Abstract
Introduction
Human coronavirus (HCoVs) are a group of viruses with recognized neurotropic and neuroinvasive capabilities. The reports on the neurological and ocular findings are increasing day after day and several central and peripheral neurological manifestations are already described. However, none specifically describes the neuro-ophthalmological manifestation of HCoVs. This is the first article specifically reviewing neuro-ophthalmological manifestations of HCoVs infection.
Methods
PubMed and Google Scholar databases were searched using the keywords: coronaviridae, coronavirus, COVID-19, SARS-CoV-2, SARS-CoV-1, MERS, ocular, ophthalmology, ophthalmological, neuro-ophthalmology, neurological, manifestations. A manual search through the reference lists of relevant articles was also performed. There were no restrictions concerning language or study type and publications not yet printed but available online were considered.
Results
Coronavirus eye involvement is not frequent and includes mostly a typical viral follicular conjunctivitis. Recently, retinal anatomical alterations were described using optic coherence tomography. Neuro-ophthalmological symptoms and signs can appear isolated or associated with neurological syndromes. The manifestations include headache, ocular pain, visual impairment, diplopia, and cranial nerve palsies secondary to Miller Fisher syndrome, Guillain-Barré syndrome, or encephalitis, and nystagmus.
Conclusion
Neurological and neuro-ophthalmological syndromes, symptoms, and signs should not be neglected and a complete ophthalmological examination of these patients should be performed to fully describe ocular manifestations related to HCoVs. We believe that major ocular and neuro-ophthalmological manifestations reports lack due to safety issues concerning detailed ophthalmological examination; on the other hand, in a large number of cases, the presence of life-threatening coronavirus disease hinders ocular examination and ophthalmologist’s visit to the intensive care unit.
Introduction
Coronaviridae is a family of enveloped positive-strand RNA viruses that infect vertebrates and is currently constituted by 2 subfamilies, 5 genera, 26 subgenera, and 46 species.Citation1–Citation3
Seven coronaviruses (CoV) species are known to cause infections in humans – 229E (alphacoronavirus), NL63 (alphacoronavirus), OC43 (betacoronavirus), HKU1 (betacoronavirus) - the majority being responsible for mild upper respiratory disease. On the other hand, severe acute respiratory syndrome-related coronavirus-1 (SARS-CoV-1), and Middle East respiratory syndrome-related coronavirus (MERS-CoV) can cause severe respiratory distress, enteric and neurological disease with a mortality rate ranging from 10% to 36%.Citation4,Citation5 More recently, severe acute respiratory syndrome-related coronavirus-2 (SARS-CoV-2), also known as Coronavirus Disease 2019 (COVID-19), is responsible for affecting 5.105.881 people and causing 333.446 deaths in 216 countries, according to data reported on 23rd May 2020 by the World Health Organization.Citation6 Despite these representative numbers, non-respiratory clinical manifestations of the disease, namely ophthalmological and neuro-ophthalmological manifestations, are still not widely and well described. We believe this is partly due to the technical and safety issues concerning the detailed ophthalmological examinations of these patients and the legitimate tendency to neglect eye complaints at the expense of life-threatening manifestations.Citation7
Neurotropic and neuroinvasive capabilities of coronaviruses have been described in humans. It is proposed that coronavirus can reach and infect the central nervous system by several paths. Some suggested pathways include the hematogenous or lymphatic route, in which persistently infected leukocytes serve as reservoir and vector to Central Nervous System (CNS) infection and transneuronal retrograde dissemination following nasal infection and olfactory bulb involvement.Citation8,Citation9 The human host cell infection pathway is mediated by the angiotensin-converting enzyme 2 receptor for SARS-CoV-1 and SARS-CoV-2Citation10,Citation12 which proved to be present in the aqueous humorCitation13 but not in other parts of the eye.
This review article aims to describe the neuro-ophthalmological manifestations of human coronavirus (HCoV) infection. To date, this is the first article specifically reviewing this issue.
