Abstract
Purpose
Acute COPD exacerbations account for much of the rising disability and costs associated with COPD, but data on predictive risk factors are limited. The goal of the current study was to develop a robust, clinically based model to predict frequent exacerbation risk.
Patients and methods
Patients identified from the Optimum Patient Care Research Database (OPCRD) with a diagnostic code for COPD and a forced expiratory volume in 1 second/forced vital capacity ratio <0.7 were included in this historical follow-up study if they were ≥40 years old and had data encompassing the year before (predictor year) and year after (outcome year) study index date. The data set contained potential risk factors including demographic, clinical, and comorbid variables. Following univariable analysis, predictors of two or more exacerbations were fed into a stepwise multivariable logistic regression. Sensitivity analyses were conducted for subpopulations of patients without any asthma diagnosis ever and those with questionnaire data on symptoms and smoking pack-years. The full predictive model was validated against 1 year of prospective OPCRD data.
Results
The full data set contained 16,565 patients (53% male, median age 70 years), including 9,393 patients without any recorded asthma and 3,713 patients with questionnaire data. The full model retained eleven variables that significantly predicted two or more exacerbations, of which the number of exacerbations in the preceding year had the strongest association; others included height, age, forced expiratory volume in 1 second, and several comorbid conditions. Significant predictors not previously identified included eosinophilia and COPD Assessment Test score. The predictive ability of the full model (C statistic 0.751) changed little when applied to the validation data set (n=2,713; C statistic 0.735). Results of the sensitivity analyses supported the main findings.
Conclusion
Patients at risk of exacerbation can be identified from routinely available, computerized primary care data. Further study is needed to validate the model in other patient populations.
Keywords:
Introduction
COPD is a serious, debilitating condition that has become a major public health concern and by 2020 is projected to rank fifth in global burden of disease and third in global mortality.Citation1 For a proportion of patients, COPD is a progressive disease characterized by periodic acute exacerbations of symptoms. These exacerbations pose an immediate threat to patients and also hasten progression of the disease. Exacerbations accelerate decline of lung function, so that patients often fail to return to baseline levels. Although symptoms may last a few days, recovery of lung function can take weeks to months, resulting in prolonged periods of functional limitation and general worsening of quality of life, often with some degree of permanent functional decline. Exacerbations are also associated with substantial risk of hospitalization and death, as well as considerable economic costs that increase with exacerbation frequency.Citation1,Citation2
Preventing exacerbations is therefore a key goal of COPD managementCitation1,Citation3–Citation5 and hence the need to predict who are likely to experience exacerbations. The recent Global Initiative for Chronic Obstructive Lung Disease (GOLD) categories A–D were developed to aid in assessing future risk of exacerbations and performed well in one study;Citation6,Citation7 however, patient assignment to categories may vary depending on the choice of symptom measure, limiting their applicability.Citation8 Indices of COPD severity such as the body mass index [BMI], obstruction, dyspnea, and exercise (BODE) index and the age, dyspnea, and obstruction (ADO) index have been used to try to predict future exacerbations among patients with COPD but with only moderate (60%–70%) prediction success; moreover, they require specific data (eg, 6-minute walk test) that may not be routinely available.Citation9,Citation10 The dyspnea, airflow obstruction, smoking status, and exacerbation frequency (DOSE) index has been shown to predict future exacerbations in a large primary care data set, and the index was stronger than previous exacerbation frequency or the ADO or BODE index.Citation9,Citation11,Citation12 Other researchers have developed de novo statistical models to identify independent clinical predictors. However, many of these studies included relatively small sample sizes,Citation10,Citation13–Citation16 patients with severe COPD,Citation14,Citation17,Citation18 and/or severe outcomes such as hospitalization or death.Citation13,Citation15,Citation17,Citation19–Citation22
The goal of the current study was to develop a robust, clinically based predictive model that would encompass all levels of COPD severity as well as moderate or severe exacerbation severity. Such a model could help in earlier targeting of patients for review to optimize drug therapy and other interventions, with the aim of reducing hospital admissions, decline in lung function, and the morbidity and mortality associated with COPD. A secondary objective was to compare the model’s predictive value in relation to existing predictive tools.
