Abstract
Purpose
This study aimed to characterize adult patients admitted with diabetic ketoacidosis (DKA) in northern Jordan.
Methods
The study examined medical records of patients diagnosed with DKA from January 2015 to April 2018. Variables analyzed included diabetes type, precipitating illness, admission month, hospital length of stay, and biochemical markers.
Results
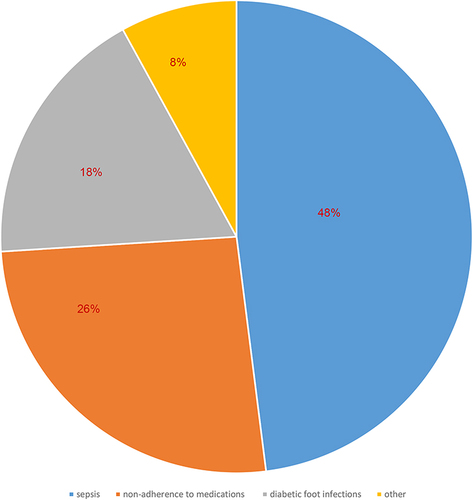
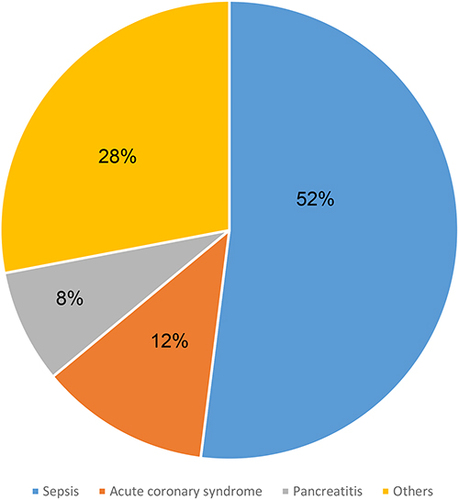
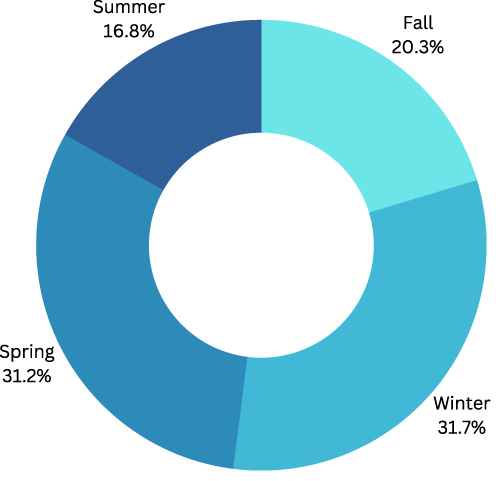
Out of 232 admissions with DKA, 70% were diagnosed with type 2 diabetes, and 56% were females. 12% of admissions had a new diagnosis of diabetes, of which 51% had type 2 diabetes. Sepsis (48%), Non-adherence (26%), and diabetic foot infections (18%) were the most encountered precipitating factors for DKA in T1DM. As for T2DM, sepsis (52%), acute coronary syndrome (12%), and pancreatitis (8%) were the most precipitating factors for DKA. High urea levels, high creatinine levels, low phosphorous levels, low hemoglobin levels, and high platelet counts were associated with a longer hospital stay for type 1 diabetes. For type 2 diabetes, low pH on admission, old age, and high Hb A1c within 6 months of admission were factors associated with a prolonged hospital stay. The study found a significant peak of admissions for DKA in both type 1 and type 2 patients in the winter and spring months (Pearson P-value= 0.0013).
Conclusion
The results of the present study highlight the seasonal variation in the frequency of DKA hospitalizations. It also highlights sepsis as the most frequent precipitating factor of DKA in both type 1 and type 2 DM patients.
Introduction
There are three main characteristics of diabetic ketoacidosis (DKA): ketonemia, acidemia, and hyperglycemia.Citation1 Diabetes ketoacidosis develops when insulin is completely or relatively deficient during the presence of excess counter-regulatory hormones.Citation2 Diabetic ketoacidosis (DKA) is a potentially life-threatening complication of type 1 diabetes and has been classically associated with it. However, type 2 diabetes patients have increasingly been diagnosed with this complication. Patients who experience diabetic ketoacidosis without a phenotype of Type 1 Diabetes are called Ketosis Prone Diabetics.Citation3–8 DKA has been reported primarily in Afro-Caribbean and indigenous populations of North America with type 2 diabetes.Citation3,Citation4 There have been studies analyzing DKA admissions in Chinese, Pakistani and Indian populations with type 2 diabetes as well.Citation5–7 Thus, DKA is not exclusively associated with certain ethnic minorities.Citation9
Our geographic location is transcontinental. There are many ethnicities in our area, mostly Arabs. Diabetes is highly prevalent in the Middle East. Prevalence of diabetes in Jordan was estimated to approach 32.4% back in 2017.Citation10
Currently, we lack studies in our region that describe patients who are ketosis-prone. We tried to describe these patients according to available data in our institution.
