Abstract
Purpose
Diabetes distress (DD) refers to the negative emotions and burden of living with diabetes. Illness perceptions are among the factors that can influence self-management and psychological distress in diabetics. This study aimed to determine the prevalence and the associated factors of DD in Tunisian patients with type 2 diabetes mellitus. We also studied the relationship between DD and illness perceptions in diabetics.
Patients and Methods
This was a cross-sectional study conducted among individuals with type 2 diabetes, followed up at the outpatient endocrinology unit at the Hedi Chaker University Hospital, Tunisia. DD was assessed using the Diabetes Distress Scale (DDS-17). The Brief Illness Perception Questionnaire (Brief-IPQ) was used to assess diabetes illness perceptions. Multivariate logistic regression was used to determine independent factors associated with the presence of DD.
Results
A total of 103 patients were recruited. The mean age was 59.31 (±10.83) years; 54.4% were female. In total, 70.9% had DD. Using regression analysis, we demonstrated that the illness perceptions of personal control, HbA1C, absence of comorbidities, lower age at diabetes diagnosis, and socioeconomic status were significantly associated with DD.
Conclusion
This study sheds light on the high prevalence of DD among patients with type 2 diabetes in Tunisia. Illness perception-focused psychological intervention would be efficacious in reducing diabetes distress in patients with type 2 diabetes mellitus.
Introduction
Diabetes mellitus (DM) is one of the most serious chronic illnesses in the world. The International Diabetes Federation (IDF) reported in 2021 that 537 million adults were living with diabetes.Citation1 DM prevalence is rising rapidly in low and middle-income countries. Its prevalence in Tunisia, a part of the IDF-MENA Region, reached 18.2% in 2019.Citation2 Diabetes not only has an impact on an individual’s physical health but also affects his/her mental well-being. A diagnosis of diabetes implies changes in life habits and imposes additional responsibilities such as following a dietary regimen, engaging in regular physical activity, and self-monitoring blood glucose levels.Citation3 Living with diabetes can be stressful and may lead to a specific condition known as diabetes distress. Diabetes distress (DD) is a concept proposed for the first time in the literature by a group of psychologists and psychiatrists from the Joslin Diabetes Centre in 1995.Citation4 Diabetes distress refers to the negative emotional or affective experience resulting from the challenge of the daily management of diabetes.Citation5
Diabetes distress is considered one of the most important psychosocial factors in the management of diabetes. It was suggested that DD could be linked to cultural and social norms, emphasizing the role of representations about diabetes in the increase of distress among patients with diabetes.Citation6 According to Leventhal’s Common-Sense Model (CSM), ill people construct personal representations of their disease, namely illness perceptions, which determine their coping strategies and the emotional response to their disease.Citation7
Illness perception has been identified in the literature as a significant factor that impacts self-management behaviors, psychological distress, and other health outcomes among patients with T2D.Citation6,Citation8–11
DD is a very common and highly prevalent psychological problem in diabetic patients, and it can have a significant impact on T2D management.Citation12 However, to the best of our knowledge, few studies have highlighted the significance of the psychological aspects of diabetes in Tunisia.
The current study aimed to determine the prevalence of DD and its associated factors and to explore the relationship between DD and illness perceptions among Tunisian patients with T2D.
Materials and Methods
Sample and Procedure
A cross-sectional, descriptive, and analytical study was conducted between March 2021 and October 2021 in an outpatient clinic at the endocrinology department at the Hedi Chaker University Hospital in Sfax (Tunisia). It is a public tertiary care academic medical center.
Participants were selected using convenience sampling of adults aged 20 years or more diagnosed with type 2 diabetes at least 1 year previously, according to the diagnostic criteria of the American Diabetes Association (ADA) (2016 edition). Exclusion criteria were type 1 diabetes and a history of mental illness or communication disorders.
The same-trained interviewer, who explained the study to interviewed patients awaiting their appointments with their doctor, explained the study to them. All patients gave informed consent and participated voluntarily.
Data Collection and Measures
Data were collected through individual interviews with the patients and from medical records. Social and demographic data (age, sex, education level, marital status, employment situation, and economic income) and clinical data (age at diagnosis of DM, duration of DM, diabetes in first-degree relatives, use of diet and exercise to manage disease, presence of diabetic complications, and comorbid illness, treatment, and glycated hemoglobin (HbA1c) level) were documented. Then, the Arabic version of the Diabetes Distress Scale (DDS-17) and the Brief Illness Perception Questionnaire (Brief-IPQ) were applied.
