Abstract
Laparoscopic sleeve gastrectomy (LSG) is an effective treatment option in patients with morbid obesity, with rare long-term sideeffects. In this report, we present a 42-year-old woman who reported positional vertigo and unilateral gradual hearing loss plus continuous tinnitus after LSG. The patient had no signs or symptoms of mental health disorders and the results of the haematological and serum biochemical tests were normal. However, audiometric test revealed mild sensorineural hearing loss with magnitude in high-frequency tones. Also, acoustic reflex threshold showed neural pathway damage, particularly at high frequencies, with no reflex. Pure tone audiometry showed signs of nerve damage in the inner ear. One possible justification for these complications might be eustachian tube dysfunction due to muscle relaxation. Muscle relaxation itself may occur as a result of adipose tissue loss around the ear muscles. Further evidence, however, would be required to better determine whether these complications are attributable to LSG, and to illuminate exact underlying reasons for such complications.
Introduction
Obesity is a major health problem worldwide.Citation1,Citation2 Laparoscopic sleeve gastrectomy (LSG) is an effective treatment for morbid obesity, with beneficial effects on body weight reported in both the short and long term.Citation3,Citation4 Although the procedure is generally known to be safe, it may cause a number of side effects, including anastomotic leaks, hemorrhage, postoperative abscess, and sleeve stricture.Citation5 Hearing impairments, however, is rarely reported after LSG. In this case report, we describe a 42-year-old woman with a chief complaint of positional vertigo, unilateral gradual hearing loss, and continues tinnitus after LSG.
Case Report
A 42-year-old woman was admitted to the Ear, Nose and Throat ward of Shariati educational hospital (Tehran, Iran) complaining from positional vertigo, unilateral gradual hearing loss, and continues tinnitus. Except a history of recent LSG for her morbid obesity, the patient had no other medical or psychological condition, including depressive disorder, bulimia nervosa, excessive consumption of coffee or alcohol, and smoking. Before the LSG, patient’s weight, height, and body mass index (BMI) were 110 kg, 164 cm, and 40 kg/m2, respectively. In months three and twelve after surgery, the BMI decreased to 33 and 27 kg/m2, respectively.
In month three post-surgery, the patient reported vertigo and hearing. At the beginning, both symptoms were mild, but they aggravated gradually, leading to intolerable vertigo and complete unilateral hearing loss at month 12. In month 12, the patient also developed a number of minor complications, including menstrual irregularities, female androgenetic alopecia, and appetite alteration. She reported an increased desire to salty and sour tastes, and a decreased desire to sweet foods.
The patient’s positional vertigo was getting intensified in the natural head position, i.e., when the head was in an upright position, with eyes looking straight, and got alleviated when the patient tilted her head to the right/left side. The Dix-Hallpike maneuver did not illuminate possible causes of positional vertigo and the eye motion test was also normal.
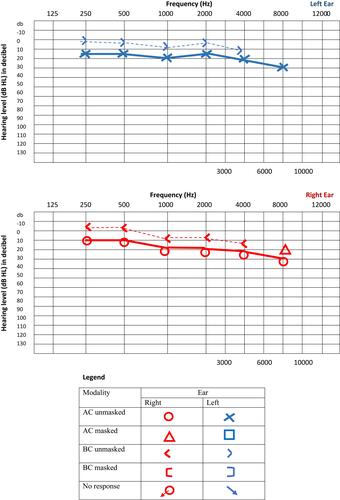
Unilateral hearing loss aggravated over a nine-month period. No trigger/causes were detected that could alleviate/aggravate the progression of the problem. The patients reported no history of head trauma, headache, migraine, dizziness, nausea/vomiting, recent infection, recent loud noise exposure, ear pain/discharge, or numbness. The otoscopy result was normal. Rinne and Weber tests also showed normal bone conduction in the absence of air conduction. The tympanogram was classified as type A in both right and left ears, and was considered to be normal. Audiometric test showed mild sensorineural hearing loss with magnitude in high-frequency tones. Acoustic reflex threshold showed Eustachian tube dysfunction. At high frequencies, the neural pathways also showed no reflex. Outer and middle ear curtain was normal in pure-tone audiometry. The test, however, showed nerve damage in the inner ear (). During a 14-month follow-up, the abovementioned symptoms alleviated by symptomatic therapy, without specific medical interventions.