Patients and methods
This was a historical follow-up study of patients with COPD identified from the Optimum Patient Care Research Database (OPCRD).Citation23 The OPCRD is a quality-controlled, longitudinal, respiratory-focused database containing anonymous data from general practices in the UK and has been approved by the Trent Multicentre Research Ethics Committee for clinical research use (approval reference 10/H0405/3), and this study was approved by the Anonymised Data Ethics Protocols and Transparency committee, the independent scientific advisory committee for the OPCRD. Informed consent was not required or possible as we worked with anonymous data, and this was not an interventional study. However, patients could opt out of having their data used in research. At the time of the study, the OPCRD contained records of >50,000 patients with COPD from >300 UK general practices. The database combines routine data from electronic patient records with linked patient-reported data collected using disease-specific questionnaires. Routine clinical data, including patient demographic characteristics, comorbidities, exacerbation history, modified Medical Research Council (mMRC) score,Citation24 and current therapy, were extracted from primary care practice management systems. In addition, a proportion of patients with relevant disease codes were invited to complete validated disease assessment questionnaires, sent via a secure mailing house. The questionnaires enabled calculation of the mMRC scores and the COPD Assessment Test (CAT) scores.Citation25
The current study was divided into model-building and model-validation components. Patients were eligible for inclusion in the model-building phase if, on or before March 12, 2013, they had at least one recorded eosinophil count, were at least 40 years of age, had been diagnostically coded for COPD, and had a forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC) ratio <0.7 recorded within 5 years of their last eosinophil count (defined as the index date). All eligible patients needed to have at least 1 year of observation before (baseline year) and 1 year after (outcome year) the index date. Included patients also needed to have complete data on the candidate predictors analyzed. Those with chronic respiratory diseases other than asthma, such as bronchiectasis, were excluded. The validation cohort consisted of patients with similar eligibility criteria identified between March 2013 and February 2014.
Potentially important variables within the OPCRD were identified from a search of the literature and from expert opinion of the authors:
Sociodemographic factors: sex, age, height, weight, BMI, smoking status
Symptom severity: mMRC dyspnea score, CAT score, number of exacerbations in the previous year
Comorbidities: asthma, eczema, allergic or nonallergic rhinitis, nasal polyps, diabetes mellitus, gastroesophageal reflux disease (GERD), ischemic heart disease, heart failure, anxiety/depression, Charlson comorbidity index
Spirometry: FEV1 (% predicted), FEV1/FVC ratio
Peripheral blood eosinophilia (defined as ≥500 cells/μL).
Model building
To enhance diagnostic specificity and to be consistent with earlier research, as well as with the GOLD cut-point for risk of future events,Citation7 we defined the outcome of interest as frequent (≥2) exacerbations. Exacerbations were defined as either 1) unscheduled hospital admission or accident/emergency attendance for COPD or lower respiratory events, 2) an acute course of oral corticosteroids prescribed with evidence of respiratory review, or 3) antibiotics prescribed with evidence of respiratory review. Where one or more oral corticosteroid course, hospitalization, or antibiotic prescription occurred within a 2-week window, these events were considered to be the result of the same exacerbation.
All analyses were performed using the R statistical package (version 3.0.2). Prior to analysis, continuous variables were evaluated via likelihood ratio test to see if quadratic or cubic transformation improved model fit. Akaike information criteria (AIC) were compared to test whether model fit was improved by categorical or continuous classification.
Univariable logistic regressions were performed to gauge the importance of individual variables and to help define the best form (eg, continuous, categorical) of each variable. However, all potentially important variables were fed into a multiple logistic regression with backward selection of the model having the lowest AIC. The questionnaire variables dealing with symptoms and pack-years were excluded from this analysis owing to small sample size.
By way of sensitivity analysis, the model-building process was repeated for two different subpopulations. Sub-population 1 consisted of all patients without an overlapping diagnosis of asthma, defining asthma using the sensitive definition of any asthma-related Read code at any time in the data set. The second, smaller subpopulation consisted of those with questionnaire information on symptoms (CAT and mMRC score) and pack-years of smoking.
Model validation
Calibration plots were performed by comparing observed with predicted risk among 150 groups of ~110 patients each. Goodness of fit was judged using both the C statistic (area under the curve) and the Hosmer–Lemeshow test.Citation26 The C statistic confidence intervals (CIs) were generated by bootstrapping. External validity was judged by the C statistic when the full multivariable model was applied to the validation cohort.
In addition, we assessed the predictive accuracy of the model to predict two or more exacerbations compared with the DOSE index and GOLD categories A–D using the mMRC, together with exacerbations and FEV1, to assign categories.Citation7
Results
Approximately 51,000 patients with COPD were identified from the OPCRD; 16,565 met all inclusion criteria. The main reasons for exclusion from the study are depicted in . The study index dates (ie, dates of last eosinophil count) ranged from 1993 to 2012 (median year, 2009; interquartile range, 2007–2010).
Figure 1 Patient selection in the database.
