Abstract
Aims
We aimed to comprehensively assess the risk of gastrointestinal toxicities associated with poly (ADP-ribose) polymerase inhibitors (PARPis) in the treatment of ovarian cancer patients.
Materials and methods
We searched several databases for relevant trials. Eligible studies included prospective Phase II and III trials of ovarian cancer patients on the four PARPis (olaparib, veliparib, niraparib and rucaparib), describing events of nausea, vomiting, diarrhea, and constipation. Summary incidence, relative risk (RR), and 95% CIs were calculated employing fixed- or random-effects models.
Results
A total of 2,286 ovarian cancer patients from 12 trials were included for analysis. Our results showed that summary incidences of all-grade gastrointestinal events in ovarian cancer patients were nausea 68.8% (95% CI, 63.5%–73.6%), vomiting 36.2% (95% CI, 30.9%–41.8%), diarrhea 25.3% (95% CI, 21.2%–29.8%), and constipation 25.3% (95% CI, 17.9%–34.5%). The RRs of all-grade nausea, vomiting, diarrhea, and constipation were 2.00 (95% CI: 1.79–2.24; P<0.001), 2.12 (95% CI: 1.75–2.58; P<0.001), 1.20 (95% CI: 1.01–1.44; P=0.044), and 1.20 (95% CI: 0.88–1.80; P=0.21); respectively. While, the RRs of high-grade nausea, vomiting, diarrhea, and constipation were 3.74 (95% CI: 1.50–9.36; P=0.005), 2.81 (95% CI: 1.17–6.74; P=0.02), 0.56 (95% CI: 0.22–1.43; P=0.23), 0.92 (95% CI: 0.34–2.49, P=0.87); respectively.
Conclusion
Our study suggests that the risk of all-grade gastrointestinal toxicities associated with PARPis, excepting constipation, is significantly increased in ovarian cancer patients. And the use of PARPis significantly increased the risk of developing high-grade nausea and vomiting, but not for diarrhea and constipation. Close clinical monitoring is recommended when administering these drugs.
Introduction
Ovarian cancer is the second most common gynecologic malignancy and is the leading cause of death from gynecologic cancers worldwide.Citation1,Citation2 Typically, ovarian cancer presents with advanced stages at the time of diagnosis.Citation3 Although most patients with advanced ovarian cancer initially receive platinum-based chemotherapy and achieve a clinical response, the effectiveness of the treatments diminishes over time, and most of these patients will ultimately relapse.Citation4–Citation6 The prognosis of these recurrent ovarian cancer patients is very poor, with a median survival ranging from 12 months to 24 months.Citation7 Clearly, novel effective drugs or treatment strategies that can improve long-term disease control in recurrent ovarian cancer are urgently needed.Citation8
Recent advances in the understanding of the molecular biology and mechanism of epithelial ovarian cancer have led to the development of a number of targeted therapies, including poly-ADP-ribose polymerase inhibitors (PARPis).Citation9,Citation10 PARPis are a novel class of therapeutic agents that target tumors with deficiencies in the homologous recombination DNA repair pathway. Until now, three PARPis olaparib,Citation11 niraparib,Citation12 and rucaparibCitation13 have been approved for use in ovarian cancer by the US Food and Drug Administration. As these drugs have now entered routine clinical practice, more and more patients would receive PARPis, and concerns increase regarding the toxicities associated with the administration of PARPis. In a previously published meta-analysis conducted by Zhou et al,Citation14 the authors found that treatment with the PARPis olaparib, veliparib, and niraparib was associated with a significant increase in the risk of developing hematologic toxicities in cancer patients. Gastrointestinal (GI) toxicities associated with PARPis have been reported in clinical trials, but the results are controversial.Citation15,Citation16 As a result, we conducted the present meta-analysis of all available trials to comprehensively assess the overall incidence and risk of selected GI toxicities (nausea, vomiting, diarrhea, and constipation) associated with PARPis in the treatment of ovarian cancer.