The Diabetes Distress Scale
Diabetes distress was measured using the 17-item Diabetes Distress Scale (DDS-17).Citation13 The DDS-17 evaluates DD over the previous month. It consists of 17 items rated on a Likert scale ranging from 1 (no problem) to 6 (serious problem). Items were grouped into four subscales: emotional burden (5 items), physician-related distress (4 items), regimen-related distress (5 items), and diabetes-related interpersonal distress (3 items). The total mean distress score was calculated by summing up the total of the 17 items and dividing by 17.Citation13,Citation14 A mean item score of greater than or equal to 3 is considered a level of distress that deserves clinical attention.Citation15 We used an Arabic-validated version of DDS-17, with Cronbach’s alpha coefficient ranging from 0.778 to 0.881 for the subscales and 0.822 for the total scale.Citation16
The Brief Illness Perception Questionnaire (Brief-IPQ)
The “Brief Illness Perception Questionnaire” (Brief-IPQ), developed in 2006 by Broadbent et al,Citation17 is a short version of the “Illness Perception Questionnaire-Revised” questionnaire, based on Leventhal’s research on representations of the disease and allows the measurement of the perception of the disease. It consists of 9 items. Eight items are rated on an 11-point scale (0–10) to assess the patients’ representations (ranging from 0 = not at all to 10 = extremely). Each of the items assesses one of the dimensions of the perception of the disease: “consequences” (Item 1), “timeline” (Item 2), “the degree of personal control over the disease” (Item 3), “treatment control” (Item 4), “identity” (Item 5) “concern” (Item 6), “emotional response” (Item 7), and “Coherence” (Item 8). The ninth item (Item 9) was an open-ended question, requiring the patients to list the 3 most important causal factors underlying their illness. The Arabic version of the Brief-IPQ was used in this study.Citation18 The reported Cronbach’s alpha was 0.717.Citation18
Statistical Analysis
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) 20.0 (IBM SPSS Statistics, New York, United States). Quantitative variables were presented as mean ± standard deviation (SD) or median and range. Qualitative variables were represented as numbers and percentages. We used kolmogorov Smirnov test to determine if variables were normally distributed. Student’s t-test, Chi-square test, and Mann–Whitney U-test were used to compare the variables between participants without DD and those with DD. After the univariate analysis, a logistic regression model was performed to identify the factors independently associated with DD. Data were considered statistically significant when P < 0.05.
Results
A total of 103 T2DM patients were recruited. The sociodemographic and clinical profile of the sample is presented in .
Table 1 Demographic and Clinical Characteristics of Tunisian Adult with DM 2 (N = 103)
The mean age was 59.31 (±10.83) years; 54.4% were female, 58.2% had only a primary school education or no formal education, 40.8% were employed, and 62.1% had medium economic income. Among the recruited patients, 42.7% reported that they practiced physical exercise, and 49.5% followed a healthy diet to manage the disease. The majority (95.1%) had a relative with DM. The mean age at diagnosis was 49.62 ± 9.4 years, and the median duration of diabetes was 7 years (range 1–34 years). A large majority of the sample (80.6%) had comorbidities, including hypertension and dyslipidemia, 40.8% had diabetic complications, and 46.6% were on insulin. Just over two-thirds (68.9%) of patients had uncontrolled diabetes (HbA1c >7%).
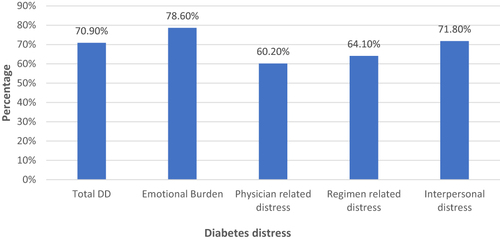
Among the study participants, 70.9% had DD. Emotional burden was the most prevalent domain (78.6% of the participants). The distribution of participants across the four subdomains is shown in .