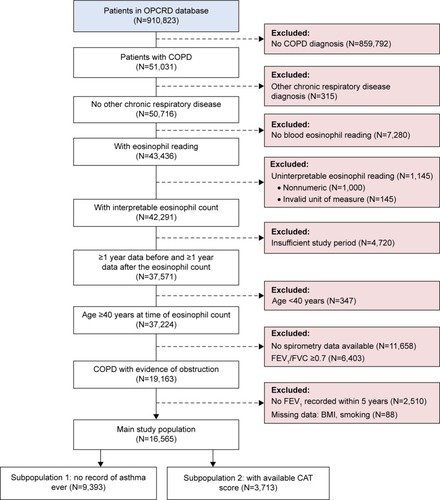
Of the 16,565 patients included in the full population, 9,393 did not have any recorded asthma Read code at any time (subpopulation 1) and 3,713 had questionnaire data for determining CAT score (subpopulation 2). The characteristics of these three populations () and the frequencies of COPD exacerbations () were similar, with only minor differences. Most patients had moderate COPD, and 92% of lung function measurements were taken within 2 years of the index date (80% within 1 year).
Table 1 Baseline characteristics of all patients and of the two subpopulations
Table 2 Number of exacerbations in baseline and outcome years
Patient numbers for the categorized mMRC and DOSE index scores and for GOLD category are in Table S1.
Approximately 20% of the total population had two or more exacerbations in the outcome year (). Most variables were significant univariable predictors ().
Table 3 Univariable predictors of two or more COPD exacerbations in the outcome year in the total population data set (N=16,565)
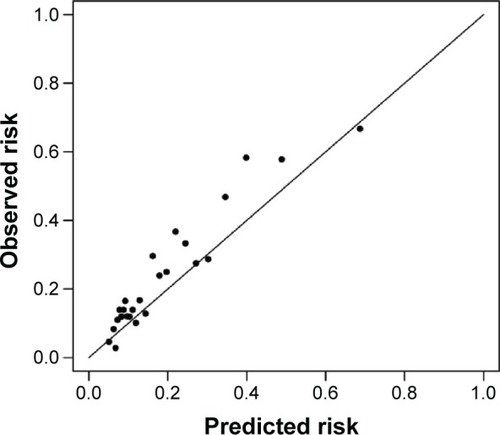
The final multivariable model contained eleven variables, of which the number of exacerbations in the preceding year had the strongest association. Most other variables were associated with relatively modest odds ratios (ORs) (). The overall C statistic for the model was 0.751 (95% CI 0.742–0.761) (). The Hosmer–Lemeshow test had a P-value of 0.30, suggesting no significant departures from goodness of fit. The model and a patient example are included in the Supplementary material.
Table 4 Significant multivariable predictors of two or more COPD exacerbations in the outcome year in the total population data set (N=16,565)
Figure 2 Calibration plot of observed versus predicted risk using the full developmental model (N=16,565).
The model developed using the asthma-free subset (subpopulation 1) was very similar to that for the full population (with the obvious exception of asthma) and had similar ORs (). The smaller subset of patients for whom CAT questionnaire data were available (subpopulation 2) also produced a similar model, although several variables important to the full data set were no longer retained in the subpopulation 2 model. This latter model included two additional variables (CAT score and female sex) not in the full model, but including these variables did not appreciably alter the C statistic for the full model. Age was a much stronger risk factor in subpopulation 2 than in the other models ().
Table 5 Significant multivariable predictors of two or more COPD exacerbations in the outcome year among subpopulations
Model validation
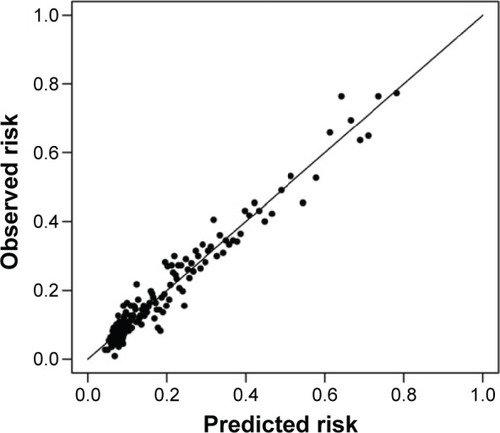
Summary measures of internal validity were unremarkable and suggested adequate fit and predictive ability for the full-population model. Applying the full-population model to the validation data set (N=2,713; baseline characteristics in Table S2) resulted in a C statistic of 0.735 (95% CI 0.713–0.757), suggesting good external validity within the validation cohort ().
Comparison of the model with other indices
The DOSE index score () and GOLD group categorization were determined using the mMRC score for 3,558 patients with available data (Table S1). The C statistic (95% CI) for a model using the DOSE index was 0.641 (0.617–0.664) and that using the GOLD groups was 0.644 (0.622–0.666) as compared with 0.751 (0.742–0.761) for our full-population model.