Materials and methods
Data source
Several databases including PubMed, Web of Science and Cochrane library were searched for relevant trials. The search key words were PARPis, olaparib, veliparib, niraparib, rucaparib and ovarian cancer. Additionally relevant articles in the reference lists of recent meta-analyses that investigated PARPis in ovarian cancer patients were also searched. In order to avoid duplication, only the most complete or recent was considered for analysis. All results were input into End-note X8 reference software (Thomson Reuters, Stamford, CT, USA) for duplication exclusion and further reference management. Finally, the most updated package inserts of olaparib, niraparib, and rucaparib were reviewed to identify other relevant information. Trials were chosen and reviewed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.Citation17
Study selection
The primary objective of the present study was to evaluate the overall incidence of PARPis-related GI toxicities and the risk of GI toxicities in ovarian cancer patients treated with PARPis; therefore, only prospective phase II and III trials evaluating PARPis in ovarian cancer patients with adequate data on GI toxicities were incorporated in the analysis. Phase I trials were omitted due to multiple dose level and limited sample sizes. Clinical trials that met the following criteria were included as follows: 1) prospective phase II and III trials, expanded access protocols (EAPs); 2) participants assigned to treatment with PARPis (alone or in combination at any dosage or frequency); and 3) available data regarding events or incidence of GI toxicities and sample size. Phase I trials were excluded because of inter-study variability in drug dosing as well as the small number of patients in these trials.
Data extraction
Two investigators independently conducted data abstraction, and any discrepancy between the reviewers was resolved by consensus. Most of the incorporated trials have used the common terminology criteria of adverse events version 4.0 for grading of the relevant adverse events. A checklist of necessary data to be extracted from each study included: first author’s name, year of publication, phases of trials, number of enrolled subjects, treatment arms, number of patients in treatment and controlled groups, median age, median progression-free survival, and the number of each of the selected GI adverse events.
Statistical analysis
The primary summary measures were incidence, relative risk (RR), and corresponding 95% CIs of all grade (grade 1–4) and high-grade (grade 3–4) selected GI toxicities. All statistical analyses were performed by using Version 2 of the Comprehensive MetaAnalysis program (Biostat, Englewood, NJ, USA). For the calculation of incidence, the number of patients with selected GI toxicities in PARPis alone and the total number of patients receiving PARPis alone were extracted. To calculate RR, patients assigned to PARPis were compared only with those assigned to control treatment in the same trial. Between-study heterogeneity was estimated using the χ2-based Q statistic.Citation18 Heterogeneity was considered statistically significant when Pheterogeneity <0.1. The presence of publication bias was evaluated by using the Begg and Egger tests.Citation19,Citation20 A statistical test with a P-value <0.05 was considered significant.
Results
Search results
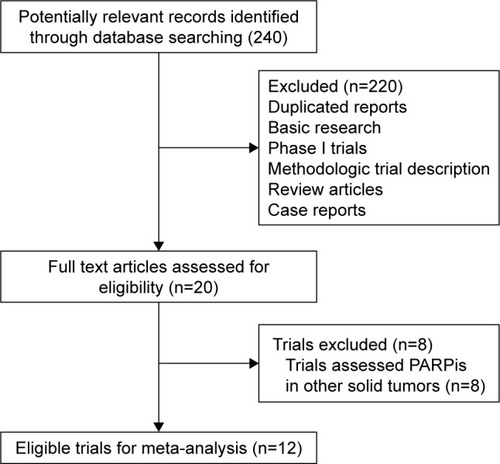
Our search yielded 240 potentially relevant citations on PARPis from the searched databases. The details for the study inclusion/exclusion procedure are illustrated in . A total of 12 trials were considered eligible for the analysis, including three Phase III trialsCitation21–Citation23 and nine Phase II trials.Citation24–Citation32 A total of 2,286 patients were included in this analysis. Most patients had a performance score between 0 and 2 and competent liver, kidney and bone marrow function. The baseline patients’ characteristics in each trial are described in .
Table 1 Baseline characteristics of included trials
Overall incidence of relevant adverse events
For the incidence analysis, we considered ovarian cancer patients receiving PARPis monotherapy. The pooled incidence of all-grade nausea, vomiting, diarrhea, and constipation was 68.8% (95% CI, 63.5%–73.6%), 36.2% (95% CI, 30.9%–41.8%), 25.3% (95% CI, 21.2%–29.8%), and 25.3% (95% CI, 17.9%–34.5%), respectively. There was significant heterogeneity among trials, and we thus performed the meta-analysis by using a random-effects model (). As for high-grade GI toxicities, the pooled incidence of GI toxicities associated with PARPis was nausea 3.4% (95% CI, 2.6%–4.5%), vomiting 2.0% (95% CI, 1.4%–3.0%), diarrhea 1.7% (95% CI, 1.0%–3.0%), and constipation 1.4% (95% CI, 0.9%–2.3%), respectively. There was no significant heterogeneity among included trials, and we thus performed the meta-analysis by using a fixed-effects model ().
