Abstract
Madelung’s disease is a rare disorder described for the first time in the year 1846 by Brodie. It is characterized by the occurrence of progressive, excessive, and symmetrical deposits of adipose tissue in the subcutaneous layer. Most often, these changes concern the neck, the nape of the neck, arms, and upper back, giving the patients a specific, pseudoathletic appearance. Madelung’s disease is also known as multiple symmetrical lipomatosis, benign symmetrical lipomatosis, and Launois-Bensaude syndrome. The most commonly affected ones are men who drink alcohol in excessive amounts. The fat masses emerging in the course of the disease are painless but can lead to adverse repercussions. Patients may experience dysphagia, dysphonia, difficulty in breathing, and limited mobility of the neck. The reasons for the willingness to take up treatment are also often esthetic reasons. The disease is usually accompanied by numerous metabolic disorders. The etiology of the disease has not been sufficiently explained so far, which creates diagnostic and therapeutic difficulties. Currently used treatment is limited to surgical resection of the resulting lesions or liposuction. Unfortunately, the effectiveness of these activities is limited. Most patients experience recurrence after treatment. This paper discusses the essence of Madelung’s disease, numerous aspects of etiology, the manner of diagnosis, and treatment based on current literature data.
Introduction
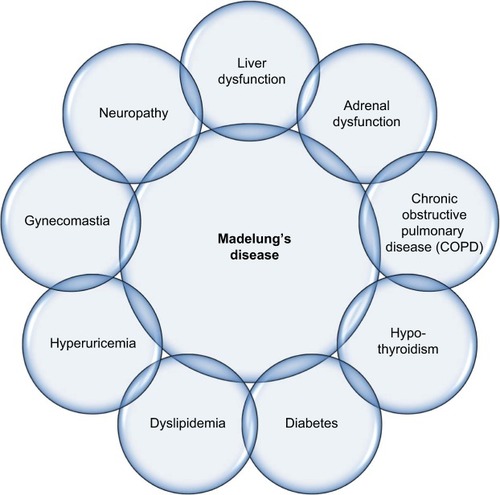
Madelung’s disease is also known as multiple symmetric lipomatosis (MSL), benign symmetric lipomatosis (BSL), and Launois-Bensaude syndrome.Citation1–Citation3 It is a rare disorder characterized by progressive, excessive, and symmetrical accumulation of adipose tissue in the subcutaneous layer, thus giving patients a peculiar appearance.Citation1,Citation2,Citation4,Citation5 EnziCitation6 distinguishes two types of lipomatosis ().
Figure 1 Madelung’s disease: division based on the area of adipose tissue accumulation.
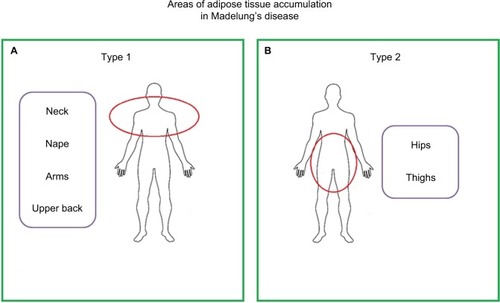
Another classification distinguishes three types of disease.Citation7 The first one is characterized by the dominant cervical localization of excess fat; for the second type, the pseudoathletic appearance is considered characteristic, while in the third type – gynecological – changes are located in the area of the abdomen and hips.Citation7,Citation8 Regardless of the type of the disease, there is rarely any accumulation of fat around the larynx, mediastinum, and distal limbs.Citation9,Citation10 The described changes are painless, but they can lead to unfavorable, often-serious repercussions.Citation4,Citation10 Patients may develop dysphagia, dysphonia, and sleep apnea syndrome. There may be dif ficulties in breathing and limited mobility of the neck. In patients, polyneuropathy is often observed. It is a generalized motor, sensory, and autonomic neuropathy not directly related to the location of fat mass.Citation1,Citation2,Citation5,Citation11 Another indirect consequence of the disease is the occurrence of depressive disorders in patients, resulting from the way they perceive themselves against the background of emerging changes in appearance.Citation7
