Dear editor
In a recently published articleCitation1 moxalactam has been claimed to be very effective on extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella pneumoniae, concluding “MOX demonstrated excellent bactericidal effect, which is worthy of further exploration to serve as an alternative therapeutic agent against ESBL-producing Enterobacteriaceae”. Similar claims have also been made earlier.Citation2 Out of interest we examined antimicrobial sensitivity data with reference to sensitivity to moxalactam, carbapenem resistant, and extended-spectrum β-lactamase (EBSL) and metallo-β-lactamase (MBL) production, among clinically important bacteria from the last 6 years (2011–2017), available from the Division of Epidemiology at Indian Veterinary Research Institute, Izatnagar.
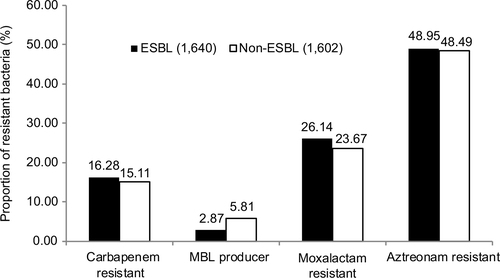
The analysis () revealed that conclusions drawn earlierCitation1,Citation2 on the basis of a study on a few strains may not be valid. My analysis revealed that of the 3,242 bacteria tested in our laboratory, using Clinical and Laboratory Standards InstituteCitation3 guidelines, 50.6% were identified as ESBL producers. Observations further revealed that moxalactam was certainly a more effective antibiotic on clinically important bacteria than most of the extended spectrum β-lactam antibiotics but no significant difference was detected between ESBL and non-ESBL producer bacteria with respect to their sensitivity to carbapenem (meropenem, imipenem and ertapenem), moxalactam and aztreonam. However, non-ESBL producing bacteria were more often positive for MBL production (p <0.001) than ESBL producing bacteria. Therefore, it may be suggested that observations on a few strains should not be used to draw a generalized statement the moxalactam is more effective on ESBL producer strains. It may give false message for misuse or undue preferences for moxalactum use.
Authors’ reply
Chen Huang, Yonghong Xiao
State Key Laboratory for Diagnosis and Treatment of Infectious Disease, Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, China
Correspondence: Yonghong Xiao, State Key Laboratory for Diagnosis and Treatment of Infectious Diseases, Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, The First Affiliated Hospital, College of Medicine, Zhejiang University, No 79 Qingchun Road, Hangzhou 310003, China Tel/fax +86 5 718 723 6421 Email [email protected]
Dear editor
We thank Dr Singh for his comments on our recently published article.Citation1 We are in favor of his view, “observations on a few strains should not be used to draw a generalized statement”. As we mentioned, moxalactam (MOX) is worthy of further exploration to serve as an alternative therapeutic agent against extended-spectrum β-lactamase (EBSL)-producing Enterobacteriaceae. Our data showed that MOX was more effective than cefotaxime and cefoperazone/sulbactam against ESBL-producing Enterobacteriaceae. However, it was not used for the treatment of metallo-β-lactamase (MBL) producers. Further explorations are still urgently needed so as to demonstrate stable efficacy of MOX against ESBL producers and decrease the usage of carbapenems. Moreover, our recent epidemiology antimicrobial surveillance isolated from bloodstream infections in China found that the resistance of ESBL producers to MOX was close to that of carbapenems (data not shown). In addition, we are confused regarding the data on Dr Singh’s . It was strange that the resistance rates to aztreonam in both ESBL- and non-ESBL-producing isolates were nearly identical, and ESBL producers were 48.95% resistant to aztreonam.
Finally, we are grateful for your attention to our published results.
Disclosure
The author reports no conflicts of interest in this communication.
Disclosure
The authors report no conflicts of interest in this communication.
References
- Huang C, Zheng B, Yu W, et al. Antibacterial effect evaluation of moxalactam against extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella pneumoniae with in vitro pharmacokinetics/pharmacodynamics simulation. Infect and Drug Resist. 2018;11:103–112.
- Ito A, Tatsumi Y, Wajima T, Nakamura R, Tsuji M. Potent antibacterial activities of latamoxef (moxalactam) against ESBL producing Enterobacteriaceae analyzed by Monte Carlo simulation. Jpn J Antibiot. 2014;67(2):109–122.
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Disk Susceptibility Tests. 24th Informational Supplement M100-S24 and M11-A8. Clinical and Laboratory Standards Institute, Wayne, PA. 2014.
Reference
- Huang C, Zheng B, Yu W, et al. Antibacterial effect evaluation of moxalactam against extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella pneumoniae with in vitro pharmacokinetics/pharmacodynamics simulation. Infect and Drug Resist. 2018;11:103–112.