with a Spiro-analyzer ST-250 (Fukuda Sangyo Co Ltd., Nagareyama City, Chiba, Japan) after a 10-minute rest. The best of at least three reproducible FEV1 and forced vital capacity values (with a difference within 200 mL or less than 5%) were used.
Exercise capacity was assessed with the 6MWT according to the American Thoracic Society guidelines. The scale was validatedCitation18 and shown to be reliableCitation19 in evaluating the exercise capacity of persons with COPD. All patients were instructed to walk as far as possible but were allowed to stop and rest during the test.Citation6 Oxygen saturation and pulse rate were recorded using a continuous finger-adapted pulse oximeter. Additionally, at the beginning and end of the 6MWT, the difference in exertion was assessed with the modified Borg scaleCitation20 by rating perceived exertion based on breathlessness. We used a ten-point scale with a nonlinear scaling scheme using descriptive terms to anchor responses, which is a commonly used format.Citation21
Statistical analysis
The results were statistically analyzed with SPSS for Windows 19.0 (SPSS Inc., Chicago, IL, USA). Descriptive data are expressed as the mean ± standard deviation or percentage. According to the Kolmogorov–Smirnov test, FEV1, MAC, and CC were normally distributed (P>0.20), but BMI and 6MWD were not normally distributed (P<0.05). Spearman’s correlation was used to evaluate the strength of the relationship between various anthropometric and pulmonary function indicators with the 6MWD. We used the sample size calculation for logistic regression with PASS 14 statistical software to retrospectively estimate the results of approximately 110 cases. The abilities of BMI, MAC, and CC in discriminating exercise capacity were analyzed with receiver operating characteristic (ROC) curves using the 6MWD (<350 m) as the reference standard. The areas under the curve (AUCs) of the ROC curves were determined. A larger AUC (maximum is 1) indicates better predictive ability. The association of BMI, MAC, and CC with the 6MWD was also analyzed with a multivariate logistic regression analysis. All models were controlled for possible confounders (age and FEV1). Statistical significance for all evaluations was set at α=0.05.
Results
shows the characteristics of the participants. The subjects averaged 72.4±7.5 years in age, 23.5±15.0 kg/m2 in BMI, 26.4±3.5 cm in MAC, and 32.9±3.5 cm in CC. Over half of the subjects had mild or moderate COPD, approximately 1/3 of the subjects (31.6%) had severe COPD, and only 16.9% of the subjects had very severe COPD. Approximately 2/3 of the subjects (95) had a 6MWD result of >350 m, and 41 of the subjects had a result of <350 m. The average O2 saturation was 95.25% at rest. The average Borg score was 0.85±1.3 at rest. The average heart rate was 90.5±16.7 bpm at rest.
Table 1 Characteristics of 136 patients with COPD
shows Spearman’s correlation coefficients of the anthropometric indicators (BMI, CC, and MAC) and FEV1 with 6MWD; all were significantly correlated with BMI (r=0.252, P<0.01), MAC (r=0.301, P<0.01), CC (r=0.426, P<0.01), and FEV1 (r=0.177, P<0.05). Similarly, the anthropometric indicators with FEV1 were all significantly correlated with BMI, MAC, and CC.
Table 2 Spearman’s correlation coefficients (r) of BMI, MAC, and CC with items in 6-minute walk distance and FEV1 of 136 patients with COPD
shows the logistic regression analysis of the association of various variables with 6MWD using 350 m as a threshold. Using a base model that controlled for age and FEV1, model I explained between 10.4% (Cox & Snell) and 14.7% (Nagelkerke) of the variance in 6MWD in patients with COPD. BMI (odds ratio [OR] =0.89, 95% confidence interval [CI] =0.79–1.00, P=0.050) did not show a significant association with impaired 6MWD. Model II explained between 14.1% (Cox & Snell) and 19.7% (Nagelkerke) of the variance in 6MWD in patients with COPD. MAC (OR =0.82, 95% CI =0.71–0.93, P=0.003) showed a significant association with impaired 6MWD. Model III explained between 16.3% (Cox & Snell) and 23.0% (Nagelkerke) of the variance in 6MWD in patients with COPD. CC (OR =0.79, 95% CI =0.68–0.90, P=0.001) showed a significant association with impaired 6MWD.
