Abstract
Introduction
The measurement of C-reactive protein (CRP) to confirm the stability of COPD has been reported. However, CRP is a systemic inflammatory biomarker that is related to many other diseases.
Objective
The objective of this study is to discover a diagnostic biomarker for COPD.
Methods
Sixty-one subjects with COPD and 15 healthy controls (10 healthy non-smokers and 5 smokers) were recruited for a 1-year follow-up study. Data regarding the 1-year acute exacerbation frequency and changes in lung function were collected. CRP and the identified biomarkers were assessed in the validation COPD cohort patients and healthy subjects. Receiver operating characteristic values of CRP and the identified biomarkers were determined. A validation COPD cohort was used to reexamine the identified biomarker. Correlation of the biomarker with 1-year lung function decline was determined.
Results
Proteoglycan 4 (PRG4) was identified as a biomarker in COPD. The serum concentrations of PRG4 in COPD Global initiative for chronic Obstructive Lung Disease (GOLD) stages 1+2 and 3+4 were 10.29 ng/mL and 13.20 ng/mL, respectively; 4.99 ng/mL for healthy controls (P<0.05); and 4.49 ng/mL for healthy smokers (P<0.05). PRG4 was more sensitive and specific than CRP for confirming COPD severity and acute exacerbation frequency. There was no correlation between CRP and PRG4 levels, and PRG4 was negatively correlated with the 1-year change in predicted forced vital capacity percent (R2=0.91, P=0.013).
Conclusion
PRG4 may be a biomarker for identification of severity in COPD. It was related to the 1-year forced vital capacity decline in COPD patients.
Introduction
COPD is characterized by a progressive loss of lung function that is caused by consistent or repeated inflammatory responses in the lungs.Citation1 The pulmonary inflammation that occurs in small airways and pulmonary tissues often results in systemic inflammation.Citation1 COPD is heterogeneous, with wide variations in the rate of lung function decline, extent of emphysema, frequency of acute exacerbations (AEs), intensity of respiratory symptoms, and presence of systemic effects. C-reactive protein (CRP) is commonly used to assess several acute clinical conditions, including COPD.Citation2 However, CRP levels are elevated in many conditions,Citation3–Citation5 and the relevance of a high CRP level in a particular disease is often inadequately defined.
Proteoglycan 4 (PRG4) has several distinct biological functions, including immunoreactivity, cytoprotection, lubrication, and matrix binding.Citation6–Citation8 PRG4 is also expressed in many tissues/organs, including the lungs, heart, liver, bone, and cartilage,Citation8 and can be detected in blood and urine.Citation9,Citation10 Proteoglycans are produced by most eukaryotic cells, and they have many disease-related forms and functions in the human body.Citation11 For example, Hallgren et al observed that fibroblasts from COPD patients have alterations in proteoglycan production that could relate to the development of pulmonary disease.Citation12 Proteoglycans provide structural support and impart biomechanical properties to the lung tissue, and they are an important biological mediator in the regulation of lung inflammation, homeostasis, and wound healing.Citation13
This study identified and assessed the use of serum biomarkers compared with CRP to confirm COPD and AEs. We performed a comprehensive screening of protein profiles in healthy subjects and patients with Global initiative for chronic Obstructive Lung Disease (GOLD) stages 1, 2, 3, and 4 COPD using a proteomic approach. The identified protein candidates were determined in serum samples from two COPD groups for biomarker selection and validation. We also collected previous 1-year AE frequency and lung function data. The receiver operating characteristic (ROC) curve values of CRP and PRG4 and their correlation with 1-year lung function decline were determined.
Materials and methods
Ethics
The Ethics Committee of Taipei Medical University-Joint Institutional Review Board (Taipei, Taiwan) approved the study protocol. All subjects received written and oral information prior to inclusion and provided written informed consent.