Descriptive analysis of the 8 items included in the Brief-IPQ questionnaire showed that (), in general, patients with T2M tended to perceive their diabetes as a chronic disease (timeline) that can be well-controlled with appropriate treatment (treatment control). The respondents reported a moderate perception of coherence, which reflects a moderate personal understanding of diabetes (coherence). In addition, they reported a low perception of their own ability to control their diabetes (personal control). They were convinced that they had experienced many diabetes-related symptoms (identity). They mostly perceived diabetes as a disease that has serious consequences (consequences), so they were concerned about it (concern) and were emotionally affected (emotional response).
Table 2 Descriptive Statistics for the 8 Items of the Brief Illness Perception Questionnaire (the Brief IPQ) Completed by Patients with Diabetes Mellitus Type 2
shows the demographic and clinical variables associated with DD. Diabetes-related distress was more common in married patients (p=0.034), with lower socio-economic status (p=0.001), with age at onset of diabetes <50 years (p=0.001), without comorbidities (p=0.008), and with insulin therapy (p=0.030). High HbA1c (p<0.001) has been correlated with DD.
Table 3 Demographic and Clinical Factors Associated with Diabetes Distress
Patients with DD presented a greater perception of consequences (p<0.001), a low perception of personal control (p=0.001), and a low belief in the efficacy of the treatment (p< 0.001); they were also more concerned (p=< 0.001) and more emotionally affected by their diabetes (p< 0.001) ().
Table 4 Results of the Nonparametric Test (Mann–Whitney U-Test) for the Association of Illness Perceptions Domains and Diabetes Distress
Multivariable logistic regression () revealed that lower age at diabetes diagnosis ([OR] =0.93; [CI] = [0.87–0.99]; p=0.027), lower socioeconomic status ([OR] =0.07; [CI] = [0.01–0.38]; p=0.002), absence of comorbid illness ([OR] = 0.063; [CI] = [0.005–0.87]; p=0.039), HbA1C ≥7 ([OR] = 4.87; [CI] = [1.50–15.77]; p=0.008), and worse personal control (odds ratio [OR] = 0.62; confidence interval [CI] = [0.45–0.86]; p=0.004) were significant contributors to high levels of DD.
Table 5 Multivariate Logistic Regression Analysis of Factors Associated with DD
Discussion
The current study revealed that a considerable proportion of a sample of Tunisian patients with T2D was suffering from clinically significant DD. The prevalence of diabetes-related distress in the sample was 70.9%. The prevalence of DD in T2D varies greatly between the studies depending on demographics, geographical region, and cultural backgrounds.Citation19 The prevalence of DD was 40.3% in Qatar,Citation8 44% in South Africa,Citation20 42% in India,Citation21 and 64% in China.Citation22 These estimates are significantly higher than those reported in a meta-analysis of 55 studies. This meta-analysis shows that DD prevalence was 36%.Citation12
The high prevalence of DD in the current study may be due to several reasons. First, because we recruited our patients from a tertiary public hospital, participants had a lower level of education and income and may present with more complex and severe cases and, therefore, may have higher levels of distress. Moreover, the public healthcare system of low- and middle-income countries is already overstretched and has limited resources but must meet the demands of the majority of the population. Patients are often seen by different healthcare professionals who are overworked and do not have enough time to provide consistent, high-quality, and individualized holistic care for their patients.Citation20
Furthermore, the higher prevalence in our sample could be due to the existing comorbidity of undiagnosed depression and the stress related to the COVID-19 Pandemic at the time of the study.
