Abstract
Objective
This study is aimed to determine the metabolomic effects of the hybrid medicine formula Yi-Qi-Bu-Shen (YQBS) on the neurotransmitter aspects of cognitive impairment in diabetic rats.
Methods
In the current study, streptozotocin (STZ) was used to induce diabetic animal model in male Sprague Dawley (SD) rats. After successful establishment of diabetic SD rats’ model, age-matched healthy SD rats and diabetic SD rats were treated with low and high doses of YQBS, and then tested for learning memory ability and analyzed for pathological changes. In addition, neurotransmitter metabolic changes in hippocampal subdivisions of rats from different treated groups were analyzed using liquid chromatography-mass spectrometry (LC-MS) technique.
Results
YQBS could significantly improve memory-cognitive impairment in diabetic rats as evidenced by the shortening of latency to target and the reduction of latency first entrance to target. Moreover, YQBS also improved the pathological alterations in the hippocampal region in the brains of diabetic rats. Metabolomic analysis showed that the expression of noradrenaline hydrochloride was down-regulated and the expressions of levodopa and 5-hydroxytryptophan were up-regulated in the hippocampal tissues of diabetic rats treated with YQBS.
Conclusion
These findings demonstrate that YQBS has protective effects against diabetic cognitive dysfunction, which might act through alteration in tyrosine and tryptophan metabolism.
Introduction
Improved health conditions, medical advances, and social development have made chronic non-communicable diseases, one of the major disease problems nowadays. Diabetes, a chronic metabolic disease, has long been a hot issue of concern worldwide as it inflicts a large population and manifests extensive systemic complications. The number of people with diabetes has increased from 151 million in 2000 to 537 million in 2021 and is expected to grow to 783 million by 2045.Citation1 As a systemic disease, the complications associated with diabetes cover a wide range of systems, including circulatory, urinary, and neurological. A growing number of clinical studies have shown a strong link between diabetes and cognitive dysfunction.Citation2–6 The cognitive impairment that accompanies diabetes often manifests as asymptomatic preclinical, mild cognitive dysfunction and prevalence of dementia stages.Citation7 Patients either have pathological, structural, and functional changes in the brain without an objective neuropsychological assessment of abnormalities or exhibit cognitive impairment that severely affects their daily work and life. Therefore, it is essential to search for effective drugs that can treat this disease.
Traditional Chinese medicine (TCM) has a unique theory of disease understanding. According to TCM, diabetic cognitive dysfunction is a combination of consumptive thirst and dementia. Although the affected area of the disease is in the brain, pathogenesis lies in kidney deficiency, resulting in blood and fluid disorders. The resulting turbid phlegm and static blood are both pathological products and pathological factors. The hybrid medicine formula YQBS is composed of Astragali Radix, Rehmanniae Radix Praeparata, Polygonati Rhizoma, Lycii Fructus, Epimedii Folium, Puerariae Lobatae Radix, Chuanxiong Rhizoma, Atractylodis Rhizoma, and Coptidis Rhizoma, which are mainly used to invigorate the kidney and also to activate blood circulation and eliminate phlegm.Citation8 Previous limited evidence has suggested the potential therapeutic effect of YQBS on patients with diabetic cognitive dysfunction by lowering their blood glucose and improving their memory, by protecting hippocampal neuronal cells from damage, and by a protective effect on the electrophysiological function of the brain in diabetic rats.Citation8,Citation9 Herein we performed comprehensive analyses to determine the protective effects of YQBS on cognitive dysfunction under diabetic condition and also elucidated the underlying mechanism through characterizing the metabolic neurotransmitters in the hippocampus.
Materials and Methods
Animals
Forty male Sprague Dawley (SD) healthy rats (8 weeks old) were purchased from SiPeiFu (Beijing) Biotechnology Co., Ltd. All rats were kept at SPF grade in the Experimental Animal Center of Qilu Hospital, Shandong University, with free access to animal maintenance chow and sterile water. The rats were housed under the following environmental conditions: alternating 12h/12h light and dark time, 22±2℃, and 30~40% humidity. All animal experimental protocols were performed in accordance with the guidelines for experimental animal husbandry management and approved by the Experimental Animal Welfare Ethics Committee of Qilu Hospital, Shandong University.
Preparation of Extracts of YQBS
The composition of YQBS extract is identical with the previous study, which is composed of nine crude drug materials, including Astragalus membranaceus (Fisch.) Bge. var. mongholicus (Bge.) Hsiao (15 g), Rehmannia glutinosa Libosch (12 g), Polygonatum sibiricum Red (10 g), Ligusticum chuanxiong Hort (6 g), Lycium barbarum L (6 g), Epimedium brevicornum Maxim (9 g), Atractylodes lancea (Thunb.) DC (3 g), Pueraria lobata (Willd.) Ohwi (12 g), Coptis chinensis Franch (3 g).Citation8 All nine Chinese herbs in YQBS were provided by Shandong Bokang Traditional Chinese Medicine Co. Ltd. (Qingzhou, China). The above nine crude drugs were decocted and made into powder followed by adding 20 times the amount of water to decoct and concentrate all the drugs 3 times, 2 h each time. Next, the nine drugs-soup was concentrated to a thick paste, and then put into a vacuum drying box with a constant temperature of 80℃ for drying and pulverizing. After it is cooled down and then moved into a refrigerator at 4℃ for storage. Each gram of YQBS dry powder is equivalent to 2.88g of the original medicinal material. The dried powder can be dissolved in sterile water for experiment according to the required dosage whenever it is needed.