Study population for biomarker selection
We examined 61 patients with COPD and 15 subjects without COPD in Shuang Ho Hospital (New Taipei City) in Taiwan between January 2013 and October 2014. All of the subjects were aged 40–80 years at the time of inclusion. Subjects with known cancer, active inflammatory disease (such as asthma, bronchiectasis, and other non-COPD-related disease), or an exacerbation during the 4 weeks prior to the study were not included. All of the patients with COPD received the diagnosis from a physician and exhibited a post-bronchodilation forced expiratory volume in the first second (FEV1)/forced vital capacity (FVC) ratio of <70%. Subjects without COPD exhibited an FEV1/FVC ratio of ≥75% and FEV1 ≥80% of the predicted value. Subjects who smoked at the time of recruitment were considered smokers (≥3 months of current smoking). Subjects who had never smoked were classified as nonsmokers.
Data collection
The study physician performed a physical examination of all participants and a clinical interview regarding smoking habits, AEs in the past year, comorbidities, and medical use. The classification of COPD severity followed the GOLD guidelines.Citation1 No subject had an AE (≤4 weeks) or had received oral corticosteroids (≥3 months) prior to the study, and all of the subjects continued with a stable regimen of medications throughout the study. Lung function parameters were assessed at the beginning of recruitment and at a 1-year follow-up visit using a Vitalograph Spirotac V™. Post-bronchodilation FEV1 and FVC were measured, and FEV1/FVC was calculated. Weight and height were measured using standard methods. Body weight was measured to the nearest 0.1 kg with the subjects standing barefoot and wearing light indoor clothing. Height was measured to the nearest 0.1 cm. BMI was calculated in kg/m2. Serum samples were obtained at a 1-year follow-up visit and stored at −80°C for laboratory measurements.
Protein digestion
Serum samples from five subjects in the same group were randomly selected and pooled together following protein digestion,Citation14 yielding the following samples: healthy controls and COPD GOLD stages 1, 2, 3, and 4. A detailed description of the protein digestion and preparation processes was provided previously.Citation15
Mass spectrometry and protein identification
Tryptic peptides were analyzed using a Thermo LTQ Orbitrap XL mass spectrometer (Thermo Fisher Scientific, Waltham, MA, USA) coupled with an Ultimate 3000 RSLC system (Dionex, Sunnyvale, CA, USA). The conditions for peptide separation and full mass spectrometry scans were reported previously.Citation15 The MS raw data were processed into peak lists using Proteome Discoverer 1.4 for Mascot database search with the National Center for Biotechnology Information and UniProt database prediction and a literature search.
Enzyme-linked immunosorbent assay
Enzyme-linked immunosorbent assays (ELISAs) determined the serum levels of CRP (PDCRP00; R&D Systems, Inc., Minneapolis, MN, USA) and PRG4 (MBS705095; MyBioSource, San Diego, CA, USA) according to the manufacturers’ instructions.
Study population for PRG4 validation
We examined 46 patients with COPD and 33 subjects without COPD in the same medical center in Taiwan between January 2014 and January 2015. All of the subjects were aged 40–80 years, and the same inclusion and exclusion criteria were used for this population as for the study population for biomarker selection. All of the patients with COPD received the diagnosis from a physician and exhibited a post-bronchodilation FEV1/FVC ratio of <70%. The subjects without COPD exhibited an FEV1/FVC ratio of ≥75% and FEV1 ≥80% of the predicted value. Serum samples were collected for PRG4 determination using ELISA.
Statistical analysis
The data are expressed as the means ± standard deviations. For comparisons among multiple values, one-way analysis of variance with Tukey’s post hoc test was used. ROC curve analysis was used to determine the specificity and sensitivity of CRP and PRG4 in COPD. The Youden index was used to determine cutoff values. Pearson’s correlation coefficient was used to examine the correlation of PRG4 with CRP. Linear regression was used to examine the correlation of the quintiles of CRP and PRG4 with a 1-year change in predicted FEV1%, FVC%, and FEV1/FVC%. Statistical analyses were performed using MedCalc statistical software version 15.2.2 (MedCalc Software bvba, Ostend, Belgium) for Windows. The level of significance was set to P<0.05.
Results
Characteristics of the study population for biomarker selection
Sixty-one subjects with COPD (19 for GOLD stages 1+2 and 42 for GOLD stages 3+4) were included, and ten healthy control and five healthy smoking volunteers were enrolled and followed-up for 1 year. Detailed baseline characteristics of the 76 subjects in the study population are presented in .
