Abstract
Background
Type 2 diabetes is known to be associated with elevated cardiovascular mortality. Pioglitazone improves blood pressure (BP) and pulse wave velocity (PWV), which is an arterial stiffness parameter. Arterial stiffness is closely associated with cardiovascular disease. However, PWV is correlated with BP. The cardio-ankle vascular index (CAVI) reflects arterial stiffness independent of BP. Pioglitazone improves PWV but reduces blood pressure. The aim of this study was to re-evaluate the effect of pioglitazone on arterial stiffness with CAVI.
Methods
Sixty patients with type 2 diabetes mellitus and already on 500 mg/day of metformin received add-on therapy of pioglitazone 15 mg/day or glimepiride 1 mg/day for 6 months, during which time changes in their metabolic parameters and CAVI were observed.
Results
After 6 months of treatment, both pioglitazone (n=30) and glimepiride (n=30) improved fasting blood glucose and glycated hemoglobin. The changes in fasting blood glucose and glycated hemoglobin between the two groups were greater in the pioglitazone group. Systolic and diastolic BP was decreased in both groups, with no significant between-group differences. Only pioglitazone increased serum adiponectin levels, and the change in adiponectin between the pioglitazone and glimepiride groups was significantly different. CAVI was decreased significantly by pioglitazone but remained unchanged after treatment with glimepiride. The change in CAVI between the two groups was significantly different.
Conclusion
These results suggest that pioglitazone improves CAVI, a BP-independent arterial stiffness parameter, in patients with type 2 diabetes mellitus treated with metformin.
Introduction
Cardiovascular disease is a major cause of death in patients with type 2 diabetes.Citation1 Intensive glycemic control reduces microvascular complications; however, the effect on cardiovascular disease is rather limited.Citation2 Control of blood glucose levels is one of the principal purposes of treating diabetes; however, it has been difficult to demonstrate a beneficial effect of well controlled blood glucose on the macrovascular complications of diabetes.Citation3,Citation4 The United Kingdom Prospective Diabetes Study (UKPDS) demonstrated that the risk of cardiovascular morbidity and mortality was reduced in patients with type 2 diabetes receiving intensive glucose control using metformin.Citation5 Metformin improves insulin sensitivity and is thus important in the management of traditional cardiovascular risk factors, such as a high glycosylated hemoglobin (HbA1c) level, hypertension, dyslipidemia, and central obesity. All of these traditional cardiovascular risk factors are associated with insulin resistance.Citation6
Some nontraditional cardiovascular risk factors have been reported. Oxidized low-density lipoprotein (LDL), which represents one type of modified LDL, is considered to be important in the progression of atherosclerosis.Citation7 Adiponectin is a well known adipocytokine. The serum adiponectin level reflects the degree of insulin resistance.Citation8 The lipoprotein lipase mass level in preheparin serum (preheparin LPL mass) is associated with metabolic syndrome.Citation9
However, metformin monotherapy cannot always control hyperglycemia, and other hypoglycemic agents sometimes have to be coadministered. Sulfonylureas have been used as insulin secretagogues and are one of the most commonly used classes of antidiabetic agents. Thiazolidinediones (TZDs) are antidiabetic agents that reduce blood glucose to increase insulin sensitivity in peripheral tissues.Citation10 Antiatherogenic effects have been reported for both sulfonylureas and TZDs.Citation11,Citation12 TZDs have beneficial effects on lipid metabolism, such as enlarging LDL particle size in patients with type 2 diabetes.Citation13 In addition, TDZ improves pulse wave velocity (PWV) in Japanese diabetic patients.Citation14
Brachial-ankle PWV (baPWV) has been used to evaluate arterial stiffness and atherosclerosis. An arterial stiffness parameter, cardio-ankle vascular index (CAVI), was developed as a marker of arteriosclerosis involving the aorta, femoral artery, and tibial artery.Citation15 CAVI is measured from an electrocardiogram, phonocardiogram, brachial artery waveform, and ankle artery waveform and is adjusted for blood pressure (BP) based on the stiffness parameter β.Citation16 CAVI is independent of BP and has adequate reproducibility for clinical use, but baPWV is dependent on BP.Citation15 Indeed, baPWV is decreased by metoprolol, a β1-selective adrenergic receptor blocker with limited arterial effects.Citation17 On the other hand, CAVI is not decreased by metoprolol.Citation17 Both baPWV and CAVI are decreased by doxazosin, an α1-adrenergic receptor blocker with a strong vasodilating effect.Citation17 These results also indicate that CAVI, not baPWV, reflects arterial stiffness independent of BP. Although arterial stiffness can be evaluated by measuring either baPWV or CAVI, CAVI is superior to baPWV as an index of arterial stiffness in patients who have undergone coronary angiography.Citation16 Some reports indicate that CAVI is useful for detecting atherosclerotic diseaseCitation15,Citation18 and is superior to intima-media thickness for predicting coronary atherosclerosis.Citation19 We considered that we needed to re-evaluate the effect of TZDs on arterial stiffness with CAVI because pioglitazone decreases both BP and PWV, which is a blood pressure-dependent arterial stiffness parameter.Citation14
In this study, we reinvestigated the effect of TZDs on arterial stiffness with CAVI. We hypothesized that TZDs improve arterial stiffness by improving not only glucose metabolism but also some nontraditional cardiovascular risk factors. We administered sulfonylureas or TZD as add-on therapy in type 2 diabetic patients receiving metformin and evaluated the effect of the combination on CAVI, a BP-independent arterial stiffness parameter and a surrogate marker of cardiovascular disease.