Methods
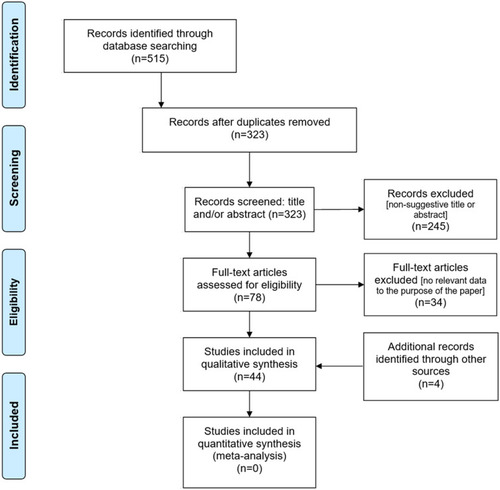
The authors searched PubMed/Medline and Google Scholar database using the following keywords: coronaviridae, coronavirus, COVID-19, Sars-Cov-2, Sars-Cov-1, MERS, ocular, ophthalmology, ophthalmological, neuro-ophthalmology, neurological, manifestations. The relevant articles were identified through the title and abstract information. The authors also performed a manual search through the reference lists of relevant articles. There were no restrictions concerning language or study type. Publications not yet printed but available online were considered. The literature review was last done on 23rd May 2020. The study flow diagram is represented in .
Figure 1 PRISMA flow diagram.
Ocular Non-Neuro-Ophthalmological Manifestations
Conjunctivitis and Keratoconjunctivitis
A report from Hubei Province in China reported 31.6% of ocular manifestations in COVID-19 patients consisting of chemosis, epiphora, conjunctival hyperemia, and secretion. Of these 12 patients, 11 had a positive nasopharyngeal swab but only two had a positive nasopharyngeal and conjunctival swab. One patient developed conjunctivitis as the first manifestation of the disease. The presence of eye symptoms appears to be associated with more severe analytical alterations such as higher white blood cell and neutrophil count, high C-reactive protein, lactate dehydrogenase, and procalcitonin levels.Citation15 This fact suggests that ocular manifestations are associated with more severe disease.
Itching, foreign body sensation, dry eyes, and floaters were also described symptoms during the course of COVID-19,Citation16,Citation17 as well as pseudomembranous and hemorrhagic conjunctivitis.Citation18
In another case series, Jianhua Xia et al described that one in 30 patients (3.3%) presented with conjunctivitis three days after disease onset, consisting of conjunctival hyperemia and aqueous secretion. Only this patient had a positive conjunctival swab for SARS-CoV-2.Citation19 No further ocular or neuro-ophthalmological manifestations were reported.
We only found two papers describing COVID-19 patients with external ocular signs of viral infection that were fully examined with a slit lamp and fundoscopic exam by an ophthalmologist.Citation20,Citation21 The first case reports a patient with ocular signs of infection 13 days after disease onset. A classic follicular conjunctivitis with a palpable preauricular lymph node and no subconjunctival hemorrhage or pseudomembrane was observed. Fundoscopic examination and macular structure and thickness analysis by optical coherence tomography (OCT) were normal.Citation20 No structural or functional imaging of the optic nerve was performed. The other case describes a keratoconjunctivitis as the initial presentation of COVID-19 with conjunctival follicular reaction and corneal subepithelial infiltrates.Citation21
Concerning the other HCoVs, polymerase chain reaction (PCR) of patient’s tears with SARS-CoV-1 demonstrated the presence of the virus during the global outbreak in 2003 but no clinical ocular manifestations were described.Citation22 Another human coronavirus, the HCoV NL63, was associated with conjunctivitis in a seven-month-old child.Citation23
HCoV infection can cause a typical viral follicular conjunctivitis with or without pseudomembrane development that appears in the majority of patients after disease onset but can be the inaugural or the only manifestationCitation15,Citation24–Citation26 of the disease.