Table 1 Baseline characteristics of the healthy control subjects, healthy smokers, and COPD patients with GOLD stages 1+2 and 3+4 for the biomarker selection study population
Selection of potential biomarkers in patients with COPD
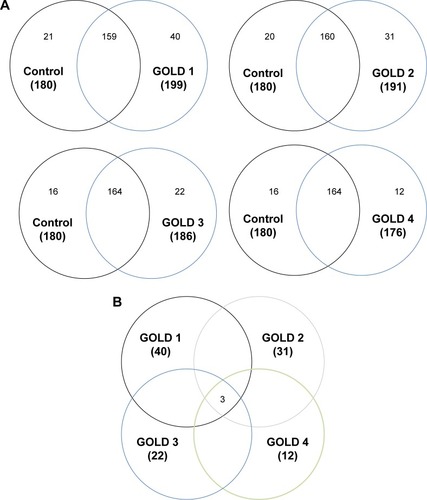
Overlaps in protein profiles between healthy controls and COPD GOLD stages 1, 2, 3, and 4 were compared to investigate protein expression in COPD (). A total of 180 proteins were identified in the healthy controls, and 199, 191, 186, and 176 proteins were identified in the patients with COPD GOLD stages 1, 2, 3, and 4, respectively (Table S1). A total of 40, 31, 22, and 12 proteins were unique to the patients with COPD GOLD stages 1, 2, 3, and 4, respectively. These unique proteins from patients with COPD GOLD stages 1, 2, 3, and 4 were further examined, and PRG4, type I cytoskeletal 16 keratin, and type II cytoskeletal 6A keratin were commonly present in the COPD serum samples ().
Serum levels of CRP and PRG4
There was no difference in CRP between the healthy controls (0.77±0.22 mg/L; 95% confidence interval [CI]: 0.50–1.14) and healthy smokers (1.06±0.67 mg/L; 95% CI: 0.23–1.89). Generally, the CRP levels of COPD GOLD stages 1+2 (4.36±5.33 mg/L, range 0.56–19.08 mg/L; 95% CI: −1.14–9.97) and 3+4 (5.20±4.62 mg/L, range 0.33–16.61 ng/mL; 95% CI: −2.36–14.29) were significantly higher than those of the healthy controls (P<0.05) (), but no significant difference in CRP was observed between the healthy smokers and the COPD patients with GOLD 1+2 and 3+4. The CRP levels in COPD patients with GOLD 3+4 were slightly higher than those in patients with GOLD 1+2, but the difference was not significant. Additionally, the CRP level was associated with COPD with a previous 1-year frequency of both AEs =0 and AEs ≥1 compared with healthy controls and smokers (). We observed that the levels of CRP in patients with COPD with AEs =0 and AEs ≥1 were 4.10±3.08 mg/L (range 0.64–9.77 mg/L; 95% CI: −0.39–8.22) and 6.02±7.07 ng/mL (range 0.33–19.08 ng/mL; 95% CI: −1.30–12.52), respectively, which were significantly higher than those in healthy controls (P<0.05). Only COPD patients with AEs =0 had higher CRP levels than healthy smokers (P<0.05). The CRP levels in COPD patients with GOLD stages 3+4 were slightly higher than those in patients with GOLD stages 1+2, but the difference was not significant.
Figure 2 CRP and PRG4 in COPD and COPD with AE.
Abbreviations: AE, acute exacerbation; GOLD, Global initiative for chronic Obstructive Lung Disease; CRP, C-reactive protein; PRG4, Proteoglycan 4.