Emotional burden (78.6%) was considered the most important domain in measuring diabetes distress. Similar results were found in the study by Hu et al.Citation23 The higher prevalence of emotional distress could be attributed to the difficulty of self-management, self-care, and the psychological aspect of managing a chronic disease.Citation24
In the present study, we found that low economic income, being married, lower age at diabetes diagnosis, absence of comorbidities, use of insulin, and uncontrolled diabetes were the factors associated with DD in patients with T2D. Gender, education level, duration of diabetes, and complications had no significant correlation with DD, which differs from findings in previous reports.Citation21,Citation25
In this study, married patients reported significantly higher DD. The presence of a partner may be a source of stress, as the patients may be subjected to more supervision and pressure from the partner regarding his/her diabetes self-management behaviors.Citation26,Citation27
We found that low economic income was significantly associated with DD. Previous reports indicate that family income is an important factor contributing to DD.Citation28 These patients would have more difficulty obtaining treatment and monitoring their blood sugar levels and, therefore, more stress factors in the management of the disease.Citation21,Citation29
In our study, the age of onset younger than 50 years and the absence of comorbidities were significantly associated with DD (p=0.001, p=0.008, respectively). These results were similar to the findings from other studiesCitation30–32 that demonstrated a significant correlation between DD and age. Younger patients were less likely to have comorbidities; they were not used to being sick or experienced in the management of chronic diseases.Citation32 In addition, living with diabetes requires the patient to follow many dietary regimens that are not easily tolerated by young adults.Citation32 An unexpected diagnosis of diabetes at an early age and the absence of coping mechanisms to cope with a severe chronic disease lead to high DD levels.Citation20,Citation33 Additionally, higher DD among younger patients could be explained by the stressors of financial, work, and family responsibilities.Citation20
Contrary to other studies,Citation30,Citation32 we did not find correlations between DD and the presence of diabetic complications. This may be because those with complications can be offered specialized healthcare support, which may diminish the distress experienced due to diabetes.Citation29 Other studies found that patients with diabetic complications had more DD due to the high burden of diabetes-related complications with possible frequent hospital visits and admissions.Citation32
The use of insulin therapy was correlated with DD. Patients who use insulin require frequent blood glucose self-monitoring and dietary behavior modifications. The management of these factors requires considerable effort by the patient.Citation27 Previous studies suggested that Insulin distress is a major contributor to DD. Insulin distress is defined as an emotional response to a suggestion to use insulin, characterized by extreme apprehension, discomfort, dejection, or denial due to a perceived inability to cope with the requirements of insulin therapy.Citation34,Citation35
Uncontrolled diabetes (HbA1c>7) was strongly correlated with DD (p<0.001), which is in keeping with most studies in the literature that support this view.Citation20,Citation36 Fisher et alCitation36 conducted a cross-sectional and longitudinal analysis and showed that distress presented time-concordant relationships with HbA1c. They suggest a bidirectional relationship between distress and HbA1c.Citation36 DD has direct mechanism hormones as well as indirect effects on glycemic control. DD can directly increase the cortisol hormone, which suppresses insulin production leading to an increase in HbA1c.Citation37 Indirectly, high disease distress can affect self-efficacy, diabetes self-management behaviors, and medication compliance and consequently worsen glycemic control.Citation36,Citation37 Lack of glycemic control can generate distress, which can affect disease management.Citation36
The Brief-IPQ revealed that these T2DM patients perceived their condition as chronic with an important impact on life. Therefore, they were more concerned and emotionally affected by their disease than reported in previous studies.Citation10,Citation17
Compared to previous studies,Citation10 our patients demonstrated low levels of personal control, indicating a lack of confidence in their ability to control their diabetes. However, they perceived their treatments as effective. Thus, our patients had confidence in the treatments and advice given by their doctors.
Most categories of illness perceptions (Consequences, Personal control, Treatment control, Concern, and Emotional representations) were correlated with DD. In our study, patients with DD presented a greater perception of consequences (p < 0.001), low perception of personal control (p = 0.001), low belief in treatment efficacy (p < 0.001), high perception of “concern” (p< 0.001) and a greater impact of negative emotions generated by their diabetes (p < 0.001). Our results were consistent with previous research.Citation38,Citation39 Meta-analysis studies found that low-threat perceptions and high-control perceptions were positively associated with psychological well-being and functioning and negatively associated with distress.Citation11,Citation38,Citation39
Personal control refers to a patient’s belief in their ability to control their diabetes and has been shown to predict illness outcomes and subsequent coping strategies.Citation40 In our study, lower personal control was significantly associated with higher DD. Our results were similar to those of Skinner et al, who show that people who believe their willpower is limited report having lower perceived control over their diabetes and experiencing more DD.Citation41 They suggest a model of causal mediation and direct effects of willpower beliefs on illness beliefs (perceived control) and diabetes distress.Citation41
The CSM model showed that illness perception control had a positive indirect association with self-care behaviors through more problem-focused coping (eg, using action planning to tackle the encountered problems).Citation11 Patients with high personal control and self-efficacy view themselves as having a greater influence on their illness and are, therefore, more likely to be proactive in performing self-management behaviors and experience lower levels of distress.Citation11
In our study, patients with DD presented a greater perception of consequences and a greater impact of negative emotions generated by their diabetes. Thus, these patients had threat perceptions and viewed diabetes as an illness with serious adverse impacts on daily life. It is suggested that perceived threat may evoke avoidant-oriented coping responses (eg, denial of the diagnosis, minimization of the threat, and resorting to substance use), which dampen adaptive self-regulation, may lead to failure to engage in diabetes self-care behaviors, and may lead to distress.Citation11,Citation38,Citation42 Conversely, other research demonstrates that perceived threats potentially enhance the adoption of problem-focused coping and consequent engagement in self-care activities.Citation11,Citation43 However, it was proved that perceptions of personal control are more effective than the perception of threat to adopt adaptive problem-focused coping strategies.Citation11,Citation43 These results indicate that illness perceptions have different impacts on diabetic patients’ health. Socio-cultural characteristics and personality traitsCitation43 may influence the illness representation and coping strategies that are employed by patients with T2D.