Table 3 Multivariate binary logistic regression analysis of the association of various variables with impaired 6MWD (<350 m) in 136 patients with COPD
shows the ability of BMI, MAC, and CC in differentiating impaired 6MWD (<350 m) with the ROC curves. The AUCs were 0.675 (0.514–0.776, P=0.001), 0.709 (0.616–0.802, P=0.000), and 0.758 (0.669–0.847, P=0.000) for BMI, MAC, and CC, respectively.
Figure 1 The receiver operating characteristic curves for BMI, MAC, and CC in persons with COPD, using 350 m of 6-minute-walking distance as the reference.
Abbreviations: BMI, body mass index; CC, calf circumference; MAC, mid-arm circumference.
Discussion
The results show that among the three anthropometric indicators examined, CC demonstrated the strongest association with the functional indicators, especially the 6MWD, compared to MAC and BMI. CC and MAC are the indicators that significantly predicted impaired 6MWD according to the regression analysis, and these factors may be capable to predict those with impaired 6MWD, according to the ROC analysis.
Association with exercise capacity
Enright et al established reference sex-specific equations to predict 6MWD in healthy adults: for men:
The 6MWD is reduced by several types of diseases, including obstructive lung disease, heart disease, and neuromuscular disease.Citation23 The determinants of poor 6MWD are complex and depend on both physical and psychological factors, and a poor 6MWD (<350 meters) result has prognostic value in identifying high-risk patients with COPD.Citation24 Therefore, in this study, we used the 6MWD (350 m) to define an impairment of functional capacity.
BMI has been demonstrated to influence walking distance in healthy subjects.Citation22 Previous studies have shown that patients with a low BMI have lower exercise capacity on submaximal and maximal exercise tests,Citation11,Citation25,Citation26 and that low BMI is an independent indicator of poor prognosis in persons with COPD. However, the present study showed that BMI is a much weaker indicator or functional indicator compared to MAC, particularly compared to CC in persons with COPD. Our finding confirms the findings of Ischaki et alCitation11 in which BMI was not effective in differentiating various COPD stages. Soler-Cataluña et alCitation27 also showed that in persons with COPD, mid-arm muscle area is a better predictor of mortality than BMI.Citation27 Villaça et alCitation28 found that an anthropometrically based method of estimating leg lean volume had high specificity and sensitivity in identifying peripheral muscle function in persons with depleted and nondepleted COPD. Patients with low leg lean volume had significantly lower exercise capacity and muscle performance than their normal counterparts. Lean body mass in legs has been observed to be a significant predictor of maximal exercise performance in patients with mild-to-moderate airflow limitation.Citation29
The predictive ability of MAC is not as strong as CC. This difference is probably because the degree of functional impairment between the upper and lower limbs is different in persons with COPD. Persons with COPD report more dyspnea during arm exercise compared to leg exercise.Citation30,Citation31 A major cause of dyspnea is dynamic hyperinflation, which is caused by airflow limitations as well as an increase in ventilation.Citation30,Citation32 Lower-limb muscles appear to be associated with muscle endurance and daily functional performance.Citation31
In the present study, BMI, MAC, and CC were all significantly correlated with FEV1. However, after adjusting for potential confounders, MAC and CC were not significantly associated with FEV1 in multivariate logistic regression models. Our results support the findings of others,Citation33–Citation35 suggesting that FEV1 is not independently associated with 6MWD in COPD.
Significance of CC in COPD
After controlling for age and FEV1, the results of three models using Nagelkerke measure of variance in 6MWD in patients with COPD were not high (0.147–0.23). However, in model III CC, R2 was higher than that in model II MAC and model I BMI. The results of the present study may be affected because some important factors were not included in the models. In the study by Britto et al approximately 62% of the variance was explained by sex, age, height, and change in heart rate during the test to predict the 6MWD in Brazilian subjects.Citation36 The present study suggests that CC is more effective than BMI or MAC in predicting exercise tolerance in persons with COPD. Lower-limb muscle atrophy is relatively common in persons with COPD, ranging from 21% to 45%, depending on the population and its operational definition.Citation37,Citation38 Muscle atrophy can even be found in persons with COPD with normal body weight.Citation37 Thus, it is conceivable that under some conditions, CC atrophy might be a factor limiting the exercise capability in persons with COPD. In non-COPD individuals, a larger CC is protective against physical functional decline.Citation39 CC is a pertinent nutritional marker compared to other anthropometric indicators.Citation40,Citation41
CC is a better indicator of body muscle mass because our legs contain over half of the muscle mass of the body and a decrease in walking activity can occur due to functional decline or long-term illness.Citation15 It is probable that long-term deconditioning could be caused by sedentary lifestyle in these patients as severe COPD is associated with greater dyspnea sensation and exercise-induced oxygen desaturation.Citation42
Taken together, the results of the present study indicate that CC is highly associated with exercise tolerance in persons with COPD and it might be of value in predicting exercise intolerance in these patients. CC is highly accessible and simple to measure.