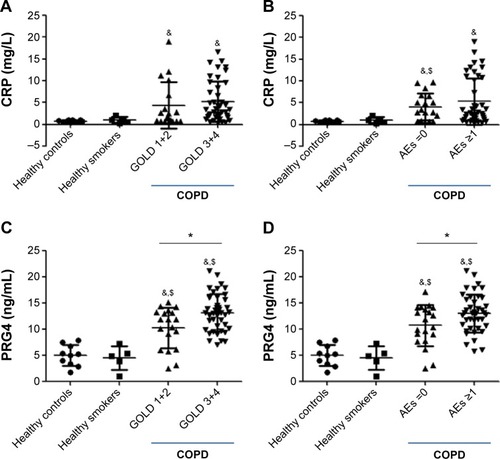
shows the PRG4 expression in COPD patients with GOLD stages 1+2 and 3+4 and healthy controls and smokers. There was no difference in PRG4 between the healthy control (4.99±2.01 ng/mL; 95% CI: 1.58–8.23) and healthy smoker (4.49±2.27 ng/mL; 95% CI: 1.67–7.31) groups. The PRG4 levels of COPD patients with GOLD stages 1+2 and 3+4 were significantly higher than those of the healthy control and healthy smoker groups (P<0.05), which were 10.29±3.86 ng/mL (range 2.5–15.2 ng/mL; 95% CI: 1.94–8.90) and 13.20±3.54 ng/mL (range 7.0–21.1 ng/mL; 95% CI: 6.49–8.74), respectively. The COPD GOLD stages 3+4 subjects had statistically higher levels of PRG4 compared with the COPD GOLD stages 1+2 subjects (P<0.05). PRG4 expression was divided into two AE-based groups (AEs =0 and AEs ≥1) of COPD patients, healthy controls, and smokers (). The PRG4 levels in COPD patients with AEs =0 and AEs ≥1 were significantly higher than those of the healthy control and smoker groups (P<0.05), which were 10.72±3.91 ng/mL (range 2.5–17.2 ng/mL; 95% CI: 12.03–14.49) and 13.07±3.64 ng/mL (range 5.8–21.1 ng/mL; 95% CI: 10.05–18.63), respectively. COPD patients with AEs ≥1 in the previous year had higher PRG4 levels compared with patients with AEs =0 (P<0.05).
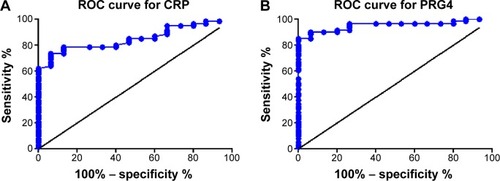
shows the ROC curve of the sensitivity and specificity of CRP and PRG4 levels for discriminating between the COPD and control groups. The area under the curve value for CRP was 0.850 (95% CI: 0.765–0.936, P<0.05), and the area under the curve for PRG4 was 0.953 (95% CI: 0.908–0.998, P<0.05). The PRG4 cutoff value determined by the Youden index for the control and COPD subjects was 7.892 ng/mL.
PRG4 validation for COPD
Forty-six subjects with COPD (30 for GOLD stages 1+2 and 16 for GOLD stages 3+4) and 33 healthy controls were enrolled in the PRG4 validation study for COPD. Detailed baseline characteristics of the 79 subjects in the study population are presented in . The PRG4 cutoff value of 7.892 ng/mL was used to validate the accuracy of COPD. The detailed diagnosis for the 79 subjects is presented in . The true negative and true positive rates were 0.79 and 0.93, respectively. The false negative rate and false positive rate were 0.17 and 0.09, respectively. Based on the validation populations, the accuracy of the 7.892 ng/mL PRG4 cutoff was 0.86 in the COPD subjects.
Table 2 Baseline characteristics of the healthy control subjects and COPD patients with GOLD stages 1+2 and 3+4 for the PRG4 validation study population
Table 3 PRG4 prediction of COPD in 79 subjects
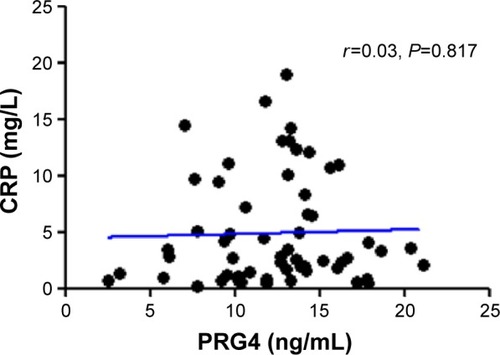
Correlation between CRP and PRG4
There was no statistical association between CRP and PRG4 in the COPD patients (r=0.03, P=0.817) (). The correlation analysis showed that PRG4 may not be related to systemic inflammation in patients with COPD.