Uveitis, Retinitis and Retinal Anatomical Alterations
Coronaviruses are capable of causing anterior uveitis, choroiditis, vasculitis, and retinitis in animalsCitation27 but these manifestations have not been described in humans. However, recently Paula Marinho et al in a study published on 12th May 2020 assessing the retina of 12 patients with COVID-19 found cotton wool spots and retinal hemorrhages on the fundus of four patients, and bilateral hyperreflective lesions in the ganglion cell and inner plexiform layers of all 12 patients using OCT.Citation28 Despite these lesions being more prominent at the papillomacular bundle, the visual acuity was normal.
Ocular non-neuro-ophthalmological manifestations of patients infected with HCoVs are represented in .
Table 1 Ocular Non-Neuro-Ophthalmological Manifestations of Patients Infected with HCoVs
Neuro-Ophthalmological Manifestations
Few studies have reported that human coronavirus may be associated with CNS involvement, namely acute encephalitis-like syndrome, acute disseminated encephalomyelitis, and multiple sclerosis.Citation29–Citation35 In animal models, CoVs have been related to an immune-mediated process of chronic demyelination of the CNS.Citation33 Despite the few associations between coronavirus and demyelinating disease, this effect in humans has not been directly proved and the association between these two entities is controversial.
Concerning the recent SARS-CoV-2, the reports on the neurological findings are increasing day after day and several central and peripheral neurological manifestations are already described such as dizziness, headache, seizures, changes in mental status, ataxia, acute cerebrovascular disease, CNS vasculitis, posterior reversible encephalopathy syndrome, acute necrotizing myelitis, encephalitis and taste and smell impairment.Citation36–Citation44 Associations with demyelinating diseases like Miller Fisher syndrome and Guillain-Barré syndrome were also described.Citation45–Citation49 Regardless of the increasing number of published data, none describes the specific neuro-ophthalmological manifestation of HCoVs.
The physiopathology of neurological involvement is still not fully understood. One of the theories suggests that coronavirus is a neurotrophic and neuroinvasive virus and that hypogeusia and anosmia are manifestations of peripheral nervous systems involvement and a way of infection into the nervous system.Citation11,Citation50 Since the central and peripheral nervous system can be affected, we believe that neuro-ophthalmological manifestations can occur.
Neuro-ophthalmological manifestations of patients infected with HCoVs are represented in .
Table 2 Neuro-Ophthalmological Manifestations of Patients Infected with HCoVs
Headache, Ocular or Periocular Pain
Headache has been reported as a major clinical symptom with 1.4% to 34% of COVID-19 patients and 71.1% healthcare workers with positive SARS-CoV-2 mentioning this symptom.Citation36,Citation37,Citation40,Citation53–Citation52 It is described as a pulsatile de novo headache, located over the temporoparietal region, the forehead or the periorbital region, relapsing and resistant to common-use analgesics.Citation59 Neuro-ophthalmological signs associated with this prevalent symptom were not described to date.
Ocular pain has also been reported and associated with SARS-CoV2 test positivity, along with headache, anosmia, myalgia, general malaise, tiredness and fever.Citation55
Pathophysiology of this symptom is still not fully understood. It appears to be associated with an increase of proinflammatory cytokines and a direct or indirect activation of the trigeminal nerve, rather than a direct COVID-19 CNS infection.Citation59 Regardless, when its development emerges associated with other neurological symptoms and signs, meningitis or encephalitis should be suspected as well other neurological syndromes.Citation36–Citation39
Visual Impairment
Visual impairment was described in three of 214 COVID-19 patients (1.4%) in WuhanCitation37 but the characteristics of vision loss such as onset, laterality, evolution, associated symptoms, and etiology were not reported. A lack of ophthalmological observation was also noted. This symptom along with hypogeusia, anosmia, and nerve pain constituted the peripheral nerve system manifestation of COVID-19 in the referred study.
Diplopia, Ophthalmoplegia and Ocular Cranial Nerves Palsy
Marc Dinkin et al described two cases of Sars-CoV-2 patients presented with diplopia and ophthalmoparesis.Citation45 The first is a 36-year-old man with an incomplete left third nerve palsy with pupillary involvement and a bilateral sixth nerve palsy associated with other neurologic symptoms. A diagnosis of Miller Fisher syndrome was presumed. The other case is a 71-year-old woman with an isolated right sixth nerve palsy that gradually improved two weeks later. In both cases, imaging of the CNS revealed an enhancement of the optic nerve sheaths and/or nerve enlargement and the lumbar puncture was normal for the second case.