Patients who were admitted to critical care as a result of DKA were analyzed. We examined their data based on their demographics, precipitating illness, severity of presentation, and peak admission times.
Materials and Methods
Subjects
The study subjects included in the analysis were admitted to King Abdullah University Hospital with the diagnosis of DKA between January 2015 and April 2018. DKA diagnosis is given according to the American Diabetes Association guidelines,Citation2 DKA was defined by pH less than 7.3, high glucose levels, positive ketones (serum or urine), and bicarbonate levels less than 18 mEq per L. Subjects determined eligible to be included in the analysis were 14 years or above, admitted to ICU with the diagnosis of DKA. Patients were determined to be type 1 or type 2 diabetes according to the history in medical records, age at time of diagnosis of diabetes, mode of presentation and medications used to treat diabetes from the outset. Antibodies of type 1 diabetes and c-peptide level are not available in our institution laboratories to further differentiate types of diabetes and thus were not collected.
Methods
A retrospective review of medical records was conducted. Various data were collected about the patients such as age, gender, length of hospital stay, the month of admission, and cause of hospitalization. We collected laboratory results done on the day of admission, including serum glucose, glycated hemoglobin (HbA1c), venous pH, bicarbonate levels, kidney function tests, serum electrolytes, and complete blood counts. We defined the four seasons as winter in December–February, spring in March–May, summer in June–August, and autumn in September–November.
Statistical Analysis
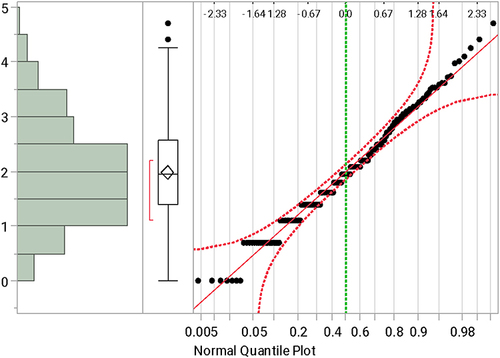
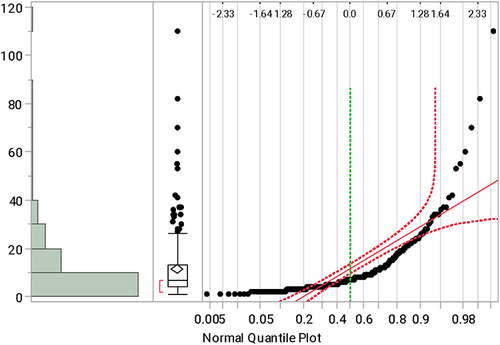
We used a Walter and Elwood 6 reversal of the Edwards test to determine the monthly variation in hospitalizations. In contrast, we used the Chi-squared test to determine whether DKA’s observed and expected seasonal incidences differed. The length of hospital stay was tested for normality to determine the factors that affected the length of hospital stay. We used log transformation to fix the normality issue when Q-Q plots were used, as shown in and . Linear regression was used afterward.
Figure 1 Testing the normality of the length of hospital stay. It was not normal when Q-Q plots were used.
Statistical analysis was conducted using JMP Pro 14 (SAS Institute Inc., Cary, NC, USA) and STATA 13.0 (StataCorp, College Station, TX, USA). All P-values are two-sided, and the significance level was set at P < 0.05.
Ethics Statement
The present study protocol was reviewed and approved by the Institutional Review Board (IRB) which is formed by active faculty members of the faculty of medicine in Jordan University of Science and Technology. This is a retrospective chart review and data collected would not adversely affect rights and welfare of subjects, so informed consent from participants was waived by IRB. Patient data confidentiality was observed in compliance with the Declaration of Helsinki.
Results
The hospital intensive care unit at our hospital has received a total of 232 DKA admissions during the period from January 2015 to April 2018.