Grouping and Management
Diabetes is induced by STZ, a glucosamine–nitrosourea compound derived from Streptomyces achromogenes, and has best been demonstrated in mouse and rat models.Citation8,Citation10,Citation11 In the present study, 8-weeks-old male SD rats injected intraperitoneally with 1% STZ (55 mg/kg) solution after fasting 12 h from water were used to induce diabetic model. Same-gender age-matched SD rats injected with sodium citrate buffer, which was used to dilute STZ, were used as negative control (NC). Eight rats in each experimental group. One week after induction with STZ, the blood glucose of the tail vein from the induced rats was measured. Rats with blood glucose ≥16.7 mmol/L were regarded as successful diabetes models, according to a previous study.Citation8 Afterwards, the identified diabetic rats (DM) were orally administered with low dose YQBS at 200 mg/kg/day (L) or high dose YQBS at 800 mg/kg/day (H) for 8 weeks according to the working dose of YQBS (600 mg/kg) in previous diabetic rat model,Citation8 and the DM rats gavaged with sterile water were used as control. Body weight and blood glucose were measured in each group every 2 weeks after successful modeling.
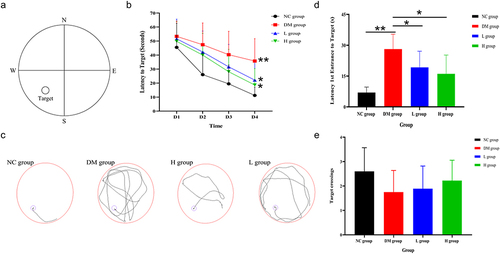
Morris Water Maze Test
The learning and memory abilities of rats in NC, DM, L, and H groups were assessed by the Morris water maze (MWM) experiment after 8 weeks of gavage. According to the literature,Citation12–14 briefly, the water maze consisted of a black circular pool with inner walls (diameter 160 cm, height 50 cm), a transparent circular (invisible) platform (diameter 12 cm, height 20 cm), a camera, and a fully automatic analysis system. The water temperature in the pool was 21±2℃, and the water surface was 1~2 cm above the platform. The pool was artificially divided into four quadrants, and the transparent circular platform was fixed and located in the center of the southwest quadrant (). A block session consisted of four experiments was conducted daily. The rats were placed in the water facing the wall of the pool at four different starting points: north, east, southeast, and northwest, and allowed to swim and find the invisible platform in the water within 60-seconds (s). If the rats failed to find the platform and boarded the platform to stay within the 60s, they were artificially guided to the platform and stayed in the platform for 15s. After 4 consecutive days, the transparent platform was removed from the pool and a visible platform was plated in another position of the pool, the rats were placed in the water in the northeast quadrant at the farthest distance from the platform, and their swimming trajectory was tracked within 60s. The latency time is from the first entrance to the visible platform, and the platform crossings were recorded.
Figure 1 Learning cognitive test in YQBS treated or untreated STZ-induced diabetic rats using MWM. (a) Schematic diagram of water maze quadrant division. (b) Results of the latency period of evasion in each group of rats. (c) Trajectory diagram of each group of rats. (d and e) are results of the first crossing time and the number of the crossing time of the platform in each group of rats, respectively. n= 8per group. Data are mean ± SE; *Represents the comparison between YQBS group and DM group. **Represents the comparison between DM group and NC group. * p< 0.05, ** p< 0.01.
Pathological Observation of Hippocampal Tissue in the Brain
The pathology of the hippocampal tissues of each group of rats is analyzed using hematoxylin–eosin (H&E) staining. After the MWM test, the rats were sacrificed and the brains were collected, and then the right-half brain was fixed in 4% paraformaldehyde fixation. After rinsing, dewaxing, and embedding, the brain tissues were cut into 5 μm sections, and then H&E staining was performed to observe the histopathological changes.
Sample Preparation for the Metabolomics Analysis Using Liquid Chromatography-Mass Spectrometry (LC-MS)
After the MWM test, the hippocampal tissues on the left side of the brain were removed from the rats on ice and then frozen in a −80℃ refrigerator for LC-MS analysis after brain severance. 600 μL solution of 10% formic acid methanol solution-water (1:1, V/V) was added to the sample, followed by adding two steel beads. The samples were vortexed and shaken for 30s, and then transferred into a tissue grinder at 55Hz for 60s. After centrifugation at 12,000 rpm for 5 min at 4℃, 100 μL of the supernatant was collected and mixed with 100 μL of a double isotope internal standard at a concentration of 10 ppb, and then vortexed and shaken for 30s, followed by filtration through a 0.22 μm membrane. This filtrate was used as a sample for low concentration substance detection. 10 μL of the original supernatant was mixed with 690 μL 10% formic acid-methanol-water (1:1, V/V) solution and vortex shaken for 30s. After vortex shaking, 100 μL of the diluted sample was further mixed with 100μL of double isotope internal standard at 10 ppb, and vortex shaken for 30s. The resultant supernatant was filtered through a 0.22 μm membrane; this filtrate was used as a sample for high concentration substance detection.