Table 2 Incidence of adverse outcomes for clinical trials included in the meta-analysis
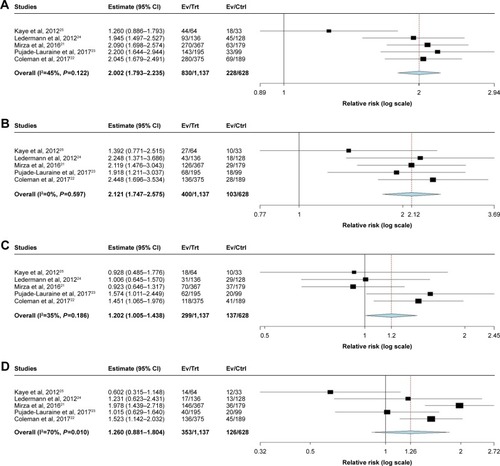
RR of all-grade relevant GI toxicities
A meta-analysis of the RR of all-grade adverse events was performed on the included randomized controlled trials (RCTs), which contained a direct comparison between PARPis and control treatment. The RRs of all-grade nausea, vomiting, diarrhea, and constipation were 2.00 (95% CI: 1.79–2.24; P<0.001, ), 2.12 (95% CI: 1.75–2.58; P<0.001, ), 1.20 (95% CI: 1.01–1.44; P=0.044, ), 1.26 (95% CI: 0.88–1.20); P<0.001, ); respectively. Thus, patients treated with PARPis had an increased risk of developing all-grade nausea, vomiting, diarrhea, and constipation. The fixed effects model was used for all the evaluated toxicities, except for constipation.
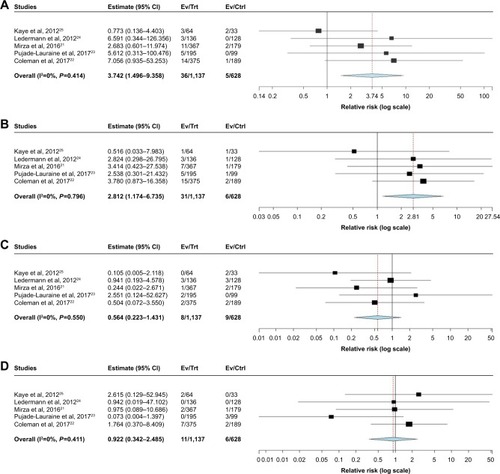
RR of high-grade relevant GI toxicities
RCTs directly comparing PARPis with control treatment were included to calculate RRs of high-grade GI toxicities. The RR of high-grade nausea, vomiting, diarrhea, and constipation were 3.74 (95% CI: 1.50–9.36; P=0.005, ), 2.81 (95% CI: 1.17–6.74; P=0.02, ), 0.56 (95% CI: 0.22–1.43; P=0.23, ), 0.92 (95% CI: 0.34–2.49, P=0.87, ); respectively. Thus, patients treated with PARPis had an increased risk of developing high-grade nausea and vomiting, but not for high-grade diarrhea and constipation. The fixed effects model was used for all evaluated toxicities.
Discussion
To the best of our knowledge, this is the most comprehensive and up-dated meta-analysis to provide an investigation of overall incidence and risk of GI toxicities in ovarian cancer patients treated with PARPis. Our analysis of data demonstrates that the risk of all-grade gastrointestinal toxicities associated with PARPis is significantly increased in the treatment of ovarian cancer. In addition, the use of PARPis in ovarian cancer significantly increases the risk of developing high-grade nausea and vomiting, but not for diarrhea and constipation. The four PARPis evaluated within our analysis are olaparib, veliparib, niraparib, and rucaparib. And three of them olaparib, niraparib, and rucaparib have been approved for use in ovarian cancer due to their survival benefits. Additionally, a number of ongoing Phase II and III studies are assessing these agents in multiple other solid tumors indications.Citation33,Citation34 Therefore, the use of PARPis is anticipated to increase in the near future, and clinicians should pay particular attention to regular monitoring of GI toxicities related to PARPis during the administration of these drugs.
Until now, GI toxicities are considered an important cause for treatment interruption and/or permanent discontinuation in the clinical trials. Although high-grade GI toxicities are relatively uncommon, there are currently no methods to predict patients at highest risk, and thus regular monitoring of clinical parameters during the administration of these drugs is warranted. Generally, administration of supportive therapy should be undertaken with the earliest manifestation of nausea and vomiting experienced by ovarian cancer patients treated by PARPis.