Other cases of Miller Fisher syndrome and polyneuritis cranialis were reported by Gutiérrez-Ortiz et al.Citation56 Among other neurological signs, the patients presented with diplopia, afferent pupillary defect, internuclear ophthalmoparesis, and incomplete oculomotor palsy in the Miller Fisher syndrome case and esotropia and bilateral abducens palsy in the polyneuritis cranialis case. Multiple cranial neuritis involving the III and VI oculomotor nerves was also described through magnetic resonance imaging (MRI) in a patient diagnosed with Guillain-Barré syndrome associated with COVID-19, although no ocular movements disturbances were clinically described on the paper.Citation61
Concerning MERS-CoV, a complete external ophthalmoplegia and mild limb ataxia were observed in a patient diagnosed with Bickerstaff’s encephalitis and Guillain-Barré syndrome.Citation51
These reports provide an association between demyelinating disease and coronavirus. Cranial nerve involvement shown by CNS imaging suggests an inflammatory process/neuritis in which etiology is still unknown. Either a para-infectious, direct infection or demyelinating immune-mediated process can be speculated.
Peripheral Facial Nerve Palsy with Incomplete Blink
A progressive bilateral facial nerve palsy with unresponsive blink reflex was described in a 61-year-old patient with a facial diplegia presumed to be a variant of Guillain-Barré syndrome.Citation46 Complete ophthalmological examination was not performed in this patient, so other ocular manifestations of seventh nerve palsy such as lagophthalmos, upper eyelid retraction, lower eyelid ectropion, and dry eye are not known.
Other reports of Guillain-Barré syndrome in COVID-19 patients do not state ocular manifestations associated with facial weakness.Citation47,Citation62–Citation66
Nystagmus
Nystagmus was described as a sign of internuclear ophthalmoparesis in a SARS-CoV-2 patient who acutely presented with Miller Fisher syndrome and in a patient with bilateral abducens palsy.Citation56 In these patients, the optic disc examination was normal without optic disc edema.
Another case of horizontal nystagmus in a COVID-19 patient without respiratory symptoms was published. Pellitero et al described a case of a patient with a previous history of anosmia and ageusia three weeks before, that was observed for disequilibrium, nausea, and vomiting. Physical examination revealed horizontal nystagmus with a rapid phase to the right that worsens in dextroversion and oscilloscopy. Imaging of the CNS including MRI was normal. An acute vestibular dysfunction secondary to SARS-CoV-2 infection was the presumed diagnosis.Citation57
Pupillary Defects
Pupillary defects are reported in COVID-19 patients with Miller Fisher syndromeCitation45 due to oculomotor nerve involvement. Slow pupillary response was also described in a case of COVID-19 with encephalitis.Citation58
Optic Neuritis and Other Optic Disc Changes
Optic neuritis and chronic demyelination of the CNS were successfully demonstrated in animal coronavirus models.Citation27,Citation33 In humans, demyelinating disease such as acute disseminated encephalomyelitis, Miller Fisher syndrome, and Guillain-Barré syndrome was also described.Citation30,Citation45,Citation46 Associations between human coronavirus and multiple sclerosis are proposed and stated in the literature as an environmental factor.Citation31–Citation34 To date, there are no data demonstrating optic neuritis secondary to a HCoV infection in humans or HCoV demyelinating process.
Recently, an association between SARS-CoV-2 and a higher incidence of a severe Kawasaki disease was reported.Citation67 Although Kawasaki disease can exhibit ocular and manifestations such as conjunctival hyperemia, uveitis, vitreous opacities, and papilledema, none of these alterations were described in this study. Nevertheless, ocular symptoms and signs should be monitored.
