Dear editor
We read the article by Porpodis et alCitation1 with great interest. In this study, the authors have evaluated the effect of roflumilast on the phagocytic activity of systemic phagocytes in severe and very severe COPD patients by measuring the oxidative burst post-bacterial stimulation. The study group for this study involved 21 severe or very severe COPD patients who were administered roflumilast in addition to other COPD treatments such as long-acting beta-adrenoceptor agonists (LABA) + inhaled corticosteroids (ICS) + long-acting anti-muscarinic agent (LAMA) or ICS + LABA.
Prior animal studies have reported that ICS impairs Klebsiella pneumoniae phagocytosis and decreases oxidative stress post-infection with bacteria.Citation2 It would have been interesting to know the phagocytic efficacy of roflumilast in combination with other therapeutic drugs for instance, whether the phagocytic efficacy of the combination of roflumilast and ICS is more as compared to other combinations. This could have been possibly achieved by dividing the study group into subgroups such as ICS + roflumilast or LABA + roflumilast or LAMA + roflumilast or ICS + LABA + roflumilast. Porpodis et alCitation1 also reported that roflumilast increases phagocytic activity, and this anti-inflammatory effect contributes toward increase in lung function parameters among COPD subjects.Citation3 Previous studies have reported that ICS + LABA or ICS + LABA + LAMA improves the lung function. However, in this study there is no control group (group without roflumilast treatment) therefore, the improvement seen in lung function could be a combined effect of ICS + LABA, ICS + LABA + LAMA and roflumilast and not roflumilast alone.
Additionally, it would have been interesting to know whether increase in phagocytosis by roflumilast can contribute toward improvement of exacerbations. It has been reported by Calverley et alCitation4 that roflumilast decreases exacerbations among mild to moderate COPD patients, but there are no data available with reference to severe COPD patients. Lastly, the authors should have presented the lung function data in terms of actual values along with the percent predicted format, this would have made the results easy to comprehend.
Disclosure
The authors have no conflicts of interest to disclose.
Disclosure
The authors have no conflicts of interest to disclose.
Dear editor
We chose outpatients from our clinic who were stable for at least a month. Seven days before roflumilast treatment these patients were monitored more frequently. They all had a history of exacerbations but no one was recovering from an acute exacerbation.
We included a table with patients’ characteristics (). No patient was taking oral steroids during the study period. Patients were treated according to TORCH (Towards a Revolution in Chronic Obstructive Pulmonary Disease Health) and UPLIFT (Understanding Potential Long-term Impacts on Function with Tiotropium) studies. Our hypothesis was that the addition of an anti-inflammatory regimen such as roflumilast, in patients who experience frequent exacerbations, would have beneficial influence on lung function and exacerbations. This is the only way to be sure that the PDE-4 inhibitor induces phagocytic activity and to what degree. If an oral corticosteroid had been used we would not be sure if PDE-4 would assist in the treatment of an exacerbations. Due to the small number of patients, statistical analysis by subgrouping the patients was not possible. Every patient was a control to himself and every spirometry value or phagocytic activity was compared to the first values before roflumilast treatment. Our study is an on-going pilot study. Although COPD care has improved over the last decade,Citation1 there is still a huge unmet burden of disease. Exacerbations in particular can be distressing for patientsCitation2 and have serious consequences on their long-term health, such as increased disease progression,Citation3 increased risk of cardiovascular events,Citation4 and increased mortality rates.Citation5,Citation6 Roflumilast is an oral PDE-4 inhibitor that targets inflammatory cells involved in triggering COPD exacerbations. It includes the only PDE-4 inhibitor approved by the US Food and Drug Administration and is available in 500 μg tablets to be administered once daily. As stated in our publication although this was a small study, the anti-inflammatory activity of roflumilast was shown to provide incremental benefits on top of existing therapies. Future randomized studies will further confirm the impact of roflumilast on COPD and beyond. The authors believe that the lung function values would not clearly present the changes and therefore we chose to present this information with the variability of the values ().
Table 1 Patients’ characteristics
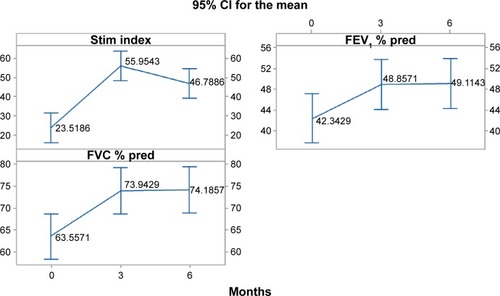
Figure 1 Mean change of stimulation index (phagocytic activity), FEV1 % predicted, FVC % predicted, per indicated periods (0: before receiving roflumilast, 3 months and 6 months after).
Abbreviations: pred, predicted; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; CI, confidence interval; stim, stimulation.
References
- AlmagroPSalvadoMGarcia-VidalCRecent improvement in long-term survival after a COPD hospitalisationThorax201065429830220388752
- KesslerRStahlEVogelmeierCPatient understanding, detection, and experience of COPD exacerbations: an observational, interview-based studyChest2006130113314216840393
- DecramerMCooperCBTreatment of COPD: the sooner the better?Thorax201065983784120805184
- DonaldsonGCHurstJRSmithCJHubbardRBWedzichaJAIncreased risk of myocardial infarction and stroke following exacerbation of COPDChest201013751091109720022970
- WedzichaJASeemungalTACOPD exacerbations: defining their cause and preventionLancet2007370958978679617765528
- Soler-CatalunaJJMartinez-GarciaMARoman SanchezPSalcedoENavarroMOchandoRSevere acute exacerbations and mortality in patients with chronic obstructive pulmonary diseaseThorax2005601192593116055622