Instrument Conditions for the LC-MS Analysis
A ZORBAX Eclipse XDB-C18 column (4.6×150mm, Agilent, USA) was used with an injection volume of 5μL and a column temperature of 40℃. The mobile phases were A-10% methanolic water (containing 0.1% formic acid) and B-50% methanolic water (containing 0.1% formic acid). The gradient elution conditions were 0~6.5 min, 10%~30% B; 6.5~7 min, 30~100% B; 7~18 min, 100% B; 18~18.5 min, 100~10% B; 18.5~21 min, 10% B; 0~8 min, flow rate 0.3 mL/min; and 8.5~21 min, flow rate 0.4 mL/min. Electrospray ionization (ESI) source was operated in positive ion mode. The ion source temperature was 500℃, the ion source voltage was 5500 V, the collision gas was 6 psi, air curtain gas was 30 psi, and both the nebulizing gas and auxiliary gas were 50 psi. Scanning was performed using multiple reaction monitoring (MRM).
Methodological Validation of the LC-MS Analysis
For each neurotransmitter, the linearity test of the standard curve was in the form of y=ax+b, with the correlation coefficient of r > 0.99; the linearity of the standard curves was within a good linear range. The range of intra-batch precision of neurotransmitters was 1.98%~9.65%, the range of inter-batch precision was 3.22%~13.44%, and the range of total precision was 1.41%~14.75%, which are all less than 15%. The range of stability was 86.81%~115.68%, indicating that storage and handling do not affect the measurable concentration of neurotransmitters. The matrix effect for neurotransmitters ranged from 90% to 114%, and the recovery ranged from 86% to 112%. These results indicate that all of the above meet the relevant requirements for the determination of biological samples.
Statistical Analysis
SPSS 26.0 software was applied for statistical analysis of the data. If the data met normal distribution and the variances were equal, one-way ANOVA was used for comparison among the four groups; Least Significant Difference (LSD) was used for multiple comparisons. For quantitative data, with non-normal distribution, Kruskal Wallis rank sum test was used for comparison among the four groups; Bonferroni method was used for multiple comparisons. For comparison of multiple groups at multiple time points, repeated measures ANOVA was used for comparison, and if the data met the Mauchly test, Sphericity Assumed was used for statistical analysis; if the data did not meet the Mauchly test, Roy’s Largest Root was used for statistical analysis; and for comparison between different groups at the same time point, LSD was used for two-way comparisons. All tests were performed using two-sided tests, and statistical results were presented as mean (Mean) ± standard deviation (SD). Differences were considered statistically significant when p < 0.05.
Results
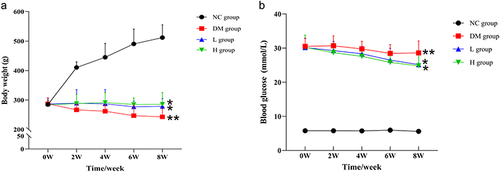
YQBS Increased the Body Weight and Decreased the Blood Glucose Level in STZ-Induced DM Rats
As described above, the rats with blood glucose ≥16.7 mmol/L were regarded as successful diabetes models. Afterwards, the identified diabetic rats (DM) were fed with low dose YQBS at 200 mg/kg/day (L) or high dose YQBS at 800 mg/kg/day (H), according to the working dose in the previous study,Citation8 for 8 weeks. DM rats fed with sterile water were used as control. Compared with NC group rats, DM group rats were observed to increase in water consumption, food intake and urine output as well as loose stools, dull fur, and delayed response. In L- and H-does YQBS treated group rats, the same symptoms presented in the DM group were relieved after treatment (observation data not shown).
In addition to observations, the body weight and blood glucose levels of different groups of rats were monitored for 8 weeks from STZ induction. From , it was found that the body weight of rats was no significant difference in each group before STZ induction, while it dramatically decreased after STZ induction compared with NC group. After treatment with YQBS, the body weight increased significantly in both L and H groups compared with control DM group. From , we could see that the blood glucose of rats in DM, H, and L groups was greater than 16.7 mmol/L after STZ induction in comparison with lower than 10 mmol/L in NC group, indicating that the diabetes mellitus model was established successfully in SD rats. After treatment with L- or H-does YQBS, the blood glucose of rats was significantly decreased compared with that in the control DM group.
Figure 2 The body weight and blood glucose in YQBS treated or untreated STZ-induced diabetic rats. 1% STZ (55mg/kg) solution were used to induce rat diabetic model. Age-matched no injection rats were used as negative control (NC). One week after the induction, the identified diabetic rats (DM) were fed with low dose YQBS at 200mg/kg/day (L) or high does YQBS at 800mg/kg/day (H) for 8 weeks. Sterile water were used as control. (a) Body weight analysis in four different rat groups. (b) Blood glucose measurement in each group. n= 8per group. Data are mean ± SE; *Represents the comparison between YQBS group and DM group. **Represents the comparison between DM group and NC group. * p< 0.05, ** p< 0.01.
YQBS Protected the Learning Cognitive Impairment in STZ-Induced DM Rats
To evaluate the protective effect of YQBS on learning cognitive impairment in diabetic rats, the Morris water maze (MWM) test () was applied to measure the learning and memory abilities of rats from NC, DM, L, and H groups. The results of the 4-day localized navigation experiment showed that the latency of the rats in the DM group was significantly longer than that in the NC group, indicating that the rats in the DM group showed a decrease in learning cognitive ability. In contrast, the L and H groups alleviated the decline in learning cognitive ability after treatment with YQBS, although it did not reach the normal level in the NC group (). The trajectories of the rats in each group in the MWM are shown in . The results of the spatial exploration performed on the end day of the experiment showed that the rats in NC group took the minimum time, while the rats in DM group took the maximum time to enter the target for the first time, and the rats in L and H groups took significantly less time to enter the target compared with DM group (). The times that rats crossed the platform in four groups were no significant differences ().