Discussion
Using a large database of routinely collected electronic health records from patients with COPD in the UK, we developed and validated a model incorporating eleven variables that performed well in predicting two or more COPD exacerbations in the subsequent year (C statistic of 0.751). Sensitivity analyses in the subpopulations with no asthma ever recorded (C statistic 0.742) and with patient-recorded questionnaire data (C statistic 0.745) supported the main results. The frequency of exacerbations in the previous year was the major predictor of future exacerbation risk. Our findings provide evidence that routinely collected health care data can be used to predict frequent COPD exacerbations. Moreover, our model performed better for predicting COPD exacerbations when applied to our heterogeneous study population than models using the DOSE index or GOLD groups calculated using the mMRC score.
Many other predictive studies have focused on risk of death or hospitalization, often among patients with severe COPD.Citation13,Citation15,Citation17,Citation19–Citation21 A strength of the current study is the inclusion of all individuals with COPD in a general population and all subsequent exacerbations, regardless of whether the exacerbation required hospitalization.
Exacerbation rates were relatively low in the study, with >50% of patients having no acute exacerbation in either the baseline or the outcome years, possibly a result of the broadly inclusive eligibility criteria that produced a distribution of COPD severities, from mild to very severe, within the study population;Citation27 primary care COPD populations are recognized as having lower rates of exacerbations than patients enrolled in clinical trials.Citation28 Moreover, the relatively low rate of exacerbations seen in this study, as compared with past research suggesting mean annual rates of 0.8 in mild COPD and 1.2–2.0 in moderate to very severe COPD,Citation27 may be a reflection of changes in recent years, including better identification of milder COPD, with spirometry being broadly undertaken, and more focused COPD management in UK primary care.Citation29
A value close to 1 for the C statistic indicates that a model has excellent discriminatory power.Citation30 While a C statistic of 0.75 for our model indicates modest predictive ability, the results of the current study compare favorably with those of the earlier studies focused on predicting exacerbations. Miravitlles et alCitation31 performed a cross-sectional assessment of frequent (≥1 per year) exacerbation occurrence among 627 ambulatory patients with COPD. Significant covariates included age, FEV1, and chronic mucus hypersecretion, but none of these were particularly strong risk factors (OR for hypersecretion 1.54), and the predictive ability of the model was marginal (C statistic 0.6).
A substantial number of prospective studies have also attempted to predict COPD exacerbations. Niewoehner et alCitation18 followed 1,829 veterans for 6 months to assess the risk of either COPD exacerbation or COPD hospitalization. Significant independent predictors for exacerbation included older age, FEV1, productive cough, previous hospitalization, and medications used previously. However, all patients had moderate to severe COPD, and the short follow-up may have limited the predictive ability of the model, which was itself inferior (C statistic 0.67). Hurst et alCitation32 followed 2,138 patients with COPD for 3 years to assess risk of COPD exacerbations requiring antibiotics, corticosteroids, or hospitalization. Significant multivariable predictors of two or more exacerbations included previous exacerbation, FEV1, history of GERD, increased white cell count, and respiratory health status. Predictive ability of the full model was not reported. Bertens et alCitation16 followed 243 patients with COPD for 24 months to assess the risk of exacerbation occurrence. Their multivariable model identified FEV1, smoking pack-years, history of vascular disease, and previous exacerbations (as a dichotomous variable, yes/no) as significant predictors. The model C statistic (0.75) suggested good predictive ability, but the small sample raises issues as to general applicability of these findings, which are mirrored by a marginal external validity (validation C statistic 0.66). Bowler et alCitation33 followed 3,804 patients with COPD for an average of 3 years, identifying ten significant exacerbation predictors, especially FEV1, St George severity score, and exacerbation in the previous year. However, none were strong risk factors (OR 1.19 per exacerbation in the previous year), and information on overall predictive ability and external validation was not provided.
The largest prospective study conducted to date included ~59,000 patients with COPD from a primary care database and followed them for 1 year. Multivariable logistic regression identified many significant predictors of two or more exacerbations, including previous exacerbation, airflow, level of dyspnea, female sex, and various comorbidities (eg, heart failure, renal disease, anxiety, and asthma). Unfortunately, predictive ability of the model was not reported.Citation34
Most recently, Make et alCitation35 followed 3,141 patients from several drug trials with a history of ≥1 COPD exacerbation in the previous year in order to predict the 6-month risk of an exacerbation requiring corticosteroids or emergency/hospital visit. Independent predictors from a multivariable model included number of maintenance medications, inhaler use, exacerbations in the previous year, FEV1/FVC ratio, female sex, and respiratory health status. The C statistic of 0.67 suggested only moderate predictive ability.