Limitations of the study
This study has some limitations. First, the study sample size was small and participants were drawn from one hospital; therefore, the results may not reflect the entire spectrum of patients with COPD. Second, there was a disproportionate number of men compared to women in this study. The applicability of study results to female subjects requires further investigation. Third, the present study involves only ambulatory patients with COPD. The applicability of the study results to persons with more severe COPD requires further investigation. Finally, the study could also benefit from using more elaborate body-composition measuring techniques, such as dual radio-graph absorptiometry, to measure body lean mass.
Conclusion
The results suggest that among the three anthropometric indicators examined, CC is highly correlated with walking ability and can predict exercise capacity in persons with COPD. CC is accessible, non invasive, and easy to measure. It may serve as an alternative or adjunct to 6MWD in rating the physical functional capacity of persons with COPD.
Acknowledgments
The authors wish to thank the patients and personnel of the hospital unit for their cooperation during the course of this study. The study was supported by a grant from the Chang Gung Memorial Hospital (CMRPG391921), Ministry of Science and Technology (MOST 103-2314-B-038-066), and the Taipei Medical University (TMU102-AE1-B45 and 104TMU-SHH-24). All authors read and approved the final version of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- VestboJHurdSSAgustiAGGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med201318734736522878278
- RabeKFHurdSAnzuetoAGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med200717653255517507545
- BossenbroekLde GreefMHWempeJBKrijnenWPTen HackenNHDaily physical activity in patients with chronic obstructive pulmonary disease: a systematic reviewCOPD2011830631921728804
- van GestelAJClarenbachCFStowhasACPrevalence and prediction of exercise-induced oxygen desaturation in patients with chronic obstructive pulmonary diseaseRespiration201284535335922269699
- PepinVSaeyDLavioletteLMaltaisFExercise capacity in chronic obstructive pulmonary disease: mechanisms of limitationCOPD2007419520417729063
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function LaboratoriesATS statement: guidelines for the six-minute walk testAm J Respir Crit Care Med200216611111712091180
- EnrightPLThe six-minute walk testRespir Care20034878378512890299
- CoteCGCasanovaCMarinJMValidation and comparison of reference equations for the 6-min walk distance testEur Respir J20083157157817989117
- SpruitMAWatkinsMLEdwardsLDDeterminants of poor 6-min walking distance in patients with COPD: the ECLIPSE cohortRespir Med201010484985720471236
- HallinRJansonCArnardottirRHRelation between physical capacity, nutritional status and systemic inflammation in COPDClin Respir J2011513614221679348
- IschakiEPapatheodorouGGakiEPapaIKoulourisNLoukidesSBody mass and fat-free mass indices in COPD: relation with variables expressing disease severityChest200713216416917505043
- LanCCSuCPChouLLYangMCLimCSWuYKAssociation of body mass index with exercise cardiopulmonary responses in lung function-matched patients with chronic obstructive pulmonary diseaseHeart Lung20124137438122421506
- TsaiACLaiMCChangTLMid-arm and calf circumferences (MAC and CC) are better than body mass index (BMI) in predicting health status and mortality risk in institutionalized elderly TaiwaneseArch Gerontol Geriatr20125444344721663980
- BonnefoyMJauffretMJusotJFMuscle power of lower extremities in relation to functional ability and nutritional status in very elderly peopleJ Nutr Health Aging20071122322817508098
- ChumleaWCIs the MNA valid in different populations and across practice settings?J Nutr Health Aging200610524527 discussion 527–53317183424
- SanchezFFFaganelloMMTanniSEAnthropometric midarm measurements can detect systemic fat-free mass depletion in patients with chronic obstructive pulmonary diseaseBraz J Med Biol Res20114445345921590002
- LeeRDNiemanDCAssessment of the hospitalized patientNutritional Assessment3rd ed2003216250 Chapter 7LeaRDNiemanDCNew YorkMcGraw-Hill 2003