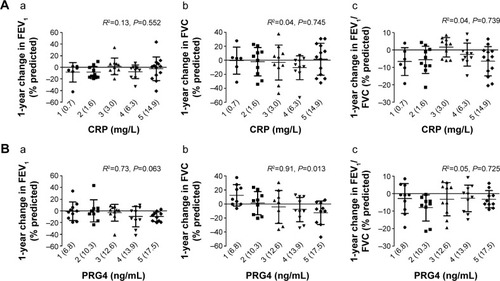
Correlation of CRP and PRG4 with lung function decline
There were no statistical correlations between CRP levels and 1-year changes in FEV1% (R2=0.13, P=0.552), FVC% (R2=0.04, P=0.745), or FEV1/FVC% of predictive values (R2=0.04, P=0.739) (). The 1-year change in predicted FEV1% decreased with an increase in PRG4 levels (), but this trend did not reach statistical significance (R2=0.73, P=0.063). Notably, we observed that the 1-year change in predicted FVC% was negatively correlated with the PRG4 level (R2=0.91, P=0.013). There was no correlation between 1-year changes in predicted FEV1/FVC% and PRG4 (R2=0.05, P=0.725).
Figure 5 The relationship of serum (A) CRP and (B) PRG4 levels to 1-year changes in predictive (a) FEV1%, (b) FVC%, and (c) FEV1/FVC% in COPD.
Abbreviations: FEV1, forced expiratory volume in the first second; FVC, forced vital capacity; CRP, C-reactive protein; PRG4, Proteoglycan 4.
Discussion
The present study examined biomarkers in the sera of COPD subjects using proteomic approaches. Three major findings are reported: 1) circulating PRG4 (cutoff value of 7.892 ng/mL) is a good biomarker for COPD; 2) PRG4 is a marker reflecting pulmonary inflammation in COPD; and 3) PRG4 relates to a 1-year FVC decline in COPD subjects.
The present study identified three biomarker candidates in the serum of healthy controls and in COPD patients with GOLD stages 1, 2, 3, and 4 from the biomarker population using a proteomics approach. Sample pooling is a strategy used to minimize individual variation in proteomic studies,Citation16 which can help overcome resource constraints when many individuals are analyzed. Type I cytoskeletal 16 keratin and type II cytoskeletal 6A keratin are associated with epithelial tissues from the nail beds, the esophagus, the tongue, and the hair follicles,Citation17,Citation18 which are less likely related to the mechanisms of COPD. Consequently, PRG4 was the best potential candidate for a COPD biomarker in the present study. The systemic biomarker CRP was selected as a basis for comparing the PRG4. The COPD subjects had very high levels of CRP in serum samples, but no significant difference was observed when we classified the COPD levels as GOLD stages 1+2 and 3+4 in our study. Notably, we observed a very good relationship between serum PRG4 levels and COPD. The subjects in the GOLD stages 3+4 group had significantly higher PRG4 levels than the subjects in the GOLD stages 1+2 group. Therefore, PRG4 may differentiate severity in COPD patients, and it can be used to identify COPD severity. A previous study has suggested that CRP is a biomarker for AEs in COPD.Citation2 Indeed, we found that CRP levels in patients with COPD with AEs ≥1 were higher than those in COPD patients with AEs =0 and in normal subjects. However, CRP levels in a portion of our COPD patients with AEs ≥1 remained similar to those of COPD patients with AEs =0. We found that the COPD subjects with at least one AE had higher PRG4 levels compared with the subjects without AEs, which suggests that an increase in serum PRG4 levels may increase the risk of AEs in patients with COPD.