Our study identified the number of exacerbations in the previous year as a significant predictive factor, which was borne out by most of the studies cited earlier. Bowler et alCitation33 and Make et alCitation35 reported only moderately increased risk for previous exacerbation, although the latter study used one previous exacerbation as the reference value (rather than none) in patients with at least one previous exacerbation. However, Bertens et alCitation16 reported an OR of 5.07 (95% CI 2.55–10.07) for at least one exacerbation in the previous year, and Hurst et alCitation32 reported an OR of 5.72 (95% CI 4.47–7.31) for this same measure. Müllerová et alCitation34 reported an exposure–response relationship, with one previous exacerbation associated with an OR of 3.31 (95% CI 3.12–3.51) and two or more associated with an OR of 13.64 (12.67–14.68). The findings from these latter three studies are consistent with those reported in the current study. Furthermore, our results and those reported by Müllerová et alCitation34 suggest that risk increases with increasing number of previous exacerbations, highlighting the importance of obtaining detailed information on this variable.
Neither our multivariable model nor most other predictive models have identified an independent association between smoking and frequent exacerbations in a broad population of patients with COPD. This suggests that the impact of this variable is dependent on inclusion criteria frequently applied to select patients with COPD for controlled trials. Any association with smoking may also be ameliorated by a so-called “healthy smoker effect”, in which those with poorer lung function or frequent exacerbations tend to quit smoking, whereas less severely affected patients do not.Citation18 This suggests that there is a phenotypical propensity to frequent exacerbation that is somewhat independent of other risk factors.Citation32,Citation34
A unique finding of the current study was the significance of blood eosinophilia as an independent predictor. This is consistent with research showing that eosinophils are present in 20%–40% of sputum samples from patients with stable COPD and that airway eosinophilia increases during exacerbation episodes.Citation36 This variable had only a moderate OR of ~1.3, and only among patients not currently smoking, so there may be somewhat limited applicability for predicting exacerbations in general. However, the relatively weak association with eosinophilia may reflect more active COPD management among this population compared with others. We conducted a post hoc sensitivity analysis to evaluate whether the association between blood eosinophilia and the risk of two or more exacerbations would be relevantly different after excluding the 17% (n=2,785) of patients with blood eosinophil counts measured at an exacerbation. The results were not relevantly different after excluding these measurements from the analyses (OR 1.26 [95% CI 1.04–1.52] vs 1.29 [1.10–1.51] for the full population).
We also identified CAT score as a significant predictor for subpopulation 2, which to the best of our knowledge has not been reported elsewhere. Indices of COPD severity such as the BODE index have been significantly linked to future exacerbations,Citation9,Citation37 but these are more complex than the simple CAT survey.
A major strength of the current study is the sample size of >16,000 patients, which is much larger than most other predictive studies. In fact, the population in the current study was more than fivefold larger than all but that of Müllerová et al.Citation34 However, it is likely that some of the variables retained in our final model reached significance primarily because of this large sample rather than because of strong biological importance. Müllerová et alCitation34 similarly reported relatively weak OR for many of their predictors but without information on the overall model predictability or the predictive power of individual variables.
We identified a number of comorbid predictors, including heart disease, GERD, and other respiratory conditions. Conditions such as GERD and heart disease have been identified in other follow-up studies,Citation32–Citation34 whereas risk factors such as nasal polyps and rhinitis appear unique to the current study. These findings highlight the potentially complex relationship that may exist between COPD and other conditions. Although these comorbidities were not strong risk factors (OR 1.1–1.4), their importance would likely improve in a model of newly diagnosed COPD patients without history of exacerbation. Of course, some of these significant predictors may have been driven by the large sample size.
Asthma is recognized as an important comorbid condition that increases disability and risk of exacerbation among those with COPD.Citation38,Citation39 Asthma was also a significant independent predictor in the current study. However, the OR for asthma was of similar magnitude as that for several other variables, and excluding patients with any record of asthma did not appreciably change the model. Such findings may reflect an overuse of the asthma “label”, especially in the past. We applied a very sensitive definition to select the subpopulation of patients without overlapping asthma, namely, the recording of any Read code that could indicate the general practitioner (GP) was considering asthma, which explains the relatively high proportion of patients reported with COPD and concomitant asthma. We cannot exclude the possibility of some patients being wrongly diagnosed with asthma by the GP or, conversely, of some patients having undiagnosed asthma.