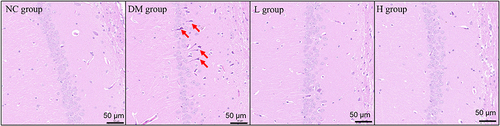
Pathological Effects of YQBS on Hippocampal Tissue in STZ-Induced DM Rats
Since YQBS showed protective effects on the learning cognitive impairment, which reflects the brain function, in STZ-induced DM rats, we next investigated the effects of YQBS on the histology of brain in diabetic rats. Through H&E staining of the hippocampus of the brain tissues, we could see that the neuronal cells in the hippocampal tissue of NC group rats were integrated, including exhibiting dense/full morphology, compact and even arrangement, greater number of cells, in comparison, the neuronal cells in DM group were disordered and scattered as well as with fewer cells and abnormal morphology (indicated by the red arrow) (). After treatment with L- or H-dose YQBS, the neuronal cells in the hippocampus became more numerous, more closely arranged, and the morphology look more normal than those in the DM group ().
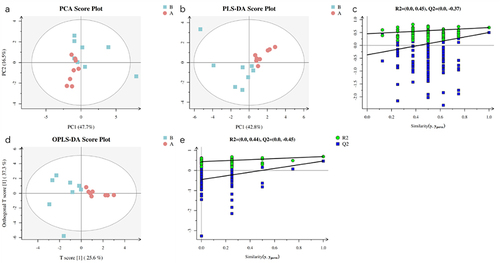
Comparison of the Metabolomics Analysis of Hippocampus in Different Groups
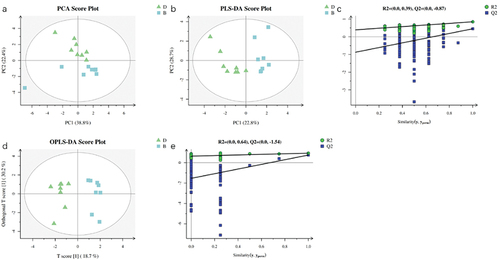
We next did a metabolomics analysis of hippocampus from different groups. shows the metabolomic analysis in NC group and DM group. The Principal Component Analysis (PCA) score plots in shows a clear separation trend between the hippocampal tissues of rats in the NC and DM groups with R2X (cum) = 0.642. Further Partial Least-Squares Discriminant Analysis (PLS-DA) and Orthogonal PLS-DA (OPLS-DA) were also performed, and the separation trend of the two groups was evidenced by the score plots in and , with the main parameters for PLS-DA being R2Y (cum) = 0.692 and Q2 (cum) = 0.498, and OPLS-DA were R2Y (cum) = 0.692 and Q2 (cum) = 0.468, respectively. The intersection of the regression line of Q2 points with the vertical coordinates in the substitution test plots of and was less than 0, suggesting good reliability and no overfitting of the analysis. This analysis indicated that the metabolic profile of hippocampal tissues of rats in the model group induced by STZ has been changed compared with NC group and further confirmed the modeling was successful.
Figure 4 Metabolomics analysis of hippocampus in NC group and DM group using LC-MS. (a) is the PCA score plot. (b and c) are the PLS-DA score plot with replacement test between DM and NC group. (d and e) are the OPLS-DA score plot with replacement test between DM and NC group. Red circles represent the NC group and blue squares represent the DM group. n = 8 per group.
is the metabolomics analysis of hippocampus in L group and DM group. The PCA score plots in shows a clear trend of separation between the hippocampal tissues of rats in the L and DM groups, with R2X (cum) = 0.598. PLS-DA and OPLS-DA were also further performed, and the separation of the two groups was evidenced by the score plots in and , with the main parameters for PLS-DA being R2Y (cum) = 0.847 and Q2 (cum) = 0.642 and OPLS-DA were R2Y (cum) = 0.896 and Q2 (cum) = 0.708, respectively. The intersection of the regression line of Q2 points with the vertical coordinates in the substitution test plots of and was less than 0, suggesting good reliability and no overfitting of the analysis. This analysis indicated that the low-dose YQBS has a moderating effect on neurotransmitters in the hippocampal tissue of diabetic rats.
Figure 5 Metabolomics analysis of hippocampus in L group and DM group using LC-MS. (a) is the PCA score plot. (b and c) are the PLS-DA score plot with replacement test between group L and DM. (d and e) are the OPLS-DA score plot with replacement test between group L and DM. The yellow diamond is the L group, and the blue square is the DM group. n = 8 per group.
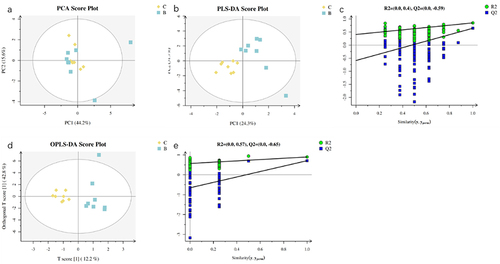
A metabolomics analysis of hippocampus between H and DM groups is shown in . Similarly, with the difference between L and DM groups, the PCA score plots in show a clear trend of separation between the hippocampal tissue of rats in the H and DM groups as well, with R2X (cum) = 0.612. Further PLS-DA and OPLS-DA analysis in and showed that the two groups were clearly separated differently, with the main parameters for PLS-DA being R2Y (cum) = 0.848 and Q2 (cum) = 0.454, OPLS-DA were R2Y (cum) = 0.932 and Q2 (cum) = 0.746, respectively. The intersection of the regression line of Q2 points with the vertical coordinates in the substitution test plots of and was less than 0, indicating the analysis with good reliability and no overfitting. These data indicates that the high-dose of YQBS also has a modulating effect on neurotransmitters in the hippocampal tissue of diabetic rats.