Materials and methods
The study protocol was prepared in accordance with the Declaration of Helsinki and was approved by the institutional review board of Sakura Hospital, Toho University Medical Center (approval number 2012-114). Before participation, we explained the purpose of the study to each subject, and consent was obtained for both participation in this study and for release of the study data.
Study subjects
A randomized open-label study was performed. Sixty patients with type 2 diabetes (HbA1c >7.0%) were enrolled. At baseline, all subjects were treated solely with 500 mg/day of metformin, which acted as an oral hypoglycemic agent. We divided the patients into two groups by simple randomization using a closed envelope. One group was administered pioglitazone (a TZD) at 15 mg/day (pioglitazone group, n=30), and the other group was administered glimepiride (a sulfonylurea) at 1 mg/day (glimepiride group, n=30). shows the clinical characteristics of the subjects at baseline. All subjects were observed for 6 months after initiation of pioglitazone or glimepiride add-on therapy, and the following parameters were measured after 6 months: body weight, body mass index, fasting blood glucose, HbA1c, serum total cholesterol, triglycerides, high-density lipoprotein cholesterol, LDL cholesterol, preheparin LPL mass, adiponectin, and malondialdehyde-modified LDL levels, as well as LDL particle size and urinary albumin. Systolic BP, diastolic BP, and CAVI were also measured before and after 6 months. All patients maintained the same diet and exercise therapies and did not change medications during this study. A dietician provided nutritional guidance to all subjects on a monthly basis, analyzing meals and suggesting changes if necessary.
Table 1 Comparisons of baseline characteristics in the two groups
Measurement of body weight and blood sampling
Measurement of body weight and collection of blood were done in the morning after 12 hours of fasting. Serum was separated within one hour, and the sample was used to measure HbA1c, serum lipids, preheparin LPL mass, and adiponectin, and for analysis of serum lipoproteins by polyacrylamide gel disc electrophoresis.
Measurement of HbA1c and plasma lipid concentrations
To measure HbA1c, blood was collected in tubes containing ethylenediaminetetraacetic acid. The stable and unstable fractions of HbA1c were measured by a high-pressure liquid chromatography method (Hi-Auto A1c analyzer system; Kyoto Daiichi Kagaku, Kyoto, Japan). Stable form data were used in the present analysis. HbA1c was expressed as the value of the national glycohemoglobin standardization program (NGSP).
Plasma total cholesterol and triglyceride levels were measured enzymatically using kits from Nippon Shoji Co, Ltd (Osaka, Japan) and a 7150 analyzer (Hitachi, Ltd, Tokyo, Japan). Serum high-density lipoprotein cholesterol was measured using a selective inhibition assay (Daiichi Pure Chemicals Co, Ltd, Tokyo, Japan).Citation20 Serum LDL cholesterol levels were calculated using the Friedewald formula.