Limitations
To the best of our knowledge, our study is the first to study DD and its relationship with illness perception in patients with T2D in Tunisia. However, the limitations of this study should be taken into account when interpreting the results. The first was the limited sample size. Second, our sample may not be representative of the whole population of diabetics, as the study was based on a sample of T2D patients treated in a public university hospital. Such patients may generally be more severely affected by the disease. Third, the transversal nature of the study will not permit us to follow the longitudinal changes. Cohort studies should be conducted to better explore DD.
Conclusion
Our study shows that diabetes distress is highly prevalent in our patients with T2D. Factors that significantly contributed to high levels of distress were low economic income, lower age at diabetes diagnosis, absence of comorbidities, uncontrolled diabetes, and worse personal control. The study results endorsed the need for clinical attention to DD.
The findings of the present study suggest that the illness perceptions, especially personal control, of Tunisian patients with T2D should be improved. Indeed, our study underlines the impact of illness perceptions on DD. Illness perception-focused psychological intervention would be efficacious in reducing diabetes distress in patients with type 2 diabetes mellitus.
Institutional Review Board Statement
All procedures performed in this study were in accordance with the ethical standards of the Hedi Chaker University Hospital committee and with the 1964 Helsinki declaration and its later amendments. The Hedi Chaker University Hospital Committee approved this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
We would like to thank the patients for participating in the study. We also wish to thank Professor Chokri Khalaf for proofreading the manuscript. The poster’s abstract was published in ‘Poster Abstracts’ in European Psychiatry. 2023;66(Suppl 1):S773–4.: [doi: 10.1192/j.eurpsy.2023.1631].
References
- Sun H, Saeedi P, Karuranga S., et al. IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. doi:10.1016/j.diabres.2021.109119
- Elleuch M, Mnif F, Malouf JK, Benlassoued M, Kamel MS, Abid M. Inventory of insulin access in Tunisia, IDF-MENA Region. J Diabetol. 2022;13(Suppl 1):S68–S72. doi:10.4103/jod.jod_113_22
- Berry E, Lockhart S, Davies M, Lindsay JR, Dempster M. Diabetes distress: understanding the hidden struggles of living with diabetes and exploring intervention strategies. Postgrad Med J. 2015;91(1075):278–283. doi:10.1136/postgradmedj-2014-133017
- Polonsky WH, Anderson BJ, Lohrer PA, et al. Assessment of diabetes-related distress. Diabetes Care. 1995;18(6):754–760. doi:10.2337/diacare.18.6.754
- Skinner TC, Joensen L, Parkin T. Twenty‐five years of diabetes distress research. Diabet Med. 2020;37(3):393–400. doi:10.1111/dme.14157
- Chittem M, Chawak S, Sridharan SG, Sahay R. The relationship between diabetes-related emotional distress and illness perceptions among Indian patients with Type II diabetes. Diabet Metabol Synd. 2019;13(2):965–967. doi:10.1016/j.dsx.2018.12.018
- Leventhal H, Meyer D, Nerenz D. The common sense representation of illness danger. Contrib Med Psychol. 1980;2:7–30.
- Abdalla H, Alnuaimi A, Gadallah A, et al. Prevalence of diabetes distress among people with type 2 diabetes at primary health care in Qatar: a cross-sectional study. Middle East J Fam Med. 2020;7:10.