Univariate Analysis
The different expression profile of the neurotransmitter among the H, L, and DM groups was further analyzed using univariate analysis. In comparison with DM group, the expression of levodopa (DOPA) and 5-hydroxytryptophan (5-HTP) was upregulated, and the expression of noradrenaline hydrochloride (NE) was downregulated in the hippocampal tissues of H group; while in L group, the expression of DOPA was up-regulated and NE was down-regulated, and 5-HTP was no change ().
Table 1 Comparison of Neurotransmitter Expression in Hippocampal Tissues Between L- or H-YQBS Treated Group and DM Group
Pathway Analysis
In order to reflect the potential mechanism of the differential metabolites between the DM group and the YQBS treatment group more visually, the pathway analysis was performed using MetaboAnalyst (https://www.metaboanalyst.ca/) to screen the metabolic pathways involved with differential associated neurotransmitters. The results showed that, compared with the DM group, the more associated metabolic pathways in the rats treated with YQBS were mainly Tyrosine metabolism and Tryptophan metabolism ().
Table 2 Associated Metabolic Pathways in Hippocampal Tissues in DM Group and YQBS Treated Groups
Discussion
STZ is widely used in animal experiments as a chemical agent that can induce changes in the structure and function of animal models of diabetes similar to those observed in human diabetes.Citation10 In STZ-induced animal models, cognitive impairment is also frequently observed,Citation11 and structural and functional alterations are often observed in the hippocampus, which is a key area for memory and learning in the cerebral cortex.Citation15–18 Neurotransmitters play an important role as endogenous chemicals that transmit excitation or inhibition between neurons, which can modulate learning and memory; therefore, neurotransmitters in the brain are often disrupted when cognitive impairment occurs in animal models of diabetes.Citation19,Citation20
Herbal formulas often lead to miraculous effects on the treatment of diseases because of the complicated interactions between the molecules. Current treatment for diabetic cognitive dysfunction is mostly based on glucose regulation accompanied by additional drugs, such as cholinesterase inhibitors and N-methyl-D-aspartate antagonists.Citation4 However, it is noted that these drugs have no effect on mild neurocognitive impairment,Citation4 one of the scopes of cognitive impairment in diabetes.Citation7 Therefore, hybrid medicine formula might play an integral role in treating the diseases.Citation21–25 YQBS exhibits a variety of biological effects.Citation8,Citation9,Citation26,Citation27 Especially Astragali, the main component of the YQBS, showed anti-oxidation and anti-diabetic effects,Citation28–30 such as Astragalus polysaccharide ameliorated hyperglycemia, improved insulin resistance and sensitivity, increased the glucose uptake level et alCitation31–33 Consistently, in the current study, YQBS was shown to increase the body weight and decrease the blood glucose in the diabetic rats compared with the control group. The MWM results showed that YQBS improved the cognitive memory level of diabetic rats, which was further confirmed by the pathological analysis. Besides Astragali, other contents of YQBS, such as Barbary Wolfberry Fruit, Pueraria, Coptis Root and their bioactive ingredients also contributed to decreasing insulin resistance and protecting against neuronal injury.Citation34,Citation35 Therefore, the anti-diabetic effect of YQBS might be due to the synergistic effects of all its active ingredients. In addition, the current study first investigated the metabolic effects of YQBS on neurotransmitters in the hippocampus of diabetic rats using metabolomics techniques. The analysis showed that the metabolites of the diabetic rats were significantly different from those in the normal rats, importantly, YQBS showed therapeutic effects on neurotransmitters in the hippocampus of diabetic rats.
The noradrenergic system is closely related to the nervous system and plays an important role in different ways, such as selective attention, memory storage and extraction.Citation36–39 A retrospective study of patients with Alzheimer’s disease showed an association between cognition level and norepinephrine levels in the plasma and cerebrospinal fluid.Citation40 The elevated norepinephrine levels in the plasma might result from the overproduction of norepinephrine in the central nervous system, which might destroy the blood–brain barrier and lead to the flow of norepinephrine from the brain into the bloodstream along with the cerebrospinal fluid.Citation40 Many studies have shown that the abnormalities in the structure and function of noradrenergic neurons are associated with the pathology of Alzheimer’s disease, such as tau phosphorylation.Citation39,Citation41 However, the reports on the amount of norepinephrine in the brain are controversial, some reports suggested that reduced levels of norepinephrine were associated with cognitive impairment,Citation21,Citation42 while others suggested that unchanged or increased levels of norepinephrine were more related to cognitive impairment.Citation41,Citation43–45 One of the current claims is that, in the early stages prior to the onset of neurological diseases, such as Alzheimer’s disease, the abnormal and compensatory hyperactivation of the nucleus coeruleus leads to an overproduction of norepinephrine in the cerebral cortex.Citation40,Citation46 This is consistent with our current results that norepinephrine levels increased in diabetic rats and then decreased after treatment with YQBS.