Discussion
Clinical complications rarely occur after sleeve gastrectomy. In this case report, we presented a woman who suffered from positional vertigo and unilateral gradual hearing loss plus continues tinnitus after LSG. These complications can occur after sleeve gastrectomy but sever forms that become intolerable or impact patients’ daily life have been rarely reported to date.Citation6–Citation8 One possible mechanism might involve the relaxation of ear muscles due to the loss of surrounding adipose tissues. In adult humans, the eustachian tube contains a 24–26 millimeters fibrocartilaginous part. Due to the elastic nature of the fibrocartilaginous part, it is closed most of the time. It only allows the air to pass through during activities such as sneezing, yawning, or swallowing.Citation9–Citation11 The exact process involved in the opening of the fibrocartilaginous part has yet to be defined. It is suggested that muscular structures such as tensor veli palatini, elevator veli palatine and salpingopharyngeus muscles play an important part in this regard.Citation8,Citation11 Besides the dysfunction of peritubalmuscles, loss of Ostmann’s fat surrounding the muscles of the eustachian tube is among the potential mechanisms implicated in the pathophysiology of hearing loss induced by eustachian tube dysfunction.Citation7 Studies showed that rapid weight lost following sleeve surgery may be associated with loss of adipocyte tissue around the eustachian tube, resulting in hearing loss and tinnitus.Citation7,Citation12
We also did no measure micronutrient levels of the patient, either before or after LSG. Micronutrient deficiencies might play a role in the development of vertigo through mechanisms such as neural impairments and decreased blood flow to the brain.Citation13,Citation14
Further reports are required to determine whether these complications are etiologically linked to LSG. Positive associations would have certain implications for the clinical management of patients who undergo LSG.
Conclusion
The complications associated with sleeve gastrectomy are rare; however, hearing loss may occur due to the relaxation of ear muscles following the loss of surrounding adipose tissues. Further cases with similar complications would better illuminate possible linkages between sleeve gastrectomy and subsequent hearing complications, including hearing loss and vertigo. Confirmed associations would have important implications for the clinical management of patients after sleeve gastrectomy.
Patient Consent
The authors confirm that written informed consent has been secured from the patient to publish the findings of this case study. No institutional approval was required for reporting this case report.
Author Contributions
All authors contributed to acquisition of data, analysis and interpretation of data, drafting or revising the article, gave final approval of the manuscript to be published, and agree to be accountable for all aspects of the study.
Acknowledgment
This case report was part of the work by Mohsen Tabasi to fulfill the requirement for a PhD degree. The authors would like to express their gratitude to nursing of Shariati Hospital of Tehran, Iran for their technical assistance in this project.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA. 2018;319(16):1723–1725. doi:10.1001/jama.2018.3060
- Saadatifar H, Ostadimoghaddam H, Khoshhal F, et al. The prevalence of obesity and overweight in Northeastern Iran. Asian J Med Sci. 2018;4(1):1–10.
- Jiménez A, Casamitjana R, Flores L, et al. Long-term effects of sleeve gastrectomy and Roux-en-Y gastric bypass surgery on Type 2 diabetes mellitus in morbidly obese subjects. Ann Surg. 2012;256(6):1023–1029. doi:10.1097/SLA.0b013e318262ee6b
- Tabasi M, Ashrafian F, Khezerloo JK, et al. Changes in Gut Microbiota and hormones after bariatric surgery: a bench-to-bedside review. Obes Surg. 2019;29(5):1663–1674. doi:10.1007/s11695-019-03779-7
- Lalor PF, Tucker ON, Szomstein S, Rosenthal RJ. Complications after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2008;4(1):33–38. doi:10.1016/j.soard.2007.08.015
- Al-Shawi Y, Ismail A, Almegil N, Al-Soqairy M. The effects of obesity on the Eustachian tube function in Saudi Adults (a cross-sectional study). Glob J Otol. 2017;9(5):555772.
- Muñoz D, Aedo C, Der C. Patulous eustachian tube in bariatric surgery patients. Otolaryngol Head Neck Surg. 2010;143:521–524. doi:10.1016/j.otohns.2010.07.004
- Pascoto G, Abreu C, Silva ML, Weber R, Pignatari SS, Stamm A. The impact of acute loss of weight on Eustachian tube function. Int Arch Otorhinolaryngol. 2014;18:376–379. doi:10.1055/s-00025477
- Poe DS. Diagnosis and management of the patulous eustachian tube. Otol Neurotol. 2007;28(5):668–677. doi:10.1097/mao.0b013e31804d4998
- Seibert JW, Danner CJ. Eustachian tube function and the middle ear. Otolaryngol Clin North Am. 2006;39(6):1221–1235. doi:10.1016/j.otc.2006.08.011
- Caldas SN, Mello JF, Martins RH, Costa SS. Treaty of Otorhinolaryngology and Cervicofacial Surgery [Tratado de Otorrinolaringologia e Cirurgia Cervicofacial]. Chap. 2011;14:260–261.
- Yoshida H, Kobayashi T, Takasaki K, et al. Imaging of the patulous Eustachian tube: high-resolution CT evaluation with multiplanar reconstruction technique. Acta Otolaryngol. 2004;124:918–923. doi:10.1080/00016480410017422
- Büki B, Ecker M, Jünger H, Lundberg YW. Vitamin D deficiency and benign paroxysmal positioning vertigo. Med Hypotheses. 2013;80(2):201–204. doi:10.1016/j.mehy.2012.11.029
- Aydın E, Babakurban ST, Özgirgin ON, Özlüoğlu LN. The relationship of homocysteine, vitamin B12, folic acid levels with vertigo. Kulak Burun Bogaz Ihtis Derg. 2012;22(4):214–218. doi:10.5606/kbbihtisas.2012.041