Madelung’s disease affects men more often – the ratio of men to women varies from 15/1 to 30/1 – and is usually diagnosed between 30 and 70 years of age.Citation1,Citation4,Citation12–Citation14 Most cases of the disease are reported in the Mediterranean region – the incidence in Italy has been reported to be as high as 1 in 25,000 men.Citation1,Citation4,Citation5,Citation9,Citation15 In contrast, in the Asian population, this disease is extremely rare.Citation1,Citation9 In the majority of cases, the disease is diagnosed in men in the 4th and 5th decades of life who consume chronically increased amounts of alcohol, especially in the form of red wine.Citation5,Citation10,Citation16 Moreover, 90% of patients also have secondary liver cirrhosis.Citation4,Citation7 The most frequently diagnosed phenotype of the disease is of type 1,with a dominant fat deposit around the neck.Citation13,Citation14,Citation16
Case report
A 53-year-old man with upper body deformity, a strongly limited neck mobility, and weakening of the muscles of the shoulders and upper limbs came to the clinic. The patient had numerous, clearly limited, round, subcutaneous fat masses protruding above the body surface. These changes were arranged symmetrically on the neck, shoulders, upper torso, and the proximal part of the upper limbs. The patient had a pseudoathletic look, and the fatty tissue around the neck formed a typical “Madelung’s collar”. In an interview, the patient admitted that he had been abusing alcohol for 39 years. However, 9 months earlier, he was subjected to tests, on the basis of which he was diagnosed with alcohol-induced decompensated liver cirrhosis. At the time of admission, the calculated patient body mass index (BMI) was 24.7 kg/m2, with a waist circumference of 81 cm. The patient was not diagnosed with overweight or obesity, and biochemical tests did not show disturbances in either lipid or coagulation parameters. However, it was noticed that gynecomastia, limb muscle abnormalities, and hepatosplenomegaly occurred in the examined man. Laboratory tests showed the following disorders: hypochromic anemia (hemoglobin 11 g/dL, red blood cell count 3,900 × 106/mL) neutropenia (1.3×103/µL), thrombocytopenia (100×103/µL), and slightly elevated hepatic (AST: 130 U/L and ALT: 90 U/L) and pancreatic (lipase: 170 U/L and amylase: 140 U/L) enzymes. The pictures of the patient with the described deformities are shown in .
Endocrine workup showed abnormalities. Hyperestro-genism was confirmed with normal testosterone levels and decreased dehydroepiandrosterone sulfate (DHEA-S) levels. The patient was diagnosed with type 2 diabetes based on an oral glucose tolerance test. The results of additionally tested parameters, ie, insulin, C-peptide, and thyroid hormones, were within the reference values. Finally, the patient was diagnosed with a rare disorder of fat proliferation, which is called Madelung’s disease. It was found that the disease phenotype presented by the man corresponds to type 1 according to the EnziCitation6 classification. The patient underwent computed tomography to visualize the structure of lesions and determine their location. The study also allowed to determine the degree of penetration of fat masses to deeper structures. Based on the history, clinical status, and examinations, it was decided to qualify the patient for surgical treatment. Surgical resection of excess adipose tissue was performed. In the postoperative period, there were no complications, and the patient’s well-being was assessed as good. The patient remained under observation for 3 years without recurrence.
Discussion
Madelung’s disease was first described in the year 1846 by BrodieCitation17 and then, in 1888, it was also described by Madelung.Citation18 In 1898, French physicians Launois and Bensaude19 published the characteristics of this disease based on a group of 65 patients. According to the data for 2012, there are >270 cases of Madelung’s disease in the literature.Citation20 Chen et alCitation21 summarized the clinical data of the cases described in the literature in the years 2000–2015 ().