- Kugbey N, Oppong Asante K, Adulai K. Illness perception, diabetes knowledge and self-care practices among type-2 diabetes patients: a cross-sectional study. BMC Res Notes. 2017;10(1):1–7. doi:10.1186/s13104-017-2707-5
- Petriček G, Vrcić-Keglević M, Vuletić G, Cerovečki V, Ožvačić Z, Murgić L. Illness perception and cardiovascular risk factors in patients with type 2 diabetes: cross-sectional questionnaire study. Croat Med J. 2009;50(6):583–593. doi:10.3325/cmj.2009.50.583
- Xin M, Chan VW, Kong AP, et al. Using the common-sense model to explicate the role of illness representation in self-care behaviours and anxiety symptoms among patients with Type 2 diabetes. Patient Educ Couns. 2023;107:107581. doi:10.1016/j.pec.2022.107581
- Perrin N, Davies M, Robertson N, Snoek F, Khunti K. The prevalence of diabetes‐specific emotional distress in people with Type 2 diabetes: a systematic review and meta‐analysis. Diabet Med. 2017;34(11):1508–1520. doi:10.1111/dme.13448
- Polonsky WH, Fisher L, Earles J, et al. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care. 2005;28(3):626–631. doi:10.2337/diacare.28.3.626
- Kamrul-Hasan A, Hannan MA, Asaduzzaman M, et al. Prevalence and predictors of diabetes distress among adults with type 2 diabetes mellitus: a facility-based cross-sectional study of Bangladesh. BMC Endocr Disord. 2022;22(1):28. doi:10.1186/s12902-022-00938-3
- Fisher L, Hessler DM, Polonsky WH, Mullan J. When is diabetes distress clinically meaningful? Establishing cut points for the diabetes distress scale. Diabetes Care. 2012;35(2):259–264. doi:10.2337/dc11-1572
- Darawad MW, Hammad S, Samarkandi OA, Hamdan-Mansour AM, Khalil AA. Evaluating the psychometric properties of the Arabic version of the diabetes distress scale. J Psychosoc Nurs Ment Health Serv. 2017;55(9):43–51. doi:10.3928/02793695-20170818-12
- Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60(6):631–637. doi:10.1016/j.jpsychores.2005.10.020
- Saarti S, Jabbour H, El Osta N, Hajj A, Khabbaz LR. Cross-cultural adaptation and psychometric properties of an Arabic language version of the brief illness perception questionnaire in Lebanon. Libyan J Med. 2016;11(1):31976. doi:10.3402/ljm.v11.31976
- Pouwer F, Wijnhoven H, Ujcic‐Voortman J, et al. Ethnic aspects of emotional distress in patients with diabetes–the Amsterdam Health Monitor Study. Diabet Med. 2013;30(1):e25–e31. doi:10.1111/dme.12031
- Ramkisson S, Pillay BJ, Sartorius B. Diabetes distress and related factors in South African adults with type 2 diabetes. J Endocrinol Metabol Diabet South Africa. 2016;21(2):35–39. doi:10.1080/16089677.2016.1205822
- Patra S, Patro BK, Padhy SK, Mantri J. Prevalence of diabetes distress and its relationship with self-management in patients with type 2 diabetes mellitus. Ind Psychiatry J. 2021;30(2):234. doi:10.4103/ipj.ipj_60_19
- Zhang J, Xu C-P, Wu H-X, et al. Comparative study of the influence of diabetes distress and depression on treatment adherence in Chinese patients with type 2 diabetes: a cross-sectional survey in the People’s Republic of China. Neuropsychiatr Dis Treat. 2013;9:1289–1294. doi:10.2147/NDT.S49798
- Hu Y, Li L, Zhang J. Diabetes distress in young adults with type 2 diabetes: a cross-sectional survey in China. J Diabetes Res. 2020;2020:1–6. doi:10.1155/2020/4814378
- Gahlan D, Rajput R, Gehlawat P, Gupta R. Prevalence and determinants of diabetes distress in patients of diabetes mellitus in a tertiary care centre. Diabet Metabol Synd. 2018;12(3):333–336. doi:10.1016/j.dsx.2017.12.024
- Kasteleyn M, de Vries L, Van Puffelen A, et al. Diabetes‐related distress over the course of illness: results from the Diacourse study. Diabet Med. 2015;32(12):1617–1624. doi:10.1111/dme.12743