Increasing efforts are being made in the search for COPD biomarkers.Citation19 Eagan et al showed that the plasma levels of neutrophil gelatinase-associated lipocalin are significantly higher in COPD patients compared with healthy control subjects.Citation20 Hurst et al identified 36 plasma biomarkers in pairs of stable and exacerbated states from 90 COPD patients.Citation21 These authors suggested that CRP was the major biomarker that confirmed COPD exacerbation severity. In the present study, the ROC curve value of PRG4 (area under the curve 0.958) for COPD was much higher than that of CRP (area under the curve 0.8503 from the present study and 0.66 referenced from Eagan et alCitation20) and neutrophil gelatinase-associated lipocalin (area under the curve 0.677).Citation20 These comparisons suggest that PRG4 is a potentially sensitive and specific biomarker for COPD. To confirm that PRG4 is a good biomarker for COPD, we recruited the second study population to validate the PRG4 cutoff value derived from the first population (biomarker selection). The accuracy in the validation population was 0.86, with a false negative rate of 0.17 and a false positive rate of 0.09, suggesting that circulating PRG4 can discriminate between COPD patients and mainly nonsmoking controls.
Altered chronic inflammation in patients with COPD results from repeated injury and repair and an increased number of inflammatory cell types in the airways, lung parenchyma, and pulmonary vasculature. Systemic CRP was compared with PRG4 to evaluate the specific value of PRG4 in patients with COPD. The results showed no correlation between CRP and PRG4, which means that PRG4 may not be involved in the systemic inflammation observed in patients with COPD. Inflammatory responses and a narrowing of peripheral airways lead to reduced FEV1. Parenchymal destruction resulting from emphysema contributes to airflow limitations.Citation22 PRG4 was related to 1-year lung function decline values, including 1-year changes in FEV1%, FVC%, and FEV1/FVC% of predicted values. Notably, we found that a 1-year change in the FVC% of predicted value was significantly correlated with PRG4 in the COPD patients. This finding implies that PRG4 is a potential biomarker reflecting pulmonary inflammation. However, more evidence is required to verify this correlation.
Breathing is powered by the muscles of the chest wall and the diaphragm, which is the strong muscle that separates the chest from the abdomen. The hallmark of COPD is narrowed bronchial tubes. The lung muscle requires more force to exhale through narrow airways to gain stable oxygen, and the air sacs become hyperinflated (ie, filled with too much air) in emphysema. Repeated high-intensity muscular loading reduces PRG4 concentrations.Citation7 The difficulty of muscle movement during breathing could be associated with lung function decline in COPD patients. Additionally, long-term corticosteroid inhalation partially modulated the pulmonary composition of the extracellular matrix, affecting, for example, the level of proteoglycan in moderate-to-severe COPD.Citation23 The PRG4 that is lost from the lungs could be transported to the circulatory system and detected as a potential biomarker for COPD. Additionally, PRG4 has been linked to cytokine regulation (IL-1 and TNF-α) and growth factors (IGF and TGF-β),Citation6 which suggests that PRG4 could be associated with pulmonary inflammation. However, further work should be undertaken to investigate the roles of PRG4 in pulmonary inflammation.
Conclusion
Serum PRG4 is an important biomarker for supporting the COPD diagnosis and relates to the decline in lung function in patients with COPD. Additionally, serum PRG4 is independently related to COPD without systemic oxidative and inflammatory responses. Notably, previous reports showed that the majority of COPD subjects in Taiwan are men (~95%),Citation24,Citation25 which is consistent with our study. The sex difference should be extrapolated to women with caution. Also, the sample size in the present study was relatively small, particularly in controls. Other lung functions and age-related difference should be discussed in the future. Future in vitro and in vivo studies in humans will provide a greater understanding of the mechanistic principles underlying PRG4 during COPD and novel insights into the role of PRG4 in this devastating disease.
Author contributions
All authors contributed substantially to the concept and design of the study, the drafting of the article, and the critical revision of the manuscript for important intellectual content. All authors have read and approved the final version of the paper for publication.
Acknowledgments
This study was funded by the Ministry of Science and Technology of Taiwan (MOST103-2314-B-038-018, MOST103-2314-B-038-066, and MOST102-2314-B-038-055-MY2) and Taipei Medical University (TMU102-AE1-B45).
Disclosure
The authors report no conflicts of interest in this work.