Differences between the current study and previous clinical research may partially reflect the populations studied. Clinical trials typically enroll restricted populations with more severe disease, often with a greater frequency of exacerbation at baseline.Citation16,Citation35 The current population better reflects the broader landscape of patients with COPD treated in routine primary care practice in the UK. Nonetheless, we cannot rule out the possibility of selection bias. For example, we required an FEV1/FVC ratio of <0.7 for study inclusion. Because spirometry is not universally available in primary care settings, 11,658 of 37,224 (31%) otherwise potentially eligible patients did not have spirometry results and hence were excluded. With regard to the requirement for blood eosinophil count, full blood count measurements are very common among patients with COPD and were available for 86% of patients evaluated (43,436 of 50,716 patients with COPD and no other chronic respiratory disease).
Our aim was to evaluate the predictive value of routinely collected data. Although other parameters of eosinophilic inflammation, such as sputum eosinophils or exhaled nitric oxide, may have improved the predictive performance of the model, these measurements are generally unavailable in general practice and hence were not included in our model. The current study used electronic records from primary care providers, which are a readily available data source. However, it is possible that outcomes such as hospital and emergency admissions may be underrepresented in the data.
The current study was validated both internally and externally, with good concordance when the multivariable model was applied to an external sample. However, this does not guarantee universal generalizability given that our external sample arose from the same patient population as the sample used for model development. Further study is needed to validate the model in other patient populations as well.
Conclusion
Routine, electronic medical record data available from most GP clinical systems can be used to identify patients with COPD at risk of two or more exacerbations the subsequent year. Our model could be used to profile patients with COPD, or to underpin decision support tools, in general practice. The number of exacerbations in the preceding year showed a strong exposure–response relationship, highlighting the importance of detailed information on patients’ exacerbation history. The findings also suggest that CAT score and eosinophilia may be convenient markers of future exacerbation, at least in some populations.
Author contributions
Drs Freeman and Price were responsible for study conception and design. Dr Kerkhof was also involved with study design and data analysis. All authors were involved with interpretation of the data, writing, and revision of the paper and decision to submit the paper for publication.
Acknowledgments
This study was funded by an unrestricted grant from the Respiratory Effectiveness Group (REG; www.effectivenessevaluation.org). Access to data from the Optimum Patient Care Research Database was co-funded by Research in Real-Life Ltd (RiRL, Cambridge, UK). The authors would like to thank Dr John Bukowski of WordsWorld Consulting for editorial assistance drafting this manuscript. Additional editorial support was provided by Elizabeth V Hillyer, DVM, funded by RiRL.
Supplementary materials
The formula: Risk of ≥2 COPD exacerbations within the next 12 months =1/(1+ exp(−0.7306+0.8840×1 previous exacerbation in last 12 months +1.4786×2 previous exacerbations in last 12 months +1.9857×3 previous exacerbations in last 12 months +2.8811× ≥4 previous exacerbations in last 12 months −0.0093× FEV1% predicted +0.0360× age −0.0004× age2 −1.2194× height (in meter) +0.2518× (blood eosinophil count ≥400/μL in a patient who is not currently smoking) +0.2953× any evidence of asthma ×0.3018× history of nonallergic rhinitis +0.3298× history of nasal polyps +0.1164× history of ischemic heart disease +0.1071× history of anxiety of depression +0.1689× history of GERD).
Example: a person aged 70 years currently smoking with height of 1.80 m and FEV1 of 60% of predicted, without a history of previous exacerbations in the last 12 months and no history of comorbidities, has a calculated risk of 0.064 (6.4%) of two or more exacerbations in the next year.
Table S1 Baseline mMRC scores, DOSE index scores, and GOLD groups based on mMRC score
Table S2 Baseline characteristics of the validation cohort
References
- Global Initiative for Chronic Obstructive Lung Disease (GOLD)Global Strategy for the Diagnosis, Management and Prevention of COPD, 20152015 Available from: http://www.goldcopd.org/Accessed July 7, 2015
- JonesRCDonaldsonGCChavannesNHDerivation and validation of a composite index of severity in chronic obstructive pulmonary disease: the DOSE IndexAm J Respir Crit Care Med2009180121189119519797160
- BestallJCPaulEAGarrodRGarnhamRJonesPWWedzichaJAUsefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary diseaseThorax199954758158610377201
Disclosure
MK is an employee of Research in Real-Life, which conducted this study and which has conducted paid research in respiratory disease on behalf of the following other organizations in the past 5 years: Aerocrine, AKL Ltd, Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Meda, Mundipharma, Napp, Novartis, Orion, Takeda, Teva, and Zentiva, a Sanofi company.
DF is a director of Respiratory Education Alliance, a company providing educational packages in the Middle and Far East, and has received fees for lectures/professional consultation from AZ, BI, GSK, Mundipharma, Novartis, and TEVA and has received educational support from Napp, Almirall, BI, and Novartis.