Table 1 Summary of the clinical data of 41 literature sources of Madelung’s disease from 2000 to 2015, with complete material on treatment
Madelung’s disease remains a disorder of unexplained etiology and unclear pathogenesis.Citation1 The distribution and type of adipocytes in patients with Madelung’s disease resemble the brown adipose tissue (BAT) of infants.Citation5,Citation8,Citation11 In patients, instead of increasing the size of existing fat cells, new ones appear.Citation7 The results of a long-term study, in which 7 patients were observed over a period of 12 years, confirm the hypothesis that lipomas formed in the course of the disease are the result of mitochondrial disorders of BAT.Citation12,Citation22 Other authors also indicate that disorders of proliferation and differentiation of human BAT cells underlie the described disease.Citation1,Citation4,Citation10
There are studies that reveal the relationship of Madelung’s disease with diabetes, hyperlipidemia, hypertension, or liver disease. However, the influence of excess body fat on the metabolism of the body is still under discussion.Citation1 Regardless of this, people with Madelung’s disease often have coexistence of other disorders ().
This is confirmed by the described case, in which the patient shows the occurrence of diabetes, hepatosplenomegaly, cirrhosis, and gynecomastia simultaneously with Madelung’s disease. Apart from these disorders, sensory, motor, and autonomic polyneuropathy is additionally observed in approximately 85% of patients with Madelung’s disease.Citation9,Citation12
One of the main factors for the development of this disease is alcohol abuse. Alcohol adversely affects the enzymatic processes in the mitochondria and disrupts adrenergic lipolysis – it can be a cofactor inducing a change in the number and function of β-adrenergic receptors. It is likely that alcohol abuse is the cause of uncontrolled accumulation of adipose tissue in various parts of the body.Citation3,Citation7,Citation11 The described case also presents a long history of consuming excessive amounts of alcohol. The literature describes only a few cases of Madelung’s disease without alcohol in the patient’s diet.Citation24 Other possible risk factors include nicotine abuse, metabolic disorders, and malignant tumors.Citation4
Most likely, there is genetic predisposition based on matrilineal inheritance.Citation1,Citation2,Citation4,Citation9 It is recognized that the disease may be inherited in an autosomal dominant manner with variable mitochondrial DNA penetration.Citation3,Citation8,Citation10,Citation12
Archeological discoveries suggest that there may be an inherited tendency for Madelung’s disease – perpetuated for centuries – among the population of people living in the Mediterranean. This may be evidenced by a statue known as the Capestrano warrior from the 6th century BC and discovered in Italy. It presents an impressive figure with a unique somatic aspect, characterized by large hips and broad shoulders. The silhouette of the Capestrano warrior is very similar to the appearance of a patient with Madelung’s disease. This convergence may be accidental and may also indicate the genetic basis of the occurrence of this disease.Citation25
A case report of a familial Madelung disease in siblings, ie, a 41-year-old woman and her 36-year-old brother, has been described in the literature. In molecular studies, the existence of mutations in the lipase-encoding gene has been demonstrated in both patients.Citation26 In the studies carried out so far, Madelung’s disease is associated with point mutations in mitochondrial DNA, whose genes are important in the regulation of lipolytic pathway processes.Citation1,Citation22 A relationship between the described disease and the occurrence of myoclonic epilepsy and shred of red fibers has also been established.Citation1 In the muscles of patients with Madelung’s disease, the occurrence of radiant red fibers is often found, which indicates mitochondrial dysfunction with reduced cytochrome c oxidase activity.Citation2,Citation10,Citation11
The local defect of catecholamine-induced lipolysis, adrenal adrenoceptor defects, and the reduction of inducible nitric oxide synthase (iNOS) are potential causes of Madelung’s disease. The implication of these processes is increased adipo-genesis.Citation1,Citation3,Citation9,Citation10 In addition, recently conducted molecular studies using next-generation sequencing have also demonstrated the existence of genetically diverse genes in patients with Madelung’s disease compared to healthy controls.Citation1
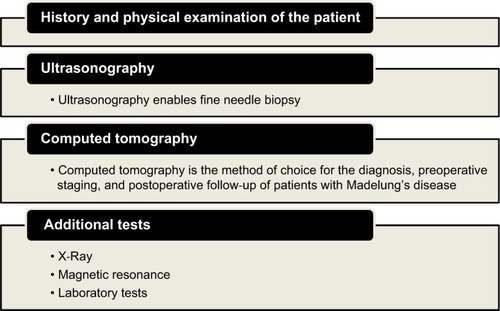
The diagnosis of Madelung’s disease is based on history, clinical appearance of the patient, and the results of imaging examinations ().