- ButlandRJPangJGrossERWoodcockAAGeddesDMTwo-, six-, and 12-minute walking tests in respiratory diseaseBr Med J (Clin Res Ed)198228416071608
- KervioGCarreFVilleNSReliability and intensity of the six-minute walk test in healthy elderly subjectsMed Sci Sports Exerc20033516917412544651
- American Thoracic SocietyAmerican College of Chest PhysiciansATS/ACCP Statement on cardiopulmonary exercise testingAm J Respir Crit Care Med200316721127712524257
- O’DonnellDEBreathlessness in patients with chronic airflow limitation. Mechanisms and managementChest19941069049128082376
- EnrightPLSherrillDLReference equations for the six-minute walk in healthy adultsAm J Respir Crit Care Med1998158138413879817683
- GuyattGHSullivanMJThompsonPJThe 6-minute walk: a new measure of exercise capacity in patients with chronic heart failureCan Med Assoc J19851329199233978515
- SpruitMAPolkeyMICelliBPredicting outcomes from 6-minute walk distance in chronic obstructive pulmonary diseaseJ Am Med Dir Assoc20121329129721778120
- CelliBRCoteCGMarinJMThe body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary diseaseN Engl J Med20043501005101214999112
- KobayashiAYonedaTYoshikawaMThe relation of fat-free mass to maximum exercise performance in patients with chronic obstructive pulmonary diseaseLung200017811912710773137
- Soler-CataluñaJJSánchez-SánchezLMartínez-GarcíaMASánchezPRSalcedoENavarroMMid-arm muscle area is a better predictor of mortality than body mass index in COPDChest20051282108211516236862
- VillaçaDSLerarioMCdal CorsoSClinical value of anthropometric estimates of leg lean volume in nutritionally depleted and non-depleted patients with chronic obstructive pulmonary diseaseBr J Nutr200810038038618184453
- YoshikawaMYonedaTTakenakaHDistribution of muscle mass and maximal exercise performance in patients with COPDChest2001119939811157589
- MartinezFJCouserJICelliBRRespiratory response to arm elevation in patients with chronic airflow obstructionAm Rev Respir Dis19911434764801900400
- MirandaEFMalagutiCCorsoSDPeripheral muscle dysfunction in COPD: lower limbs versus upper limbsJ Bras Pneumol201137380388 English, Portuguese21755195
- PortoEFCastroAAVellosoMNascimentoODal MasoFJardimJRExercises using the upper limbs hyperinflate COPD patients more than exercises using the lower limbs at the same metabolic demandMonaldi Arch Chest Dis200971212619522161
- WijkstraPJTenVergertEMvan der MarkTWRelation of lung function, maximal inspiratory pressure, dyspnoea, and quality of life with exercise capacity in patients with chronic obstructive pulmonary diseaseThorax1994494684728016768
- FoglioKCaroneMPaganiMBianchiLJonesPWAmbrosinoNPhysiological and symptom determinants of exercise performance in patients with chronic airway obstructionRespir Med20009425626310783937
- BauerleOChruschCAYounesMMechanisms by which COPD affects exercise toleranceAm J Respir Crit Care Med199815757689445279
- BrittoRRProbstVSde AndradeAFReference equations for the six-minute walk distance based on a Brazilian multicenter studyBraz J Phys Ther20131755656324271092
- VermeerenMACreutzbergECScholsAMPrevalence of nutritional depletion in a large out-patient population of patients with COPDRespir Med20061001349135516412624
- ScholsAMSoetersPBDingemansAMMostertRFrantzenPJWoutersEFPrevalence and characteristics of nutritional depletion in patients with stable COPD eligible for pulmonary rehabilitationAm Rev Respir Dis1993147115111568484624
- ReidKFNaumovaENCarabelloRJPhillipsEMFieldingRALower extremity muscle mass predicts functional performance in mobility-limited eldersJ Nutr Health Aging20081249349818615232
- BonnefoyMJauffretMKostkaTJusotJFUsefulness of calf circumference measurement in assessing the nutritional state of hospitalized elderly peopleGerontology20024816216911961370
- VellasBGuigozYBaumgartnerMGarryPJLauqueSAlbaredeJLRelationships between nutritional markers and the mini-nutritional assessment in 155 older personsJ Am Geriatr Soc2000481300130911037019
- JenkinsSČečinsNSix-minute walk test: observed adverse events and oxygen desaturation in a large cohort of patients with chronic lung diseaseIntern Med J20114141642220059599