Study Limitations and Strengths
There may be some possible limitations in this study. The current topic is very recent and specific information about neuro-ophthalmological manifestation is still scarce. Most of the published information consist of clinical cases or small case series, which makes generalization difficult. On the other hand, exponential published new data are available every-day and we believe that in the future there will be a better knowledge of the characteristics of human coronavirus, allowing a more solid and non-hypothetical base of knowledge.
To date, this is the first article reviewing neuro-ophthalmological manifestations of human coronavirus.
Conclusion
Human coronavirus can affect the central and peripheral nervous system; thus, neurological and neuro-ophthalmological syndromes, symptoms and signs should not be neglected. Complete ophthalmological examination of these patients should be performed to fully describe ocular manifestations related to HCoVs. The few data published consisting of small sample sizes studies, case series or isolated case reports preclude strong associations between these viruses and neurological and ophthalmological syndromes. We believe that major ocular and neuro-ophthalmological manifestations reports lack due to safety issues concerning detailed ophthalmological examination; on the other hand, in a large number of cases, the presence of life-threatening coronavirus disease hinders ocular examination and ophthalmologist’s visit to the intensive care unit.
Acknowledgments
The authors thank Dr Inês Albano, Family Medicine Doctor at Unidade de Cuidados Personalizados de Lagoa, for her contribution reviewing this manuscript.
Disclosure
There are no financial conflicts of interest to disclose. The authors report no conflicts of interest for this work.
Additional information
Funding
References
- Masters PS. The molecular biology of coronaviruses. Adv Virus Res. 2006;65(06):193–292. doi:doi:10.1016/S0065-3527(06)66005-3
- Siddell SG, Anderson R, Cavanagh D, et al. Coronaviridae. Intervirology. 1983;20:181–189. doi:10.1159/0001493906654644
- Virus Taxonomy: 2019 Release. ICTV (International Committee on Taxonomy of Viruses). Available from: https://talk.ictvonline.org/ictv-reports/ictv_9th_report/positive-sense-rna-viruses-2011/w/posrna_viruses/222/coronaviridae.
- Decaro N, Lorusso A. Novel human coronavirus (SARS-CoV-2): A lesson from animal coronaviruses. Vet Microbiol. 2020;244(April):108693. doi:doi:10.1016/j.vetmic.2020.10869332402329
- Gorbalenya AE, Baker SC, Baric RS, et al. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5(4):536–544. doi:doi:10.1038/s41564-020-0695-z32123347
- WHO Coronavirus Disease (COVID-19) Dashboard. Available from: https://covid19.who.int/.
- Gharebaghi R, Desuatels J, Moshirfar M, Parvizi M, Daryabari SH, Heidary F. Covid-19: preliminary clinical guidelines for ophthalmology practices. Med Hypothesis, Discov Innov Ophthalmol. 2020;9(2):149–158.32490022
- Desforges M, Le Coupanec A, Dubeau P, et al. Human coronaviruses and other respiratory viruses: underestimated opportunistic pathogens of the central nervous system? Viruses. 2019;12(1):1–28. doi:doi:10.3390/v12010014
- Desforges M, Le Coupanec A, Stodola JK, Meessen-Pinard M, Talbot PJ. Human coronaviruses: viral and cellular factors involved in neuroinvasiveness and neuropathogenesis. Virus Res. 2014;194:145–158. doi:doi:10.1016/j.virusres.2014.09.01125281913