The disease should be differentiated from morbid obesity, Cushing’s syndrome, salivary gland disease, lymphoma, Froelich’s syndrome, angiolipomatosis, myxoid liposarcoma, encapsulated lipomas, neurofibromatosis, and lipomatosis in patients infected with HIV.Citation4,Citation12 The disease progresses rapidly in the first few years, after which the progression usually slows down or the size of the created adipose tissue mass stabilizes.Citation3,Citation8
The therapeutic approach in Madelung’s disease is reduced to palliative treatment, which includes surgical resection of the adipose tissue, liposuction, or injection lipolysis.Citation1–Citation4 It seems reasonable to correct metabolic disorders and overweight.Citation3 Alcohol withdrawal and weight loss may be helpful in controlling the disease, but they do not guarantee the inhibition of its progression.Citation1,Citation3,Citation16 Surgical procedures are time consuming – often divided into several stages – due to the volume of fat mass, as well as their spread and infiltration into neighboring tissues.Citation3,Citation4 Conventional surgery is recommended, especially in heavily vascularized and innervated regions, as well as in violation of patency of the airways and esophagus.Citation3,Citation13 The efficacy of surgical treatment or liposuction is limited.Citation1,Citation14 It is estimated that nearly 63% of patients experience recurrence after surgical resection of adipose tissue, while in the case of liposuction, up to 95% of patients experience recurrence.Citation1,Citation8,Citation16 After injection lipolysis, fibrosis and adhesions form. This impedes surgical treatment or liposuction in the recurrence of lesions.Citation11 Despite frequent relapses, functional and cosmetic effects obtained in surgical treatment can be satisfactory.Citation4 Unfortunately, no effective pharmacotherapy has been developed so far in the treatment of Madelung’s disease. The use of salbutamol for adrenergically stimulating lipolysis and thus inhibiting the progression of the disease in larger clinical trials did not show the expected effect.Citation8,Citation12,Citation16
Conclusion
Madelung’s disease – apart from the essential excessive accumulation of adipose tissue – is characterized by the occurrence of numerous metabolic disorders. In the literature, the authors describe the coexistence, among others, of carbohydrate, lipid, or hormonal disorders along with the disorder in question. Diagnosis of diabetes and abnormal levels of sex hormones in the presented case are the confirmation.
The described case also confirms the role of excessive alcohol consumption in the pathogenesis of the disease. In contrast, impaired liver function – occurring in the majority of patients with Madelung’s disease – may have a greater impact on the metabolic abnormalities than the pathology of adipose tissue alone.
Madelung’s disease is rarely diagnosed, which may not necessarily be due to the low incidence of this disease but may be associated with the diagnostic and therapeutic difficulties, as well as with the availability of few literature reports, often related to individual cases.
Consent for publication
The patient provided written informed consent for publication of the clinical details and images.
Disclosure
The authors report no conflicts of interest in this work.