Meanwhile, current results showed that YQBS could increase levodopa content in the hippocampal tissue of diabetic rats, supporting a positive effect on memory cognition. Several randomized double-blind clinical studies have shown the beneficial effects of levodopa on word memory.Citation47–49 The neurotransmitters measured in the current study can be enriched with tyrosine metabolism, suggesting that YQBS may be able to improve cognitive impairment in rats by regulating the metabolic process of tyrosine. In addition, data in this study also enriched tryptophan metabolism, which is closely related to human learning and cognitive functions. In the case–control study, tryptophan pathway metabolites were increased in the cerebrospinal fluid of Alzheimer’s disease patients compared to healthy subjects.Citation50 In humans, tryptophan metabolism consists of both 5-hydroxytryptophan and kynurenine pathway metabolism, with the majority of tryptophan resulting in kynurenine and only a small fraction, about 1%, of tryptophan, forming 5-hydroxytryptamine (5-HT).Citation51 In the 5-HT pathway, tryptophan is catalyzed to 5-hydroxytryptophan (5-HTP) through tryptophan hydroxylase, which leads to the formation of the neurotransmitter 5-HT. Therefore, the increased dose of YQBS may improve the cognitive function of rats through the 5-hydroxytryptamine pathway.
However, a couple of limitations in the current study were also noted. First, it was suggested that the cognitive disorders of diabetic rats were observed after 8-, 10-, and 12-weeks induction,Citation11 and the cognitive function also needs to be further evaluated after a longer time of diabetic induction. Second, more parameters of MWM, such as the swimming speeds and time spent to find the platform during the four-day test, need to be assayed to comprehensively evaluate the cognitive function. Third, the swimming speeds and time spent in the quadrants in the pool without platform also needs to be evaluated on the following day after the 4-day test.
Conclusions
In conclusion, the present study demonstrates that the hybrid medicine formula YQBS could significantly improve memory-cognitive impairment in diabetic rats as well as improve the pathological alterations in the hippocampal region in the brains of diabetic rats. Analysis of the metabolomic results showed that the expression of noradrenaline hydrochloride was down-regulated and the expression of levodopa and 5-hydroxytryptophan was up-regulated in the hippocampal tissues of diabetic rats treated with YQBS. These findings suggest that YQBS has a protective effect on diabetic cognitive dysfunction and that tyrosine metabolism and tryptophan metabolism may be one of the mechanisms by which YQBS improves diabetic cognitive dysfunction.
Institutional Review Board Statement
The study was approved by the institutional review board at Qilu Hospital, Cheeloo College of Medicine. All animal studies were performed in accordance with institutional guidelines and approved by the Institutional Animal Care and Use Committee of Qilu Hospital, Cheeloo College of Medicine, Shandong University, Jinan, China.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
All authors disclose no conflict of interest.
Acknowledgments
We thank all lab members for the insightful discussions.
Additional information
Funding
References
- IDF Diabetes Atlas. IDF diabetes atlas, 10th edn [EB/OL]; 2021. Available from: https://www.diabetesatlas.org. Accessed March 24, 2023.
- Moheet A, Mangia S, Seaquist ER. Impact of diabetes on cognitive function and brain structure. Ann NY Acad Sci. 2015;1353:60–71. doi:10.1111/nyas.12807
- Shalimova A, Graff B, Gąsecki D, et al. Cognitive dysfunction in type 1 diabetes mellitus. J Clin Endocrinol Metab. 2019;104(6):2239–2249. doi:10.1210/jc.2018-01315
- Srikanth V, Sinclair AJ, Hill-Briggs F, Moran C, Biessels GJ. Type 2 diabetes and cognitive dysfunction-towards effective management of both comorbidities. Lancet Diabetes Endocrinol. 2020;8(6):535–545. doi:10.1016/S2213-8587(20)30118-2
- Thomassen JQ, Tolstrup JS, Benn M, Frikke-Schmidt R. Type-2 diabetes and risk of dementia: observational and Mendelian randomisation studies in 1 million individuals. Epidemiol Psychiatr Sci. 2020;29:e118. doi:10.1017/S2045796020000347
- Reinke C, Buchmann N, Fink A, et al. Diabetes duration and the risk of dementia: a cohort study based on German health claims data. Age Ageing. 2022;51(1). doi:10.1093/ageing/afab231
- Biessels GJ, Despa F. Cognitive decline and dementia in diabetes mellitus: mechanisms and clinical implications. Nat Rev Endocrinol. 2018;14(10):591–604. doi:10.1038/s41574-018-0048-7