Serum preheparin LPL mass, adiponectin, and malondialdehyde-modified LDL
Serum preheparin LPL mass was measured by a sandwich enzyme-linked immunosorbent assay (ELISA) using a specific monoclonal antibody against LPL (Daiichi Pure Chemicals Co, Ltd), as described by Kobayashi et al.Citation21 The linearity and coefficient of variation are described in our previous report.Citation22 The serum adiponectin level was measured using an adiponectin ELISA system (Otsuka Pharmaceutical Co, Tokushima, Japan). The ELISA for malondialdehyde-modified LDL was based on the method reported by Kotani et alCitation23 and is described in our previous report.Citation22
Urinary albumin
The urinary albumin concentration was determined by turbidimetric immunoassay using a superior-microalbumin kit (LSI Medience Corporation, Tokyo, Japan). Urinary albumin was corrected for urinary creatinine concentration, which was measured by an enzymatic reaction.
LDL particle size
Serum lipoproteins were separated using polyacrylamide gel disc electrophoresis by the Lipo Phor™ system (Quantimetrix Corporation, Redondo Beach, CA, USA).Citation24 LDL particle size was evaluated by examining the relative mobility of the peak of LDL fraction (LDL-Rm) determined from the densitometric pattern (Densitron 20-HR; Jokoh Co, Ltd., Tokyo, Japan). The LDL-Rm is significantly correlated with LDL particle size, and a decrease in the Rm ratio indicates an increase in LDL particle size in polyacrylamide gel disc electrophoresis.Citation25
CAVI and systolic and diastolic BP
CAVI is obtained by measuring BP and PWV according to the following formula: CAVI = a{(2ρ/ΔP) × ln(Ps/Pd) PWVCitation2} + b, where Ps is systolic BP, Pd is diastolic BP, PWV is pulse wave velocity, ΔP is Ps − Pd, ρ is blood density, and a and b are constants. The details and measurement of CAVI are described in our previous reports.Citation15,Citation22 In the present study, CAVI was measured using a VaSera CAVI instrument (Fukuda Denshi Co, Ltd, Tokyo, Japan) as described previously.Citation15 Systolic and diastolic BP was measured at the same time as CAVI measurement.
Statistical analysis
The data are expressed as the mean ± standard deviation. Normal distribution was tested using the Shapiro–Wilk test. Normality was secured by logarithmic transformation, because some data were not normally distributed. Statistical analysis was performed using the Student’s t-test and analysis of variance. All analyses were performed using JMP computer software version 9.0 (SAS Institute, Cary, NC, USA). P-values of <0.05 were considered to be statistically significant.
Results
The mean patient age was slightly higher in the pioglitazone group. The mean body weight and body mass index were slightly lower and urinary albumin was slightly higher in the pioglitazone group than in the glimepiride group. However, these differences were not significant. At baseline, the mean CAVI was slightly higher in the pioglitazone group than in the glimepiride group (9.59±0.88 versus 9.32±1.44), although the difference was not significant. Other parameters were almost identical in the two groups ().
Body weight and body mass index were increased in both groups, and the increase in body weight and body mass index was significantly higher in pioglitazone group than in the glimepiride group (). Both pioglitazone and glimepiride reduced fasting blood glucose and HbA1c after 6 months of treatment. The change in fasting blood glucose was significant between the two groups. Serum adiponectin levels were increased only in the pioglitazone group. Comparison between the two groups revealed that the change of adiponectin was +6.43±4.89 ng/mL in the pioglitazone group and −0.09±3.04 ng/mL in the glimepiride group, representing a significant increase in the pioglitazone group (P<0.0001). The LDL-Rm ratio, which reflects LDL particle size, was decreased in the pioglitazone group and increased in the glimepiride group. These results indicate that LDL particle size in the pioglitazone group was increased. However, the difference between the two groups was not significant (P=0.0608, ). Other parameters were not significantly different between the two groups (). No drug-related adverse effects were observed in any of the patients.
Table 2 Comparisons of the differentiation of each clinical parameter after 6 months in the two groups
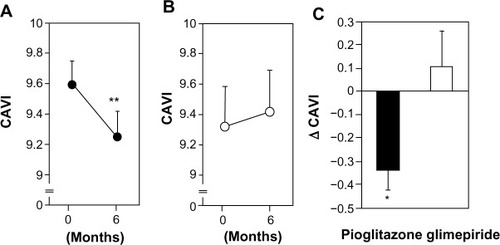
Pioglitazone significantly decreased the mean (standard error) CAVI from 9.59±0.16 to 9.25±0.17 (P<0.001) after 6 months (). Mean (standard error) CAVI increased slightly, but not significantly, in the glimepiride group (from 9.32±0.26 to 9.42±0.27; ). The changes in CAVI during this study are shown in . The mean (standard error) decrease in CAVI was significantly greater in the pioglitazone group than in the glimepiride group (−0.337±0.088 versus 0.107±0.151, P<0.05).