References
- VestboJHurdSSAgustíAGGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med201318734736522878278
- ThomsenMIngebrigtsenTSMarottJLInflammatory biomarkers and exacerbations in chronic obstructive pulmonary diseaseJAMA20133092353236123757083
- AgassandianMShurinGVMaYShurinMRC-reactive protein and lung diseasesInt J Biochem Cell Biol201453778824853773
- PalaniyarNNadesalingamJReidKBPulmonary innate immune proteins and receptors that interact with gram-positive bacterial ligandsImmunobiology200220557559412396017
- Zbroja-SontagWDefense proteins and immune complexes in the blood serum of women with inflammatory and neoplastic lesions of the ovaryAm J Reprod Immunol1983411206194700
- ReesSGDaviesJRTudorDImmunolocalisation and expression of proteoglycan 4 (cartilage superficial zone proteoglycan) in tendonMatrix Biol20022159360212475643
- AbusaraZKrawetzRSteeleBDuVallMSchmidtTHerzogWMuscular loading of joints triggers cellular secretion of PRG4 into the joint fluidJ Biomech2013461225123023506642
- IkegawaSSanoMKoshizukaYNakamuraYIsolation, characterization and mapping of the mouse and human PRG4 (proteoglycan 4) genesCytogenet Cell Genet20009029129711124536
- LiuYJLuSHXuBHemangiopoietin, a novel human growth factor for the primitive cells of both hematopoietic and endothelial cell lineagesBlood20041034449445614976050
- SuJLSchumacherBLLindleyKMDetection of superficial zone protein in human and animal body fluids by cross-species monoclonal antibodies specific to superficial zone proteinHybridoma20012014915711461663
- HardinghamTEFosangAJProteoglycans: many forms and many functionsFASEB J199268618701740236
- HallgrenONihlbergKDahlbäckMAltered fibroblast proteoglycan production in COPDRespir Res2010115520459817
- FrevertCWSannesPLMatrix proteoglycans as effector molecules for epithelial cell functionEur Respir Rev200514137144
- YuCJWangCLWangCIComprehensive proteome analysis of malignant pleural effusion for lung cancer biomarker discovery by using multidimensional protein identification technologyJ Proteome Res2011104671468221806062
- SuCLChenTTChangCCTaiwan CardioPulmonary Research Group (T-CPR)Comparative proteomics of inhaled silver nanoparticles in healthy and allergen provoked miceInt J Nanomedicine201382783279923946650
- DizAPTruebanoMSkibinskiDOThe consequences of sample pooling in proteomics: an empirical studyElectrophoresis2009302967297519676090
- RosenbergMFuchsELe BeauMMEddyRLShowsTBThree epidermal and one simple epithelial type II keratin genes map to human chromosome 12Cytogenet Cell Genet19915733381713141
- SchweizerJBowdenPECoulombePANew consensus nomenclature for mammalian keratinsJ Cell Biol200617416917416831889
- SinDDHollanderZDeMarcoMLMcManusBMNgRTBiomarker development for COPD: from discovery to clinical implementationAm J Respir Crit Care Med Epub2015715
- EaganTMDamåsJKUelandTNeutrophil gelatinase-associated lipocalin: a biomarker in COPDChest201013888889520495108
- HurstJRDonaldsonGCPereraWRUse of plasma biomarkers at exacerbation of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med200617486787416799074
- HoggJCChuFUtokaparchSThe nature of small-airway obstruction in chronic obstructive pulmonary diseaseN Engl J Med20043502645265315215480
- KunzLIStrebusJBudulacSEGLUCOLD (Groningen Leiden Universities Corticosteroids in Obstructive Lung Disease) Study GroupInhaled steroids modulate extracellular matrix composition in bronchial biopsies of COPD patients: a randomized, controlled trialPLoS One20138e6343023667615
- AhamedMAlhadlaqHANickel nanoparticle-induced dose-dependent cyto-genotoxicity in human breast carcinoma MCF-7 cellsOnco Targets Ther2014726928024627639
- ChenCZWangLYOuCYLeeCHLinCCHsiueTRUsing cluster analysis to identify phenotypes and validation of mortality in men with COPDLung201419288989625288484