RJ reports personal fees from Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla GSK; grants, personal fees, nonfinancial support from Novartis; personal fees and nonfinancial support from Napp/Mundipharma.
AC has no relevant conflicts to declare.
DBP has Board Membership with Aerocrine, Almirall, Amgen, AstraZeneca, Boehringer Ingelheim, Chiesi, Meda, Mundipharma, Napp, Novartis, and Teva. Consultancy: Almirall, Amgen, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Meda, Mundipharma, Napp, Novartis, Pfizer, Teva, and Zentiva; grants/grants pending with UK National Health Service, British Lung Foundation, Aerocrine, AstraZeneca, Boehringer Ingelheim, Chiesi, Eli Lilly, GlaxoSmithKline, Meda, Merck, Mundipharma, Novartis, Orion, Pfizer, Respiratory Effectiveness Group, Takeda, Teva, and Zentiva; payments for lectures/speaking: Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, GlaxoSmithKline, Kyorin, Meda, Merck, Mundipharma, Novartis, Pfizer, SkyePharma, Takeda, and Teva; payment for manuscript preparation: Mundipharma and Teva; patents (planned, pending, or issued): AKL Ltd; payment for the development of educational materials: GlaxoSmithKline, Novartis; stock/stock options: shares in AKL Ltd that produces phytopharmaceuticals and owns 80% of Research in Real-Life Ltd and its subsidiary social enterprise Optimum Patient Care; received payment for travel/accommodations/meeting expenses from Aerocrine, Boehringer Ingelheim, Mundipharma, Napp, Novartis, and Teva; funding for patient enrollment or completion of research: Almirall, Chiesi, Teva, and Zentiva; peer reviewer for grant committees: Medical Research Council (2014), Efficacy and Mechanism Evaluation programme (2012), HTA (2014); and received unrestricted funding for investigator-initiated studies from Aerocrine, AKL Ltd, Almirall, Boehringer Ingelheim, Chiesi, Meda, Mundipharma, Napp, Novartis, Orion, Takeda, Teva, and Zentiva. The authors report no other conflicts of interest in this work.
References
- VestboJHurdSSAgustíAGGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med2013187434736522878278
- PunekarYSShuklaAMullerovaHCOPD management costs according to the frequency of COPD exacerbations in UK primary careInt J Chron Obstruct Pulmon Dis20149657324426781
- CroxtonTLWeinmannGGSeniorRMWiseRACrapoJDBuistASClinical research in chronic obstructive pulmonary disease: needs and opportunitiesAm J Respir Crit Care Med200316781142114912684252
- CelliBCrossSGrossmanRImproving the care of COPD patients – suggested action points by the COPD exacerbations taskforce for reducing the burden of exacerbations of COPDPrim Care Respir J200615313914216757393
- DecramerMJanssensWMiravitllesMChronic obstructive pulmonary diseaseLancet201237998231341135122314182
- LangePMarottJLVestboJPrediction of the clinical course of chronic obstructive pulmonary disease, using the new GOLD classification: a study of the general populationAm J Respir Crit Care Med20121861097598122997207
- Global Initiative for Chronic Obstructive Lung Disease (GOLD)Global Strategy for the Diagnosis, Management and Prevention of COPD, 20152015 Available from: http://www.goldcopd.org/Accessed July 7, 2015
- HanMKMuellerovaHCurran-EverettDGOLD 2011 disease severity classification in COPDGene: a prospective cohort studyLancet Respir Med201311435024321803
- MotegiTJonesRCIshiiTA comparison of three multidimensional indices of COPD severity as predictors of future exacerbationsInt J Chron Obstruct Pulmon Dis2013825927123754870
- FaganelloMMTanniSESanchezFFPelegrinoNRLuchetaPAGodoyIBODE index and GOLD staging as predictors of 1-year exacerbation risk in chronic obstructive pulmonary diseaseAm J Med Sci20103391101419926966
- JonesRCDonaldsonGCChavannesNHDerivation and validation of a composite index of severity in chronic obstructive pulmonary disease: the DOSE IndexAm J Respir Crit Care Med2009180121189119519797160
- JonesRPriceDChavannesNA comparison of multi-component indices of COPD severity in primary care: an UNLOCK study from the IPCRGEur Respir J201342suppl 572006
- Garcia-AymerichJMonsóEMarradesRMEFRAM InvestigatorsRisk factors for hospitalization for a chronic obstructive pulmonary disease exacerbation. EFRAM studyAm J Respir Crit Care Med200116461002100711587986
- ForemanMGDeMeoDLHershCPReillyJJSilvermanEKClinical determinants of exacerbations in severe, early-onset COPDEur Respir J20073061124113017715170