Figure 1 (A) Changes in cardio-ankle vascular index (CAVI) before and after 6 months of pioglitazone therapy. Data are presented as the mean ± standard error of the mean **P<0.01 versus 0 month, paired t-test. (B) Changes in CAVI before and after 6 months of glimepiride therapy. Data are presented as the mean ± standard error of the mean. (C) Changes in CAVI after 6 months of pioglitazone or glimepiride therapy. The closed bar denotes the pioglitazone group and the open bar denotes the glimepiride group. Data are presented as the mean ± standard error of the mean. Δ indicates the difference between the value at baseline and the value after 6 months. *P<0.05 versus glimepiride group, unpaired t-test.
The correlation between change in CAVI and changes in various parameters was analyzed in all subjects to clarify the important factors involved in the decrease in CAVI. Among the factors analyzed, changes in body weight, body mass index, adiponectin level, and LDL-Rm ratio had a significant correlation with a decrease in CAVI (). The changes in systolic and diastolic BP were not correlated with a change in CAVI. The change in fasting blood glucose was significantly different between the two groups, but was not correlated with the change in CAVI.
Table 3 Correlation between change in CAVI and changes in various parameters after 6 months in all subjects
Discussion
In the present study, pioglitazone as add-on therapy significantly increased body weight and body mass index and improved fasting blood glucose and serum adiponectin compared with glimepiride as add-on therapy in patients with type 2 diabetes receiving metformin. Only pioglitazone add-on therapy decreased CAVI significantly, whereas glimepiride add-on therapy did not decrease CAVI. The decrease in CAVI correlated with the increase in body weight, body mass index, serum adiponectin, and LDL-Rm ratio. There were no correlations between the change in CAVI and changes in systolic and diastolic BP.
Cardiovascular disease is a major cause of death in patients with type 2 diabetes.Citation1 Metformin, an insulin sensitizer, reduces the incidence of myocardial infarction compared with sulfonylureas.Citation5 This finding suggests that it is important to reduce insulin resistance in patients with type 2 diabetes mellitus. However, when metformin monotherapy cannot control blood glucose, should the next step of diabetes treatment be to increase insulin secretion or to reduce insulin resistance? In the present study, pioglitazone as add-on therapy improved CAVI, a surrogate marker of cardiovascular disease, in patients with type 2 diabetes who were already receiving metformin. Glimepiride as add-on therapy did not decrease CAVI in patients with type 2 diabetes on metformin. The change in fasting blood glucose was significantly different between pioglitazone and glimepiride, but was not correlated with the change in CAVI. Adiponectin, a well known marker of insulin resistance, was increased only in the pioglitazone group. The change in adiponectin between the pioglitazone and glimepiride groups was significantly different, and was correlated with the change in CAVI. Thus, our results suggest that reducing insulin resistance is more important than increasing insulin secretion in patients with type 2 diabetes not adequately controlled on metformin. Other clinical studies support our results.Citation26,Citation27
Although arterial stiffness is usually evaluated by baPWV, baPWV is correlated with BP.Citation17 In a previous study, pioglitazone improved baPWV but also decreased systolic BP.Citation14 Therefore, it is uncertain if pioglitazone improves arterial stiffness in diabetic patients, and we considered it necessary to evaluate the effect of pioglitazone on arterial stiffness with CAVI. We found that pioglitazone decreased systolic and diastolic BP. However, glimepiride also decreased systolic and diastolic BP, and these changes were not significant between the pioglitazone and glimepiride groups. Further, the change in CAVI was not correlated with changes in systolic or diastolic BP. Thus, we confirmed that pioglitazone improves arterial stiffness in type 2 diabetic patients.
Serum adiponectin reflects insulin resistance and is also related to atherosclerosis and cardiovascular disease. Serum adiponectin levels have an inverse correlation with the risk of high carotid intima-media thickness.Citation28 Further, there has been a clinical study showing that adiponectin has a strong association with aortic stiffness in patients after acute ST-segment elevation myocardial infarctionCitation29 and that serum adiponectin levels were increased more by pioglitazone than glimepiride. Thus, we conclude that serum adiponectin is an important factor in the mechanism via which pioglitazone improved CAVI in this study.