Patients hospitalized with DKA had a mean age of 25.27± 5.52 for T1DM patients and 59.73± 13.43 for T2DM patients. There were 68 patients with type 1 diabetes and 164 with type 2 diabetes. Among all patients, 56% were females. In 12% of admissions, diabetes was diagnosed for the first time; 51% of those diagnosed had type 2 diabetes. .
Table 1 Patients Characteristics
The results of the laboratory tests conducted on the day of admission are presented in .
Table 2 Laboratory Results on Admission
Having an extended hospital stay in type 1 diabetes was associated with high urea, high creatinine, low phosphorus, low hemoglobin, and a high platelet count. We used linear regression to find the relationship between continuous variables and the log (#of days) for type 1 diabetes. P-value <0.005.
We studied the same factors for type 2, only the following variables were significant to affect the number of days of hospitalization; lower pH on admission and older age, as well as higher HbA1c within 3 months of admission. P-value<0.005.
Three factors were most often associated with DKA admissions to ICU in people with type 1 diabetes and regarded as the precipitating factors; sepsis (48%), non-adherence to medications (26%), and diabetic foot infections (18%). .
When it came to type 2 diabetes, sepsis (52%), acute coronary syndrome (12%), and pancreatitis (8%) were the most frequently encountered precipitating factors. .
We found a significant peak of admissions for DKA in both type 1 and type 2 patients in the months of winter and spring (Pearson P-value = 0.0013). .
Discussion
In northern Jordan, from 2015 to 2018, we studied patients who presented with DKA, the factors that contributed to the development of this complication and how it affected their hospitalization times. Our results describe infection as the main contributing factor to the development of DKA in both types of diabetes. These findings are consistent with the literature, which suggest infections as frequent causes for the development of DKA in diabetic patients.Citation11,Citation12
There is a seasonal pattern to infectious diseases, such as influenza viruses; however, hospitalizations for asthma, heart failure, and myocardial infarctions also exhibit seasonal fluctuations.Citation13–17 An analysis of 207 diabetic ketoacidosis cases from Korea revealed a seasonality that peaks in December for most cases.Citation18 Temporal variations were demonstrated for acute complications with T1D by many studies with winter being a high risk for DKA. Authors explained the potential causes underlining the temporality of hospitalizations as environmental (eg, temperature, daylight hours, and/or air pollution), social and/or behavioral (eg holiday periods, changes in dietary habits, and physical activity), physiological, or a combination of such factors.Citation18–23 Similar studies have found that HbA1c levels of school children with type 1 diabetes vary seasonally,Citation24 which is associated with changes in the weather. HbA1c levels were inversely related to temperature (r = –0.56, P = 0.0002) and sunshine hours (r = –0.52, P = 0.0007).
In another study comparing HbA1c between the Northern and Southern hemispheres, temperature was found again to be related to variation in HbA1c, with levels being higher in cooler months and lower in warmer months.Citation25
Researchers have also found that glycemic control in adults with type 2 diabetes varies with the season (with significantly higher HbA1c values noted in winter).Citation26–28 There may be a differential risk for DKA depending on the temporal variation of HbA1c. There is no doubt that the level of HbA1c is a reliable predictor of acute complications, with higher HbA1c values being associated with DKA.Citation29–32 Our study found that high HbA1c was associated with a prolonged hospital stay in type 2 diabetes patients presenting with DKA. That may reflect as well the increased risk of complications inherent with poor control of diabetes.
The study also identified other factors that predicted prolonged hospital stay for both types of diabetes.
These factors may be point to the severity of acute illness triggering the onset of DKA.Citation33 It may also indicate how poorly controlled diabetes over the preceding months of acute presentation affects the general health of diabetic patients which leads to a more protracted stay in hospital.Citation34
The results of this study contribute to the existing body of knowledge regarding DKA in the Middle East. The study provides insight into characteristics of DKA in the population of northern Jordan, a region with a relatively high prevalence of diabetes. Furthermore, the findings of this study can inform clinical practice on the need for monitoring for infections and adherence to medications in patients with diabetes, particularly during the winter and spring seasons.
The limitations of this study include its retrospective design, which limited the amount of data that could be collected and analyzed. Additionally, the study was conducted at a single center, which may limit the generalizability of the results to other regions in Jordan and the Middle East region.