- Rook KS, August KJ, Choi S, Franks MM, Stephens MAP. Emotional reactivity to daily stress, spousal emotional support, and fasting blood glucose among patients with type 2 diabetes. J Health Psychol. 2016;21(11):2538–2549. doi:10.1177/1359105315581064
- Zanchetta FC, Trevisan DD, Apolinario PP, Silva J, Lima MHd M. Clinical and sociodemographic variables associated with diabetes-related distress in patients with type 2 diabetes mellitus. Einstein. 2016;14(3):346–351. doi:10.1590/S1679-45082016AO3709
- Parsa S, Aghamohammadi M, Abazari M. Diabetes distress and its clinical determinants in patients with type II diabetes. Diabet Metabol Synd. 2019;13(2):1275–1279. doi:10.1016/j.dsx.2019.02.007
- Bo A, Pouwer F, Juul L, Nicolaisen S, Maindal H. Prevalence and correlates of diabetes distress, perceived stress and depressive symptoms among adults with early‐onset type 2 diabetes: cross‐sectional survey results from the Danish DD2 study. Diabet Med. 2020;37(10):1679–1687. doi:10.1111/dme.14087
- Aljuaid MO, Almutairi AM, Assiri MA, Almalki DM, Alswat K. Diabetes-related distress assessment among type 2 diabetes patients. J Diabetes Res. 2018;2018:1–10. doi:10.1155/2018/7328128
- Chew B-H, Vos R, Mohd-Sidik S, Rutten GE, Hashimoto K. Diabetes-related distress, depression and distress-depression among adults with type 2 diabetes mellitus in Malaysia. PLoS One. 2016;11(3):e0152095. doi:10.1371/journal.pone.0152095
- Fayed A, AlRadini F, Alzuhairi RM, et al. Relation between diabetes related distress and glycemic control: the mediating effect of adherence to treatment. Prim Care Diabetes. 2022;16(2):293–300. doi:10.1016/j.pcd.2021.12.004
- Paddison C, Alpass F, Stephens C. Deconstructing distress: the contribution of cognitive patterns to elevated distress among people with type 2 diabetes. Euro Diabet Nurs. 2007;4(1):23–27. doi:10.1002/edn.72
- Kalra S, Balhara YPS. Insulin distress. US Endocrinol. 2018;14(1):27–29. doi:10.17925/USE.2018.14.1.27
- Onyenekwe BM, Young EE, Nwatu CB, Okafor CI, Ugwueze CV. Diabetes distress and associated factors in patients with diabetes mellitus in south east Nigeria. Dubai Diabet Endocrinol J. 2020;26(1):31–37. doi:10.1159/000508706
- Fisher L, Mullan JT, Arean P, Glasgow RE, Hessler D, Masharani U. Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longitudinal analyses. Diabetes Care. 2010;33(1):23–28. doi:10.2337/dc09-1238
- Wibowo ZK, Wibisono S, Khairina K. The relationship between diabetes distress and HbA1C level in type 2 diabetes mellitus therapy patients: a systematic review. Bali Medl J. 2022;11(1):476–484. doi:10.15562/bmj.v11i1.2986
- Hagger MS, Koch S, Chatzisarantis NL, Orbell S. The common sense model of self-regulation: meta-analysis and test of a process model. Psychol Bull. 2017;143(11):1117. doi:10.1037/bul0000118
- Hagger MS, Orbell S. A meta-analytic review of the common-sense model of illness representations. Psychol Health. 2003;18(2):141–184. doi:10.1080/088704403100081321
- Hudson JL, Bundy C, Coventry PA, Dickens C. Exploring the relationship between cognitive illness representations and poor emotional health and their combined association with diabetes self-care. A systematic review with meta-analysis. J Psychosom Res. 2014;76(4):265–274. doi:10.1016/j.jpsychores.2014.02.004
- Skinner TC, Skinner IK. Willpower beliefs and diabetes distress: a preliminary cross‐sectional study. Pract Diabet. 2021;38(1):11–16. doi:10.1002/pdi.2314
- Hapunda G. Coping strategies and their association with diabetes specific distress, depression and diabetes self-care among people living with diabetes in Zambia. BMC Endocr Disord. 2022;22(1):215. doi:10.1186/s12902-022-01131-2
- Lawson VL, Bundy C, Belcher J, Harvey JN. Changes in coping behavior and the relationship to personality, health threat communication and illness perceptions from the diagnosis of diabetes: a 2-year prospective longitudinal study. Health Psychol Res. 2013;1(2):20. doi:10.4081/hpr.2013.716