- Liu DS, Gao W, Lin -W-W, et al. Effects of the Chinese Yi-Qi-Bu-Shen Recipe extract on brainstem auditory evoked potential in rats with diabetes. J Ethnopharmacol. 2011;137(1):414–420. doi:10.1016/j.jep.2011.05.033
- Liu DS, Zhou YH, Liang ES, et al. Neuroprotective effects of the Chinese Yi-Qi-Bu-Shen recipe extract on injury of rat hippocampal neurons induced by hypoxia/reoxygenation. J Ethnopharmacol. 2013;145(1):168–174. doi:10.1016/j.jep.2012.10.046
- Goyal SN, Reddy NM, Patil KR, et al. Challenges and issues with streptozotocin-induced diabetes - A clinically relevant animal model to understand the diabetes pathogenesis and evaluate therapeutics. Chem Biol Interact. 2016;244:49–63. doi:10.1016/j.cbi.2015.11.032
- Tanbek K, Ozerol E, Yilmaz U, et al. Alpha lipoic acid decreases neuronal damage on brain tissue of STZ-induced diabetic rats. Physiol Behav. 2022;248:113727. doi:10.1016/j.physbeh.2022.113727
- Vorhees CV, Williams MT. Morris water maze: procedures for assessing spatial and related forms of learning and memory. Nat Protoc. 2006;1(2):848–858. doi:10.1038/nprot.2006.116
- Ghasemi R, Zarifkar A, Rastegar K, et al. Insulin protects against Abeta-induced spatial memory impairment, hippocampal apoptosis and MAPKs signaling disruption. Neuropharmacology. 2014;85:113–120. doi:10.1016/j.neuropharm.2014.01.036
- Tian H, Ding N, Guo M, et al. Analysis of learning and memory ability in an alzheimer’s disease mouse model using the Morris water maze. J Vis Exp. 2019;152. doi:10.3791/60055
- Ward R, Li W, Abdul Y, et al. NLRP3 inflammasome inhibition with MCC950 improves diabetes-mediated cognitive impairment and vasoneuronal remodeling after ischemia. Pharmacol Res. 2019;142:237–250. doi:10.1016/j.phrs.2019.01.035
- Zhang JH, Zhang J-F, Song J, et al. Effects of berberine on diabetes and cognitive impairment in an animal model: the mechanisms of action. Am J Chin Med. 2021;49(6):1399–1415. doi:10.1142/S0192415X21500658
- Chandrasekaran K, Choi J, Arvas MI, et al. Nicotinamide mononucleotide administration prevents experimental diabetes-induced cognitive impairment and loss of hippocampal neurons. Int J Mol Sci. 2020;21(11):3756. doi:10.3390/ijms21113756
- Ramos-Rodriguez JJ, Infante-Garcia C, Galindo-Gonzalez L, et al. Increased spontaneous central bleeding and cognition impairment in APP/PS1 mice with poorly controlled diabetes mellitus. Mol Neurobiol. 2016;53(4):2685–2697. doi:10.1007/s12035-015-9311-2
- Datusalia AK, Sharma SS. Amelioration of diabetes-induced cognitive deficits by GSK-3beta inhibition is attributed to modulation of neurotransmitters and neuroinflammation. Mol Neurobiol. 2014;50(2):390–405. doi:10.1007/s12035-014-8632-x
- Han X, Min M, Wang J, et al. Quantitative profiling of neurotransmitter abnormalities in brain, cerebrospinal fluid, and serum of experimental diabetic encephalopathy male rat. J Neurosci Res. 2018;96(1):138–150. doi:10.1002/jnr.24098
- Chu X, Zhou S, Sun R, et al. Chrysophanol relieves cognition deficits and neuronal loss through inhibition of inflammation in diabetic mice. Neurochem Res. 2018;43(4):972–983. doi:10.1007/s11064-018-2503-1
- Jing GC, Liu D, Liu Y-Q, et al. Nao-Fu-Cong ameliorates diabetic cognitive dysfunction by inhibition of JNK/CHOP/Bcl2-mediated apoptosis in vivo and in vitro. Chin J Nat Med. 2020;18(9):704–713. doi:10.1016/S1875-5364(20)60009-7
- Sun X, Li S, Xu L, et al. Paeoniflorin ameliorates cognitive dysfunction via regulating SOCS2/IRS-1 pathway in diabetic rats. Physiol Behav. 2017;174:162–169. doi:10.1016/j.physbeh.2017.03.020
- Bi T, Feng R, Zhan L, et al. ZiBuPiYin Recipe prevented and treated cognitive decline in ZDF rats with diabetes-associated cognitive decline via microbiota-gut-brain axis dialogue. Front Cell Dev Biol. 2021;9:651517. doi:10.3389/fcell.2021.651517
- Wang K, Chen Q, Wu N, et al. Berberine ameliorates spatial learning memory impairment and modulates cholinergic anti-inflammatory pathway in diabetic rats. Front Pharmacol. 2019;10:1003. doi:10.3389/fphar.2019.01003
- Wei Y, Luo Q-L, Sun J, et al. Bu-Shen-Yi-Qi formulae suppress chronic airway inflammation and regulate Th17/Treg imbalance in the murine ovalbumin asthma model. J Ethnopharmacol. 2015;164:368–377. doi:10.1016/j.jep.2015.01.016
- Zhang SG, Xiong GL, Yang X. 益气补肾颗粒治疗慢性肾功能不全的初步实验及临床研究 [Preliminary experimental and clinical study of the treatment of chronic renal insufficiency by granule of yi-qi bu-shen]. Zhongguo Zhong Xi Yi Jie He Za Zhi. 1992;12(6):335–7, 323. Chinese.