- Hamming I, Timens W, Bulthuis MLC, Lely AT, Navis GJ, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631–637. doi:doi:10.1002/path.157015141377
- Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol. 2020;92(6):552–555. doi:doi:10.1002/jmv.2572832104915
- Heidary F, Varnaseri M, Gharebaghi R. The potential use of persian herbal medicines against COVID-19 through angiotensin-converting enzyme 2. Arch Clin Infect Dis. 2020 Online ahead of Print; 15(COVID–19):e102838. doi:doi:10.1136/bmj.m810
- Holappa M, Vapaatalo H, Vaajanen A. Many faces of renin-angiotensin system - focus on eye. Open Ophthalmol J. 2017;11(1):122–142. doi:doi:10.2174/187436410171101012228761566
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:7. doi:doi:10.1371/journal.pmed.1000097
- Wu P, Duan F, Luo C, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020;2019:4–7. doi:doi:10.1001/jamaophthalmol.2020.1291
- Zhou Y, Duan C, Zeng Y, et al. Ocular findings and proportion with conjunctival SARS-COV-2 in COVID-19 Patients. Ophthalmology. 2020. doi:doi:10.1016/j.ophtha.2020.04.028
- Hong N, Yu W, Xia J, Shen Y, Yap M, Han W. Evaluation of ocular symptoms and tropism of SARS‐CoV‐2 in patients confirmed with COVID‐19. Acta Ophthalmol. 2020;1–7. doi:doi:10.1111/aos.1444532749776
- Navel V, Chiambaretta F, Dutheil F. Haemorrhagic conjunctivitis with pseudomembranous related to SARS-CoV-2. Am J Ophthalmol Case Reports. 2020;19(May):100735. doi:doi:10.1016/j.ajoc.2020.100735
- Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS‐CoV‐2 infection. J Med Virol. 2020;92(6):589–594. doi:doi:10.1002/jmv.2572532100876
- Chen L, Liu M, Zhang Z, et al. Ocular manifestations of a hospitalised patient with confirmed 2019 novel coronavirus disease. Br J Ophthalmol. 2020;figure 2:1–4. doi:doi:10.1136/bjophthalmol-2020-316304
- Cheema M, Aghazadeh H, Nazarali S, et al. Keratoconjunctivitis as the initial medical presentation of the novel coronavirus disease 2019. Can J Ophthalmol Can D’ophtalmologie. 2020;2019:1–5. doi:doi:10.1016/j.jcjo.2020.03.003
- Loon SC, Teoh SCB, Oon LLE, et al. The severe acute respiratory syndrome coronavirus in tears. Br J Ophthalmol. 2004;88(7):861–863. doi10.1136/bjo.2003.03593115205225
- Van Der Hoek L, Pyrc K, Jebbink MF, et al. Identification of a new human coronavirus. Nat Med. 2004;10(4):368–373. doi:doi:10.1038/nm102415034574
- Daruich A, Martin D, Bremond-Gignac D. Ocular manifestation as first sign of coronavirus disease 2019 (COVID-19): interest of telemedicine during the pandemic context. J Fr Ophtalmol. 2020;43:389–391. doi:10.1016/j.jfo.2020.04.00232334847
- Pei X, Jiao X, Lu D, Qi D, Huang S, Li Z. How to face COVID-19 in ophthalmology practice. Med Hypothesis Discov Innov Ophthalmol. 2020;9(3):164–171.
- SirakayaE, SahinerM, Sirakaya HAA.A Patient with bilateral conjunctivitis positive for Sars-Cov-2 RNA in conjunctival sample.Cornea.2020 Jul 2:10.1097/ICO.0000000000002485.doi:10.1097/ICO.0000000000002485.Epub ahead of print
- Seah I, Agrawal R. Can the coronavirus disease 2019 (COVID-19) affect the eyes? a review of coronaviruses and ocular implications in humans and animals. Ocul Immunol Inflamm. 2020;28(3):391–395. doi:10.1080/09273948.2020.173850132175797
- Marinho PM, Marcos AAA, Romano AC, Nascimento H. Retinal findings in patients with COVID-19. Lancet. 2020;395:1610. doi:10.1016/S0140-6736(20)31014-X32405105