References
- Chen K Wang L Yang W Wang C Hu G Mo Z Profiling of differentially expressed genes in adipose tissues of multiple symmetric lipomatosis Mol Med Rep 2017 16 5 6570 6579 28901441
- Nisi G Sisti A Images in clinical medicine. Madelung’s disease N Engl J Med 2016 374 6 572 26863358
- El Ouahabi H Doubi S Lahlou K Boujraf S Ajdi F Launois-Bensaude syndrome: a benign symmetric lipomatosis without alcohol association Ann Afr Med 2017 16 1 33 34 28300050
- Ardeleanu V Chicos S Georgescu C Tutunaru D Multiple benign symmetric lipomatosis – a differential diagnosis of obesity Chirurgia 2013 108 4 580 583 23958107
- Prahlow SP Kosciuk P Prahlow JA Multiple symmetric lipomatosis J Forensic Sci 2018 63 1 312 315 28643398
- Enzi G Multiple symmetric lipomatosis: an updated clinical report Medicine 1984 63 1 56 64 6318013
- Zielińska-Kaźmierska B Lewicki M Manowska B Madelung disease Advances in Dermatology and Allergology 2015 5 400 403
- Jang JH Lee A Han SA Ryu JK Song JY Lipomatosis MS Multiple Symmetric Lipomatosis (Madelung’s Disease) Presenting as Bilateral Huge Gynecomastia J Breast Cancer 2014 17 4 397 400 25548590
- Yeh NC Yang CY Chou CW Yen FC Lee SY Tien KJ Madelung’s disease J Clin Endocrinol Metab 2012 97 9 3012 3013 22701018
- Enzi G Busetto L Sergi G Multiple symmetric lipomatosis: a rare disease and its possible links to brown adipose tissue Nutr Metab Cardiovasc Dis 2015 25 4 347 353 25770761
- Wollina U Heinig B Madelung’s Disease – Case Series and Treatment by Tumescent Liposuction or Lipectomy Open Access Maced J Med Sci 2017 5 4 427 431 28785324
- Esposito AC Munhoz T Abbade LP Miot HA Do you know this syndrome? Type 2 benign symmetric lipomatosis (Launois-Bensaude) An Bras Dermatol 2016 91 6 840 841 28099616
- Chen HW Chen HW Chen HL Lai CC Madelung Disease Am J Med Sci 2016 352 6 654 27916224
- Pinto CI Carvalho PJ Correia MM Madelung’s Disease: Revision of 59 Surgical Cases Aesthetic Plast Surg 2017 41 2 359 368 28032179
- Landis MS Etemad-Rezai R Shetty K Goldszmidt M Case 143: Madelung disease Radiology 2009 250 3 951 954 19244057
- Brea-García B Cameselle-Teijeiro J Couto-González I Taboada-Suárez A González-Álvarez E Madelung’s disease: comorbidities, fatty mass distribution, and response to treatment of 22 patients Aesthetic Plast Surg 2013 37 2 409 416 23435503
- Brodie BC Clinical Lectures on Surgery delivered at St. George’s Hospital Am J Med Sci 1846 11 22 437
- Madelung OW Ueber den Fetthals Arch Klin Chir 1888 37 106 130
- Launois PE Bensaude R De l’adenolipomatose symetriqe Bull Mem Soc Med Hop Paris 1898 1 298
- Persici Rodrigues L Lima Araujo Melo E. Madelung’s disease: a case report and literature review Radiol Bras 2012 45 2
- Chen CY Fang QQ Wang XF Madelung’s Disease: Lipectomy or Liposuction? Biomed Res Int 2018 2018 21 3975974 29682541
- Plummer C Spring PJ Marotta R Multiple Symmetrical Lipomatosis – a mitochondrial disorder of brown fat Mitochondrion 2013 13 4 269 276 23524250
- Enzi G Busetto L Ceschin E Coin A Digito M Pigozzo S Multiple symmetric lipomatosis: clinical aspects and outcome in a long-term longitudinal study Int J Obes Relat Metab Disord 2002 26 2 253 261 11850759
- Bergler-Czop B Wcisło-Dziadecka D Brzezińska-Wcisło L Madelung’s disease in a patient with chronic renal insufficiency: a case report and review of literature Poste˛py Dermatol Alergol 2014 31 121 124
- Feliciani C Amerio P Images in clinical medicine. Madelung’s disease: inherited from an ancient Mediterranean population? N Engl J Med 1999 340 19 1481 10320387
- Zolotov S Xing C Mahamid R Shalata A Sheikh-Ahmad M Garg A Homozygous LIPE mutation in siblings with multiple symmetric lipomatosis, partial lipodystrophy, and myopathy Am J Med Genet A 2017 173 1 190 194 27862896