- Luo Y, Qin Z, Hong Z, et al. Astragaloside IV protects against ischemic brain injury in a murine model of transient focal ischemia. Neurosci Lett. 2004;363(3):218–223. doi:10.1016/j.neulet.2004.03.036
- Mao XQ, Wu Y, Wu K, et al. Astragalus polysaccharide reduces hepatic endoplasmic reticulum stress and restores glucose homeostasis in a diabetic KKAy mouse model. Acta Pharmacol Sin. 2007;28(12):1947–1956. doi:10.1111/j.1745-7254.2007.00674.x
- Wu Y, Ou-yang J-P, Wu K, et al. Hypoglycemic effect of Astragalus polysaccharide and its effect on PTP1B. Acta Pharmacol Sin. 2005;26(3):345–352. doi:10.1111/j.1745-7254.2005.00062.x
- Yu J, Zhang Y, Sun S, et al. Inhibitory effects of astragaloside IV on diabetic peripheral neuropathy in rats. Can J Physiol Pharmacol. 2006;84(6):579–587. doi:10.1139/y06-015
- Liu M, Wu K, Mao X, et al. Astragalus polysaccharide improves insulin sensitivity in KKAy mice: regulation of PKB/GLUT4 signaling in skeletal muscle. J Ethnopharmacol. 2010;127(1):32–37. doi:10.1016/j.jep.2009.09.055
- Zou F, Mao XQ, Wang N, Liu J, Ou-Yang JP. Astragalus polysaccharides alleviates glucose toxicity and restores glucose homeostasis in diabetic states via activation of AMPK. Acta Pharmacol Sin. 2009;30(12):1607–1615.
- Tang LQ, Wei W, Chen L-M, et al. Effects of berberine on diabetes induced by alloxan and a high-fat/high-cholesterol diet in rats. J Ethnopharmacol. 2006;108(1):109–115. doi:10.1016/j.jep.2006.04.019
- Bebrevska L, Foubert K, Hermans N, et al. In vivo antioxidative activity of a quantified Pueraria lobata root extract. J Ethnopharmacol. 2010;127(1):112–117. doi:10.1016/j.jep.2009.09.039
- Herrmann N, Lanctot KL, Khan LR. The role of norepinephrine in the behavioral and psychological symptoms of dementia. J Neuropsychiatry Clin Neurosci. 2004;16(3):261–276. doi:10.1176/jnp.16.3.261
- Raskind MA, Peskind ER. Neurobiologic bases of noncognitive behavioral problems in Alzheimer disease. Alzheimer Dis Assoc Disord. 1994;8(Suppl 3):54–60. doi:10.1097/00002093-199404000-00005
- Sontag TA, Hauser J, Kaunzinger I, Gerlach M, Tucha O, Lange KW. Effects of the noradrenergic neurotoxin DSP4 on spatial memory in the rat. J Neural Transm. 2008;115(2):299–303. doi:10.1007/s00702-007-0830-5
- Weinshenker D. Long road to ruin: noradrenergic dysfunction in neurodegenerative disease. Trends Neurosci. 2018;41(4):211–223. doi:10.1016/j.tins.2018.01.010
- Pillet LE, Taccola C, Cotoni J, et al. Correlation between cognition and plasma noradrenaline level in Alzheimer’s disease: a potential new blood marker of disease evolution. Transl Psychiatry. 2020;10(1):213. doi:10.1038/s41398-020-0841-7
- Braak H, Del Tredici K. Where, when, and in what form does sporadic Alzheimer’s disease begin? Curr Opin Neurol. 2012;25(6):708–714. doi:10.1097/WCO.0b013e32835a3432
- Matthews KL, Chen CPL-H, Esiri MM, et al. Noradrenergic changes, aggressive behavior, and cognition in patients with dementia. Biol Psychiatry. 2002;51(5):407–416. doi:10.1016/S0006-3223(01)01235-5
- Martignoni E, Blandini F, Petraglia F, et al. Cerebrospinal fluid norepinephrine, 3-methoxy-4-hydroxyphenylglycol and neuropeptide Y levels in Parkinson’s disease, multiple system atrophy and dementia of the Alzheimer type. J Neural Transm Park Dis Dement Sect. 1992;4(3):191–205. doi:10.1007/BF02260903
- Tohgi H, Ueno M, Abe T, et al. Concentrations of monoamines and their metabolites in the cerebrospinal fluid from patients with senile dementia of the Alzheimer type and vascular dementia of the Binswanger type. J Neural Transm Park Dis Dement Sect. 1992;4(1):69–77. doi:10.1007/BF02257623
- Elrod R, Peskind ER, DiGiacomo L, Brodkin KI, Veith RC, Raskind MA. Effects of Alzheimer’s disease severity on cerebrospinal fluid norepinephrine concentration. Am J Psychiatry. 1997;154(1):25–30.
- Gannon M, Che P, Chen Y, et al. Noradrenergic dysfunction in Alzheimer’s disease. Front Neurosci. 2015;9:220. doi:10.3389/fnins.2015.00220
- Knecht S, Breitenstein C, Bushuven S, et al. Levodopa: faster and better word learning in normal humans. Ann Neurol. 2004;56(1):20–26. doi:10.1002/ana.20125
- Shellshear L, MacDonald AD, Mahoney J, et al. Levodopa enhances explicit new-word learning in healthy adults: a preliminary study. Hum Psychopharmacol. 2015;30(5):341–349. doi:10.1002/hup.2480
- Breitenstein C, Flöel A, Korsukewitz C, Wailke S, Bushuven S, Knecht S. A shift of paradigm: from noradrenergic to dopaminergic modulation of learning? J Neurol Sci. 2006;248(1–2):42–47. doi:10.1016/j.jns.2006.05.012
- van der Velpen V, Teav T, Gallart-Ayala H, et al. Systemic and central nervous system metabolic alterations in Alzheimer’s disease. Alzheimers Res Ther. 2019;11(1):93. doi:10.1186/s13195-019-0551-7
- Comai S, Bertazzo A, Brughera M, Crotti S. Tryptophan in health and disease. Adv Clin Chem. 2020;95:165–218.