- Li Y, Li H, Fan R, et al. Coronavirus infections in the central nervous system and respiratory tract show distinct features in hospitalized children. Intervirology. 2017;59(3):163–169. doi:doi:10.1159/000453066
- Yeh EA, Collins A, Cohen ME, Duffner PK, Faden H. Detection of coronavirus in the central nervous system of a child with acute disseminated encephalomyelitis. Pediatrics. 2004;113(1):e73–e76. doi:10.1542/peds.113.1.e7314702500
- Murray RS, Brown B, Brain D, Cabirac GF. Detection of coronavirus RNA and antigen in multiple sclerosis brain. Ann Neurol. 1992;31(5):525–533. doi:doi:10.1002/ana.4103105111596089
- Stewart JN, Mounir S, Talbot PJ. Human coronavirus gene expression in the brains of multiple sclerosis patients. Virology. 1992;191(1):502–505. doi:doi:10.1016/0042-6822(92)90220-J1413524
- Wege H, Schluesener H, Meyermann R, Barac-Latas V, Suchanek G, Lassmann H. Coronavirus infection and demyelination: development of inflammatory lesions in Lewis rats. Adv Exp Med Biol. 1998;440:437–444.9782312
- Murray RS, MacMillan B, Cabirac G, Burks JS. Detection of Coronavirus RNA in CNS tissue of multiple sclerosis and control patients. Coronaviruses and their Diseases. Advances in Experimental Medicine and Biology 1990;276:505–510. doi:doi:10.1007/978-1-4684-5823-7_70
- Arbour N, Day R, Newcombe J, Talbot PJ. Neuroinvasion by human respiratory coronaviruses. J Virol. 2000;74(19):8913–8921. doi:doi:10.1128/JVI.74.19.8913-8921.200010982334
- Asadi-Pooya AA, Simani L. Central nervous system manifestations of COVID-19: A systematic review. J Neurol Sci. 2020;413:116832. doi:doi:10.1016/j.jns.2020.11683232299017
- Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020. doi:doi:10.1001/jamaneurol.2020.1127
- Werner C, Scullen T, Mathkour M, et al. Neurological impact of coronavirus disease (COVID-19): practical considerations for the neuroscience community. World Neurosurg. 2020. doi:doi:10.1016/j.wneu.2020.04.222
- Goldberg MF, Goldberg MF. Cerebrovascular DIsease in COVID-19. American Journal of Neuroradiology. 2020;41(7).
- Brouwer MC, Ascione T, Pagliano P. Neurologic aspects of COVID-19: A concise Review. Infez Med. 2020;28:42–45.32532937
- Saxena R, Singh D, Jethani J, et al. Pediatric ophthalmology, strabismus and neuro-ophthalmology practice in the COVID-19 era: all India Ophthalmological Society guidelines. Indian J Ophthalmol. 2020;68(7):1300–1305. doi:doi:10.4103/ijo.IJO_1789_2032587154
- Cariddi LP, Damavandi PT, Carimati F, et al. Reversible Encephalopathy Syndrome (PRES) in a COVID ‑ 19 patient. J Neurol. 2020;0123456789:5–8. doi:doi:10.1007/s00415-020-10001-7
- Hanafi R, Roger P-A, Perin B, et al. COVID-19 neurologic complication with CNS vasculitis-like pattern. AJNR Am J Neuroradiol. 2020;1–4.31924602
- Sotoca J, Rodríguez-Álvarez Y. COVID-19-associated acute necrotizing myelitis. Neurol Neuroimmunol Neuroinflam. 2020;7:e803. doi:doi:10.1212/NXI.0000000000000803
- Dinkin M, Gao V, Kahan J, et al. COVID-19 presenting with ophthalmoparesis from cranial nerve palsy. Neurology. 2020. doi:doi:10.1212/WNL.0000000000009700
- Juliao Caamaño DS, Alonso Beato R. Facial diplegia, a possible atypical variant of Guillain-Barré syndrome as a rare neurological complication of SARS-CoV-2. J Clin Neurosci. 2020. doi:doi:10.1016/j.jocn.2020.05.016
- Hutchins KL, Jansen JH, Comer AD, Scheer RV. COVID-19 – associated bifacial weakness with paresthesia subtype of Guillain-Barré syndrome. AJNR Am J Neuroradiol. 2020;1–5.31924602