The LDL–Rm ratio, which reflects LDL particle size, correlated significantly with CAVI in patients with attenuated CAVI after 6 months in our present study. The LDL–Rm ratio was decreased in the pioglitazone group and increased in the glimepiride group. Small-sized LDL is a known risk factor for coronary heart disease.Citation30 Troglitazone, a TZD, has been observed to increase LDL particle size in a previous study.Citation13 We consider that enlargement of LDL particle size might be an important reason for the decrease in CAVI seen in the current study, although comparison of the change in LDL-Rm ratio between the two groups indicates that there was no significant difference.
Body weight and body mass index were significantly increased in the pioglitazone group compared with the glimepiride group, and these changes were correlated with the decrease in CAVI. CAVI was not correlated with body mass index in a previous study.Citation31 Pioglitazone is well known for increasing body weight. Only pioglitazone significantly decreased CAVI in our study. We consider the effects of pioglitazone to be the reason for the correlation between body weight or body mass index and CAVI.
Glimepiride decreased CAVI in type 2 diabetic patients not treated with metformin, and this attenuating effect on CAVI was due to improved insulin resistance.Citation32 In the present study, however, glimepiride add-on therapy did not increase adiponectin, a well known marker of insulin resistance.Citation8 We speculate that glimepiride is incapable of reducing insulin resistance in patients with type 2 diabetes who were already treated with metformin and, consequently, could not decrease CAVI in this study.
The main limitation of this study is its short duration of only 6 months. Thus, the long-term effect of pioglitazone and prognosis are still unclear. Further investigation with longer-term evaluations might be necessary. However, we were able to demonstrate an effect of pioglitazone on arterial stiffness in this study.
Conclusion
Pioglitazone add-on therapy in patients with type 2 diabetes already treated with metformin achieved improvement in CAVI, a BP-independent arterial stiffness parameter and a surrogate marker of cardiovascular disease. These effects were not observed with glimepiride add-on therapy. These results suggest that pioglitazone added on to metformin improves arterial stiffness independent of BP.
Author contributions
Masahiro Ohira worked on substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. Takashi Yamaguchi worked on acquisition of data. Atsuhito Saiki worked on acquisition of data. Noriko Ban worked on acquisition of data. Hidetoshi Kawana worked on acquisition of data. Ayako Nagumo worked on acquisition of data. Takeyoshi Murano worked on analysis and interpretation of data. Kohji Shirai worked on interpretation of data. Ichiro Tatsuno worked on analysis and interpretation of data. All authors worked on revising the article critically for important intellectual content, final approval of the version to be published and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
The authors report no conflicts of interest in this work.
References
- Lee WL Cheung AM Cape D Zinman B Impact of diabetes on coronary artery disease in women and men: a meta-analysis of prospective studies Diabetes Care 2000 23 962 968 10895847
- Stratton IM Adler AI Neil HA Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study BMJ 2000 321 405 412 10938048
- [No authors listed] UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet 1998 352 837 853 9742976
- Stettler C Allemann S Jüni P Glycemic control and macro-vascular disease in type 1 and 2 diabetes mellitus: meta-analysis of randomized trials Am Heart J 2006 152 27 38 16824829
- [No authors listed] UK Prospective Diabetes Study (UKPDS) Group Effect of intensive blood-glucose control with metformin on complication in over weight patients with type 2 diabetes (UKPDS 34) Lancet 1998 352 854 865 9742977
- Scarpello JH Howlett HC Metformin therapy and clinical uses Diab Vasc Dis Res 2008 5 157 167 18777488
- Koenig W Karakas M Zierer A Oxidized LDL and the Risk of Coronary Heart Disease: Results from the MONICA/KORA Augsburg Study Clin Chem 2011 57 1196 1200 21697499