- BahadoriKFitzGeraldJMLevyRDFeraTSwistonJRisk factors and outcomes associated with chronic obstructive pulmonary disease exacerbations requiring hospitalizationCan Respir J2009164e43e4919707601
- BertensLCReitsmaJBMoonsKGDevelopment and validation of a model to predict the risk of exacerbations in chronic obstructive pulmonary diseaseInt J Chron Obstruct Pulmon Dis2013849349924143086
- FanVSRamseySDMakeBJMartinezFJPhysiologic variables and functional status independently predict COPD hospitalizations and emergency department visits in patients with severe COPDCOPD200741293917364675
- NiewoehnerDELokhnyginaYRiceKRisk indexes for exacerbations and hospitalizations due to COPDChest20071311202817218552
- AustinPCStanbrookMBAndersonGMNewmanAGershonASComparative ability of comorbidity classification methods for administrative data to predict outcomes in patients with chronic obstructive pulmonary diseaseAnn Epidemiol2012221288188723121992
- RoweBHVilla-RoelCGuttmanAPredictors of hospital admission for chronic obstructive pulmonary disease exacerbations in Canadian emergency departmentsAcad Emerg Med200916431632419298621
- StiellIGClementCMAaronSDClinical characteristics associated with adverse events in patients with exacerbation of chronic obstructive pulmonary disease: a prospective cohort studyCMAJ20141866E193E20424549125
- LiuDPengSHZhangJBaiSHLiuHXQuJMPrediction of short term re-exacerbation in patients with acute exacerbation of chronic obstructive pulmonary diseaseInt J Chron Obstruct Pulmon Dis2015101265127326170655
- Optimum Patient Care Research Database (OPCRD) Available from: http://optimumpatientcare.org/Accessed July 7, 2015
- BestallJCPaulEAGarrodRGarnhamRJonesPWWedzichaJAUsefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary diseaseThorax199954758158610377201
- JonesPWHardingGBerryPWiklundIChenWHKline LeidyNDevelopment and first validation of the COPD Assessment TestEur Respir J200934364865419720809
- HosmerDWLemeshowSApplied Logistic RegressionNew YorkWiley1989
- HoogendoornMFeenstraTLHoogenveenRTAlMMolkenMRAssociation between lung function and exacerbation frequency in patients with COPDInt J Chron Obstruct Pulmon Dis2010543544421191438
- KruisALStällbergBJonesRCPrimary care COPD patients compared with large pharmaceutically-sponsored COPD studies: an UNLOCK validation studyPLoS One201493e9014524598945
- JonesRCPriceDRyanDRespiratory Effectiveness GroupOpportunities to diagnose chronic obstructive pulmonary disease in routine care in the UK: a retrospective study of a clinical cohortLancet Respir Med20142426727624717623
- PencinaMJD’AgostinoRBSrEvaluating discrimination of risk prediction models: the C statisticJAMA2015314101063106426348755
- MiravitllesMGuerreroTMayordomoCSanchez-AgudoLNicolauFSeguJLFactors associated with increased risk of exacerbation and hospital admission in a cohort of ambulatory COPD patients: a multiple logistic regression analysis. The EOLO Study GroupRespiration200067549550111070451
- HurstJRVestboJAnzuetoAEvaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) InvestigatorsSusceptibility to exacerbation in chronic obstructive pulmonary diseaseN Engl J Med2010363121128113820843247
- BowlerRPKimVReganECOPDGene InvestigatorsPrediction of acute respiratory disease in current and former smokers with and without COPDChest2014146494195024945159
- MüllerováHShuklaAHawkinsAQuintJRisk factors for acute exacerbations of COPD in a primary care population: a retrospective observational cohort studyBMJ Open2014412e006171
- MakeBJErikssonGCalverleyPMA score to predict short-term risk of COPD exacerbations (SCOPEX)Int J Chron Obstruct Pulmon Dis20151020120925670896
- SahaSBrightlingCEEosinophilic airway inflammation in COPDInt J Chron Obstruct Pulmon Dis200611394718046901
- PuhanMAGarcia-AymerichJFreyMExpansion of the prognostic assessment of patients with chronic obstructive pulmonary disease: the updated BODE index and the ADO indexLancet2009374969170471119716962
- HardinMSilvermanEKBarrRGCOPDGene InvestigatorsThe clinical features of the overlap between COPD and asthmaRespir Res20111212721951550
- PapaiwannouAZarogoulidisPPorpodisKAsthmachronic obstructive pulmonary disease overlap syndrome (ACOS): current literature reviewJ Thorac Dis20146suppl 1S146S15124672688