- Webb S, Wallace VCJ, Martin- D, Yogarajah M. Guillain-Barré syndrome following COVID-19: a newly emerging post-infectious complication. BMJ Case Rep. 2020;3:e236182. doi:doi:10.1136/bcr-2020-236182
- Riva N, Russo T, Falzone YM, et al. Post‑infectious Guillain–Barré syndrome related to SARS‑CoV‑2 infection: a case report. J Neurol. 2020. doi:doi:10.1007/s00415-020-09907-z
- Li Z, Liu T, Yang N, et al. Neurological manifestations of patients with COVID-19: potential routes of SARS-CoV-2 neuroinvasion from the periphery to the brain. Front Med. 2020. doi:doi:10.1007/s11684-020-0786-5
- Kim JE, Heo JH, Kim HO, et al. Neurological complications during treatment of middle east respiratory syndrome. J Clin Neurol. 2017;13(3):227–233. doi:doi:10.3988/jcn.2017.13.3.22728748673
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020. doi:doi:10.1016/S0140-6736(20)30183-5
- Li R, Tian J, Yang F, et al. Clinical characteristics of 225 patients with COVID-19 in a tertiary Hospital near Wuhan, China. J Clin Virol. 2020;127(April):1–3. doi:doi:10.1016/j.jcv.2020.104363
- Zheng Y, Xiong C, Liu Y, et al. Epidemiological and clinical characteristics analysis of COVID-19 in the surrounding areas of Wuhan, Hubei Province in 2020. Pharmacol Res. 2020:104821. doi:10.1016/j.phrs.2020.104821.32360481
- Tostmann A, Bradley J, Bousema T, et al. Strong associations and moderate predictive value of early symptoms for SARS-CoV-2 test positivity among healthcare workers, the Netherlands, March 2020. Eurosurveillance. 2020;25:16. doi:doi:10.2807/1560-7917.es.2020.25.16.2000508
- Gutiérrez-Ortiz C, Méndez A, Rodrigo-Rey S, et al. Miller Fisher Syndrome and polyneuritis cranialis in COVID-19. Neurology. 2020. doi:doi:10.1212/wnl.0000000000009619
- Pellitero SE, Ferrer-Bergua LG. Paciente Con Clínica Neurológica Como Única Manifestación De Infección Por Sars-Cov-2. Neurología. 2020. doi:doi:10.1016/j.nrl.2020.04.010
- Xiang P, Xu X, Gao L, Wang H, Xiong H, Li R. First case of 2019 novel coronavirus disease with encephalitis. ChinaXiv. 2020.
- Bolay H, Gul A, Baykan B. COVID-19 is a real headache! 2020. doi:doi:10.1111/head.13856
- Zhu J. Clinical characteristics of 3062 COVID-19 patients: a meta-analysis Clinical characteristics of COVID-19: a meta-analysis. J Med Virol. 2020. doi:10.1002/jmv.25884
- Bigaut K, Mallaret M, Baloglu S, et al. Guillain-Barré syndrome related to SARS-CoV-2 infection. Neurol Neuroimmunol Neuroinflam. 2020;(7):e785. doi:doi:10.1212/NXI.0000000000000785
- Toscano G, Palmerini F, Ravaglia S, et al. Guillain–barré syndrome associated with SARS-CoV-2. N Engl J Med. 2020. doi:doi:10.1056/NEJMc2009191
- Scheidl E, Canseco DD, Hadji-Naumov A, Bereznai B. Guillain-Barre syndrome during SARS-CoV-2 pandemic: a case report and review of recent literature. J Peripher Nerv Syst. 2020. doi:doi:10.1111/jns.12382
- Zhao H, Shen D, Zhou H, Liu J, Chen S. Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol. 2020;19(5):383–384. doi:doi:10.1016/S1474-4422(20)30109-532246917
- Marta-Enguita J, Rubio-Baines I, Gastón-Zubimendi I. Síndrome de Guillain-Barré fatal tras infección por el virus SARS-CoV-2. Neurología. 2020. doi:doi:10.1016/j.nrl.2020.04.004
- Sedaghat Z, Karimi N. Guillain-Barre syndrome associated with COVID-19 infection: A case report. J Clin Neurosci. 2020. doi:doi:10.1016/j.jocn.2020.04.062
- Verdoni L, Mazza A, Gervasoni A, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020:1–8. doi:10.1016/S0140-6736(20)31103-X.