However, as far as we know, there are no specific guidelines for the treatment of PARPis-induced GI toxicities due to lack of controlled studies addressing the subject. The philosophy of management of anticancer-related GI toxicities extends to employing some nutritional interventions. In a recent Cochrane review evaluating how to minimize the frequency of diarrhea associated with pelvic radiotherapy, the authors found that combinations of modified fat, lactose-restriction, fat-restriction and fiber supplementation was recommended to reduce to the frequency of diarrhea.Citation35 Additionally, according to the package insert of approved PARPis,Citation36–Citation38 if grade three or higher non-hematological toxicity occurs, temporary dose interruption and/or dose reduction to half the dose previously administered should be considered based on tolerability and severity.
A number of limitations are needed to be acknowledged: first, as with any similar meta-analysis, the pooled results of our study are significantly affected by the confounding factors of individual studies that are chosen. Second, this meta-analysis only includes published trials, and a meta-analysis of individual level data might define more clearly treatment benefits in specific subgroups. Third, heterogeneity is observed in some of the RR analyses. This may be related to the different PARPis for the RR analysis, and differences in sample size, although we have tried to minimize its influence by using the random-effect model. Finally, as the present meta-analysis excludes Phase I trials, the impact of PARPis dose/schedules on the risk of gastrointestinal toxicities could not be fully assessed in this analysis.
Conclusion
Our study suggests that the risk of all-grade gastrointestinal toxicities associated with PARPis is significantly increased in ovarian cancer patients receiving these drugs. And the use of PARPis significantly increased the risk of developing high-grade nausea and vomiting, but not for diarrhea and constipation. Although the rate of clinically high-grade GI toxicities is very low, clinicians should be aware of these risks and perform regular assessment for such toxicities during administration of these drugs. Additionally, further research into the pathogenesis of these toxicities is still needed.
Disclosure
The authors report no conflicts of interest in this work.
References
- JemalABrayFCenterMMFerlayJWardEFormanDGlobal cancer statisticsCA Cancer J Clin2011612699021296855
- SiegelRMaJZouZJemalAStatisticsCCancer statistics, 2014CA Cancer J Clin201464192924399786
- BookmanMAOptimal primary therapy of ovarian cancerAnn Oncol201627Suppl. 1i58i6227141074
- CortezAJTudrejPKujawaKALisowskaKMAdvances in ovarian cancer therapyCancer Chemother Pharmacol2018811173829249039
- MarthCReimerDZeimetAGFront-line therapy of advanced epithelial ovarian cancer: standard treatmentAnn Oncol201728Suppl. 8viii36viii3929232473
- KatsumataNYasudaMIsonishiSLong-term results of dose-dense paclitaxel and carboplatin versus conventional paclitaxel and carboplatin for treatment of advanced epithelial ovarian, fallopian tube, or primary peritoneal cancer (JGOG 3016): a randomised, controlled, open-label trialLancet Oncol201314101020102623948349
- FoleyOWRauh-HainJAdel CarmenMGRecurrent epithelial ovarian cancer: an update on treatmentOncology2013274288298294
- MariappanLJiangXYJacksonJDrewYEmerging treatment options for ovarian cancer: focus on rucaparibInt J Womens Health2017991392429290694
- BitlerBGWatsonZLWheelerLJBehbakhtKPARP inhibitors: clinical utility and possibilities of overcoming resistanceGynecol Oncol2017147369570429037806
- SisayMEdessaDPARP inhibitors as potential therapeutic agents for various cancers: focus on niraparib and its first global approval for maintenance therapy of gynecologic cancersGynecol Oncol Res Pract201741829214031
- KimGIsonGMckeeAEFDA Approval summary: Olaparib monotherapy in patients with deleterious germline BRCA-mutated advanced ovarian cancer treated with three or more lines of chemotherapyClin Cancer Res201521194257426126187614
- ScottLJNiraparib: first global approvalDrugs20177791029103428474297
- BalasubramaniamSBeaverJAHortonSFDA Approval summary: Rucaparib for the treatment of patients with deleterious BRCA mutation-associated advanced ovarian cancerClin Cancer Res201723237165717028751443
- ZhouJXFengLJZhangXRisk of severe hematologic toxicities in cancer patients treated with PARP inhibitors: a meta-analysis of randomized controlled trialsDrug Des Devel Ther20171130093017
- MooreKNMonkBJPatient counseling and management of symptoms during olaparib therapy for recurrent ovarian cancerOncologist201621895496327256873