- Weyer C Funahashi T Tanaka S Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia J Clin Endocrinol Metab 2001 86 1930 1935 11344187
- Saiki A Oyama T Endo K Preheparin serum lipoprotein mass might be a biomarker of metabolic syndrome Diabetes Res Clin Pract 2007 76 93 101 16956692
- Staels B Fruchart JC Therapeutic roles of peroxisome proliferator-activated receptor aonist Diabetes 2005 54 2460 2470 16046315
- Shakuto S Oshima K Tsuchiya E Glimepiride exhibits prophylactic effect on atherosclerosis in cholesterol-fed rabbits Atherosclerosis 2005 182 209 217 16159593
- Subramanian V Golledge J Ijaz T Bruemmer D Daugherty A Pioglitazone-induced reductions in atherosclerosis occur via smooth muscle cell-specific interaction with PPAR{gamma} Circ Res 2010 107 953 958 20798360
- Shirai K Itoh Y Sasaki H The effect of insulin sensitizer, troglitazone, on lipoprotein lipase mass in preheparin serum Diabetes Res Clin Pract 1999 46 35 41 10580614
- Kato T Sawai Y Kanayama H Comparative study of low-dose pioglitazone or metformin treatment in Japanese diabetic patients with metabolic syndrome Exp Clin Endocrinol Diabetes 2009 117 593 599 19924605
- Shirai K Utino J Otsuka K Takata M A novel blood pressure-independent arterial wall stiffness parameter; cardio-ankle vascular index (CAVI) J Atherosclerosis Thromb 2006 13 101 107
- Takaki A Ogawa H Wakayama T Cardio-ankle vascular index is a new noninvasive parameter of arterial stiffness Circ J 2007 71 1710 1714 17965489
- Shirai K Song M Suzuki J Contradictory effects of β1- and α1-aderenergic receptor blockers on cardio-ankle vascular stiffness index (CAVI)- CAVI independent of blood pressure J Atheroscler Thromb 2011 18 49 55 21071883
- Kubozono T Miyata M Ueyama K Clinical significance and reproducibility of new arterial distensibility index Circ J 2007 71 89 94 17186984
- Nakamura K Tomaru T Yamamura S Miyashita Y Shirai K Noike H Cardio-ankle vascular index is a candidate predictor of coronary atherosclerosis Circ J 2008 72 598 604 18362432
- Shirai K Nema T Hiroh Y Itoh Y Miyashita Y Watanabe H Clinical efficacy of the direct assay method using polymers for serum high density lipoprotein cholesterols J Clin Lab Anal 1997 11 82 86 9058241
- Kobayashi J Hashimoto H Fukamachi I Lipoprotein lipase mass and activity in severe hypertriglyceridemia Clin Chim Acta 1993 216 113 123 8222262
- Ohira M Endo K Oyama T Improvement of postprandial hyperglycemia and arterial stiffness upon switching from premixed human inuslin 30/70 to biphasic insulin aspart 30/70 Metabolism 2011 60 78 85 20667560
- Kotani K Maekawa M Kanno T Kondo A Toda N Manabe M Distribution of immunoreactive malondialdehyde-modified low-density lipoprotein in human serum Biochim Biophys Acta 1994 1215 121 125 7947993
- Mead MG Dangerfield WG The investigation of midband lipoproteins using polyacrylamide gel electrophoresis Clin Chim Acta 1974 51 173 182 4133339
- Miwa K Low density lipoprotein particles are small in patients with coronary vasospasm Int J Cardiol 2003 87 193 201 12559540
- Mazzone T Meyer PM Feinstein SB Effect of pioglitazone compared with glimepiride on carotid intima-media thickness in type 2 diabetes: a randomized trial JAMA 2006 296 2572 2581 17101640
- Nissen SE Nicholls SJ Wolski K PERISCOPE investigators Comparison of pioglitazone vs glimepiride on progression of coronary atherosclerosis in patients with type 2 diabetes: the PERISCOPE randomized controlled trial JAMA 2008 299 1561 1573 18378631
- Yoon JH Kim SK Choi HJ Adiponectin provides additional information to conventional cardiovascular risk factors for assessing the risk of atherosclerosis in both genders PLoS One 2013 8 e75535 24116054
- Reinstadler S Klug G Feistritzer H Relation of plasma adiponectin levels and aortic stiffness after acute ST-segment elevation myocardial infarction Eur Heart J Acute Caridiovasc Care 2014 3 10 17
- Austin MA Breslow JA Hennekens CH Buring JE Willett WC Krauss RM Low density lipoprotein subclass pattern and risk of myocardial infarction J Am Med Assoc 1988 260 1917 1921
- Nagayama D Endo K Ohira M Effects of body weight reduction on carido-ankle vascular index (CAVI) Obes Res Clin Pract 2013 7 e89 e164 24331770
- Nagayama D Saiki A Endo K Improvement of cardio-ankle vascular index by glimepiride in type 2 diabetic patients Int J Clin Pract 2010 64 1796 1801 20946343