Conclusion
In conclusion, this retrospective study aimed to identify the characteristics of adult patients admitted with DKA in northern Jordan, examining variables such as type of diabetes, precipitating illness, month of admission, length of stay, and biochemical markers. The results of this study revealed a significant peak of admissions for DKA in both type 1 and type 2 patients in the months of winter and spring, which suggests a seasonal variation in the frequency of DKA hospitalizations. The most frequent precipitating factor of DKA for both type 1 and type 2 patients was sepsis. For type 2 diabetes patients, it was also found that ketosis-prone diabetes was highly prevalent. This finding highlights the need for further studies to determine the prevalence of ketosis-prone diabetes in the population of Jordan.
Disclosure
The authors declare no competing interests.
Additional information
Funding
References
- Kitabchi AE, Drexler A. Diabetic ketoacidosis and hyperglycemic hyperosmolar state. In: De Fronzo RA, editor. International Textbook of Diabetes Mellitus. 3rd ed. John Wiley and Sons; 2004:1101.
- American Diabetes Association. Hyperglycaemic crises in patients with diabetes mellitus. Diabetes Care. 2002;25(Suppl 1):s100–s108. doi:10.2337/diacare.25.2007.S100
- Umpierrez G, Casals MMC, Gebhart SSP, et al. Diabetic ketoacidosis in obese African-Americans. Diabetes. 1995;44:790–795. doi:10.2337/diab.44.7.790
- Wilson C, Krakoff J, Gohdes D, et al. Ketoacidosis in Apache Indians with non-insulin-dependent diabetes mellitus. Arch Intern Med. 1997;157:2098–2100. doi:10.1001/archinte.1997.00440390094012
- Chu CH. The occurrence of diabetic ketoacidosis in type 2 diabetic adults. Am J Med. 1996;101(1):19–24. doi:10.1016/S0002-9343(96)00076-9
- Jabbar A, Farooqui K, Habib A, et al. Clinical characteristics and outcomes of diabetic ketoacidosis in Pakistani adults with type 2 diabetes mellitus. Diabet Med. 2004;21:920–923. doi:10.1111/j.1464-5491.2004.01249.x
- Rao VD, Pradhan B, Mallikarjuna Y, et al. Clinical profile of diabetic ketoacidosis in adults. Health Renaissance. 2012;10(2):80–86. doi:10.3126/hren.v10i2.6569
- Wang ZH, Kihl-Selstam E, Eriksson JW. Ketoacidosis occurs in both Type 1 and Type 2 diabetes, a population-based study from Northern Sweden. Diabet Med. 2008;25(7):867–870. doi:10.1111/j.1464-5491.2008.02461.x
- Balasubramanyam A, Nalini R, Hampe CS, Maldonado M. Syndromes of ketosis-prone diabetes mellitus. Endocr Rev. 2008;29(3):292–302. doi:10.1210/er.2007-0026
- Ajlouni K, Batieha A, Jaddou H, et al. Time trends in diabetes mellitus in Jordan between 1994 and 2017. Diabet Med. 2019;36:1176–1182. doi:10.1111/dme.13894
- Nyenwe EA, Kitabchi AE. The evolution of diabetic ketoacidosis: an update of its etiology, pathogenesis and management. Metabolism. 2016;65(4):507–521. doi:10.1016/j.metabol.2015.12.007
- Kitabchi AE, Nyenwe EA. Hyperglycemic crises in diabetes mellitus: diabetic ketoacidosis and hyperglycemic hyperosmolar state. Endocrinol Metab Clin. 2006;35(4):725–751. doi:10.1016/j.ecl.2006.09.006
- Spencer F, Goldberg R, Becker RG, Gore JM. Seasonal distribution of acute myocardial infarction in the second National Registry of Myocardial Infarction. J Am Coll Cardiol. 1998;31:1226–1233. doi:10.1016/S0735-1097(98)00098-9
- Public Health Agency of Canada. Flu (influenza); 2011. Available from: http://www.phac-aspc.gc.ca/influenza/index-eng.php. Accessed November 20, 2023.