- SamolJRansonMScottESafety and tolerability of the poly(ADP-ribose) polymerase (PARP) inhibitor, olaparib (AZD2281) in combination with topotecan for the treatment of patients with advanced solid tumors: a phase I studyInvest New Drugs20123041493150021590367
- PanicNLeonciniEde BelvisGRicciardiWBocciaSEvaluation of the endorsement of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement on the quality of published systematic review and meta-analysesPLoS One2013812e8313824386151
- ZintzarasEIoannidisJPHeterogeneity testing in meta-analysis of genome searchesGenet Epidemiol200528212313715593093
- YusufSPetoRLewisJCollinsRSleightPBeta blockade during and after myocardial infarction: an overview of the randomized trialsProg Cardiovasc Dis19852753353712858114
- BeggCBMazumdarMOperating characteristics of a rank correlation test for publication biasBiometrics1994504108811017786990
- MirzaMRMonkBJHerrstedtJNiraparib maintenance therapy in platinum-sensitive, recurrent ovarian cancerN Engl J Med2016375222154216427717299
- ColemanRLOzaAMLorussoDRucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): a randomised, double-blind, placebo-controlled, phase 3 trialLancet2017390101061949196128916367
- Pujade-LauraineELedermannJASelleFOlaparib tablets as maintenance therapy in patients with platinum-sensitive, relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): a double-blind, randomised, placebo-controlled, phase 3 trialLancet Oncol20171891274128428754483
- LedermannJHarterPGourleyCOlaparib maintenance therapy in platinum-sensitive relapsed ovarian cancerN Engl J Med2012366151382139222452356
- KayeSBLubinskiJMatulonisUPhase II, open-label, randomized, multicenter study comparing the efficacy and safety of olaparib, a poly (ADP-ribose) polymerase inhibitor, and pegylated liposomal doxorubicin in patients with BRCA1 or BRCA2 mutations and recurrent ovarian cancerJ Clin Oncol201230437237922203755
- GelmonKATischkowitzMMackayHOlaparib in patients with recurrent high-grade serous or poorly differentiated ovarian carcinoma or triple-negative breast cancer: a phase 2, multicentre, open-label, non-randomised studyLancet Oncol201112985286121862407
- AudehMWCarmichaelJPensonRTOral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and recurrent ovarian cancer: a proof-of-concept trialLancet2010376973724525120609468
- DomchekSMAghajanianCShapira-FrommerREfficacy and safety of olaparib monotherapy in germline BRCA1/2 mutation carriers with advanced ovarian cancer and three or more lines of prior therapyGynecol Oncol2016140219920326723501
- Bell-McGuinnKMKonnerJATewWPA phase 2, single arm study of iniparib in patients with BRCA1 or BRCA2 associated advanced epithelial ovarian, fallopian tube, or primary peritoneal cancerInt J Gynecol Cancer201626225526026745694
- ColemanRLSillMWBell-McGuinnKA phase II evaluation of the potent, highly selective PARP inhibitor veliparib in the treatment of persistent or recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer in patients who carry a germline BRCA1 or BRCA2 mutation – An NRG Oncology/Gynecologic Oncology Group studyGynecol Oncol2015137338639125818403
- LiuJFBarryWTBirrerMCombination cediranib and olaparib versus olaparib alone for women with recurrent platinum-sensitive ovarian cancer: a randomised phase 2 studyLancet Oncol201415111207121425218906
- SwisherEMLinKKOzaAMRucaparib in relapsed, platinum-sensitive high-grade ovarian carcinoma (ARIEL2 Part 1): an international, multicentre, open-label, phase 2 trialLancet Oncol2017181758727908594
- LoweryMAKelsenDPCapanuMPhase II trial of veliparib in patients with previously treated BRCA-mutated pancreas ductal adenocarcinomaEur J Cancer201889192629223478
- HanHSDiérasVRobsonMVeliparib with temozolomide or carboplatin/paclitaxel versus placebo with carboplatin/paclitaxel in patients with BRCA1/2 locally recurrent/metastatic breast cancer: randomized phase II studyAnn Oncol201829115416129045554
- HensonCCBurdenSDavidsonSELalSNutritional interventions for reducing gastrointestinal toxicity in adults undergoing radical pelvic radiotherapyCochrane Database Syst Rev20131111CD009896
- Zejula (niraparib) FDA prescribing information Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2017/208447Orig1s000Lbl.pdfAccessed January 6, 2018
- Rubraca (rucaparib) FDA prescribing information Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2016/209115Orig1s000Lbl.pdfAccessed January 6, 2018
- LYNPARZA (olaparib) FDA prescribing information Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/206162s008lbl.pdfAccessed January 6, 2018