- Langley G, Anderson L. Epidemiology and prevention of respiratory syncytial virus infections among infants and young children. Pediatr Infect Dis J. 2011;30:510–517. doi:10.1097/INF.0b013e3182184ae7
- Crighton E, Mamdani M, Upshur R. A population based time series analysis of asthma hospitalizations in Ontario, Canada: 1988 to 2000. BMC Health Serv Res. 2001;1:7. doi:10.1186/1472-6963-1-7
- Gallerani M, Boari B, Manfredini F, Manfredini R. Seasonal variation in heart failure hospitalization. Clin Cardiol. 2011;34:389–394. doi:10.1002/clc.20895
- Lee HK, Oh YS, Chung YH, et al. Epidemiological characteristics of ketoacidosis among Korean diabetic patients. J Korean Med Sci. 1987;2:7–11. doi:10.3346/jkms.1987.2.1.7
- Goday A, Castell C, Tresserras R, Canela J, Taberner JL, Lloveras G. Incidence of Type 1 (insulin-dependent) diabetes mellitus in Catalonia. Spain Diabetologia. 1992;35:267–271. doi:10.1007/BF00400928
- Padaiga Z, Tuomilehto J, Karvonen M, et al. Seasonal variation in the incidence of Type 1 diabetes mellitus during 1983 to 1992 in the countries around the Baltic Sea. Diabet Med. 1999;16:736–743. doi:10.1046/j.1464-5491.1999.00140.x
- Samuelsson U, Carstensen J, Löfman O, Nordfeldt S. Seasonal variation in the diagnosis of T1D in southeast Sweden. Diabetes Res Clin Pract. 2007;76:75–81. doi:10.1016/j.diabres.2006.07.023
- Karvonen M, Jäntti V, Muntoni S, et al. Comparison of the seasonal pattern in the clinical onset of IDDM in Finland and Sardinia. Diabetes Care. 1998;21:1101–1109. doi:10.2337/diacare.21.7.1101
- Ludvigsson J, Afoke AO. Seasonality of Type 1 (insulin-dependent) diabetes mellitus: values of C-peptide, insulin antibodies and haemoglobin A (1c) show evidence of a more rapid loss of insulin secretion in epidemic patients. Diabetologia. 1989;32:84–91. doi:10.1007/BF00505179
- Mianowska B, Fendler W, Szadkowska A, et al. HbA1c levels in schoolchildren with T1D are seasonally variable and dependent on weather conditions. Diabetologia. 2011;54:749–756. doi:10.1007/s00125-010-2013-4
- Higgins T, Saw S, Sikaris K, et al. Seasonal variation in hemoglobin A1c: is it the same in both hemispheres? J Diabetes Sci Technol. 2009;3:668–671. doi:10.1177/193229680900300408
- Tseng C-L, Brimacombe M, Xie M, et al. Seasonal patterns in monthly hemoglobin A1c values. Am J Epidemiol. 2005;161:565–574. doi:10.1093/aje/kwi071
- Ishii HSH, Baba T, Nakamura K, Watanabe T. Seasonal variation of glycemic control in type 2 diabetic patients. Diabetes Care. 2001;2001:241503.
- Gikas A, Sotiropoulos A, Pastromas V, Papazafiropoulou A, Apostolou O, Pappas S. Seasonal variation in fasting glucose and HbA1c in patients with type 2 diabetes. Prim Care Diabetes. 2009;3:111–114. doi:10.1016/j.pcd.2009.05.004
- Govan L, Wu O, Briggs A, et al. Achieved levels of HbA1c and likelihood of hospital admission in people with type 1 diabetes in the Scottish population. Diabetes Care. 2011;34:1992–1997. doi:10.2337/dc10-2099
- Rewers A, Chase HP, Mackenzie T, et al. Predictors of acute complications in children with type 1 diabetes. JAMA. 2002;287:2511–2518. doi:10.1001/jama.287.19.2511
- Fritsch M, Rosenbauer J, Schober E, et al. Predictors of diabetic ketoacidosis in children and adolescents with T1D. Experience from a large multicentre database. Pediatr Diabetes. 2011;12:307–312. doi:10.1111/j.1399-5448.2010.00728.x
- Butalia S, Johnson JA, Ghali WA, Rabi DM. Clinical and socio-demographic factors associated with diabetic ketoacidosis hospitalization in adults with Type 1 diabetes. Diabet Med. 2013;30:567–573. doi:10.1111/dme.12127
- Freire AX, Umpierrez GE, Afessa B, et al. Predictors of intensive care unit and hospital length of stay in diabetic ketoacidosis. J Crit Care. 2002;17(4):207–211. doi:10.1053/jcrc.2002.36755
- Ata F, Khan AA, Khamees I, et al. Clinical and biochemical determinants of length of stay, readmission and recurrence in patients admitted with diabetic ketoacidosis. Ann Med. 2023;55(1):533–542. doi:10.1080/07853890.2023.2175031