Abstract
Background & Aims
Coronavirus disease 2019 (COVID-19) is a global health problem, presenting with symptoms ranging from mild nonspecific symptoms to serious pneumonia. Early screening techniques are essential in the diagnosis and assessment of disease progression. This consensus was designed to clarify the role of lung ultrasonography versus other imaging modalities in the COVID-19 pandemic.
Methods
A multidisciplinary team consisting of experts from different specialties (ie, pulmonary diseases, infectious diseases, intensive care unit and emergency medicine, radiology, and public health) who deal with patients with COVID-19 from different geographical areas was classified into task groups to review the literatures from different databases and generate 10 statements. The final consensus statements were based on expert physically panelists’ discussion held in Cairo July 2021 followed by electric voting for each statement.
Results
The statements were electronically voted to be either “agree,” “not agree,” or “neutral.” For a statement to be accepted to the consensus, it should have 80% agreement.
Conclusion
Lung ultrasonography is a rapid and useful tool, which can be performed at bedside and overcomes computed tomography limitations, for screening and monitoring patients with COVID-19 with an accepted accuracy rate.
Introduction
The coronavirus disease 2019 (COVID-19) is a pandemic caused by a novel coronavirus species named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Its clinical manifestations range from nonspecific symptoms, such as fever, nausea, and dry cough, to serious pneumonia.Citation1 Available evidence has recommended early therapy given its association with better and faster recovery.Citation2 This highlights the importance of early screening techniques hindering in the progression of the disease.
Unfortunately, real-time polymerase chain reaction (RT-PCR) has some limitations. First, it produces false-negative results when the viral load in the specimen is low, resulting in a low detection. Second, it cannot reflect disease incidence or forecast disease progression. Third, there is a reagent stock shortage, and new reagents require intensive research and development. Fourth, it is a time-consuming procedure. Because of these limitations, researchers suggest using computed tomography (CT) as the primary method for diagnosing COVID-19. Furthermore, patients clinically suspected to have COVID-19 with positive CT results but unfavorable PCR results, the patient should be isolated and managed as a positive case as soon as possible.Citation3 However, the number of cases may exceed the capability of the radiological department. Moreover, patients may be too ill to be moved, or the lack of staff and personal protective equipment (PPE) may preclude this possibility. Furthermore, equipment washing may cause delays in releasing test results. Finally, in resource-constrained environments, traditional radiology might not be available. Lung ultrasonography (LUS) is an excellent option during epidemics due to the lack of ionizing radiation contamination, ease of equipment sterilization, and significantly lower cost. Furthermore, low-cost portable ultrasound machines have recently been developed. These instruments could significantly reduce the costs of LUS implementations.Citation4
LUS may now be conducted immediately at the bedside by a single operator, eliminating the possibility of cross-contamination, limiting healthcare workers’ susceptibility to extreme acute SARS-CoV-2 infection, and minimizing PPE shortages in several healthcare settings.Citation5 Furthermore, the absence of radiation in LUS is crucial in patients who are more vulnerable to radiation toxicity, such as pregnant women, in which LUS is a reliable instrument for tracking COVID-19 progression.Citation6 Considering that, CT is not widely available in several developing countries, for confirming suspected COVID-19 cases, a comparatively inexpensive initial diagnostic and screening method is needed. Such a technique may be ultrasonography given its feasibility and portability and reliable sensitivity. However, ultrasonography is recommended to be used as an integrated diagnostic instrument.Citation7 Furthermore, in health care settings with inadequate resources, LUS with oxygen saturation monitoring can be is an effective method for determining the priority at which COVID-19 patients.Citation8 This context calls for better understanding on the features of LUS, such as its efficacy in both diagnosing and tracking the progression of lung diseases, including viral pneumonia. This consensus was designed to clarify the role of lung ultrasonography versus other imaging modalities in the COVID-19 pandemic.
Methods
For consensus development, We used Nominal Group Process and Consensus Development Panel. The chairperson and two coordinators of the consensus are members of the Egyptian scientific committee for management of COVID-19. They identified the research questions and the tasks of the consensus. They selected a multidisciplinary group consisting of experts in research and management of COVID-19 in Egypt. Selection of the expert group was based upon their practical input in diagnosis and treatment of COVID-19, their publication in the field of the consensus, their input in epidemiological research and their representation for the specialties included in management, namely tropical medicine, infectious diseases, pulmonology, emergency medicine, radiology, and epidemiology. The expert also represented most of Egyptian Universities and different geographical areas in Egypt.
Four tasks were identified:
Importance of imaging study in managing COVID-19.
Comparing the role of LUS in the diagnosis and follow-up of COVID-19 compared with that of other imaging modalities.
LUS criteria for the diagnosis of COVID-19.
Safety and infection control regulations for the use of LUS.
The group has been classified into task groups. Each group was responsible for reviewing the literature from different databases, including PubMed, Cochrane Library, and Scopus, to better understand and abstract the responses to the task.
The statements generated by each group were recirculated anonymously by the chairperson among the entire group using the WhatsApp application. Each member reviewed the statements and provide their comments. After obtaining feedback the statements were reviewed again by the task groups after getting the feedback who then made changes.
A multidisciplinary expert group consisting of 32 delegate members held a face to face meeting for 6 h on July 16, 2021. Each statement was presented by one of the task groups, including the statement’s evidence. The presenter and facilitator responded to the group questions. After discussing each statement, an anonymous electronic voting was run. Each statement was voted as either “agree,” “disagree,” or “neutral.”
The statement should have a predefined score of 80% agreement to be accepted and reported in this manuscript.
Summary of the Statements and Their Percentage of Agreement ()
Statement 1
Objective staging of the disease severity and evaluation of the course of infection help make proper treatment choices and improve prognosis. Consequently, this would reflect the reduction in the chain of transmission and the overall morbidity and mortality from COVID-19.
Table 1 Summary of the Statements and Their Percentage of Agreement
Rationale
COVID-19 was classified as a class B infectious disease by the Centers for Disease Control and Prevention (CDC) on January 20, 2020.Citation9 Even with substantial suppression measures in place, there may be shortage of beds, physicians, oxygen, and PPE. Because of measures, such as school lockdowns and distance restrictions, poverty and undernutrition may increase, where as educational achievement and recent gains in access to health care may decrease.Citation10
The most essential steps in controlling COVID-19 are rapid case detection, severity assessment, and contact tracing because they allow close contacts or even suspected persons to be identified, isolated, and tested for the disease.Citation11
The uncertainty in the clinical symptoms of COVID-19 is a challenge, and atypical patients must be carefully diagnosed since they may serve as carriers of the disease in the community. In addition to clinical criteria (pneumonia with fever and cough without or with indications of hypoxia), COVID-19 case definition considers radiological criteria (because “some cases may have no clinical signs or symptoms; however, chest CT or LUS shows subclinical lung lesions”).Citation12
Staging is a method for determining the severity of a disease based purely on predetermined diagnostic criteria to provide information regarding the illness severity during hospitalization.Citation13 With such information, we can establish a diagnosis, recommend a treatment plan, and predict the outcomes.Citation14 Otherwise, the more delays in diagnosis; the higher the death rates.Citation15
In developing countries, such as Africa, COVID-19 management options may be restricted given that the epidemic’s peak capacity may be several fold larger than the baseline capacity.Citation16
LUS is a safe and simple method for monitoring pneumonia and other respiratory diseases.Citation17
Statement 2
Indication for Lung Imaging
Given that respiratory dysfunction is the main cause of morbidity and mortality in patients with COVID-19, lung imaging is considered a key tool for assessing the disease.
Lung imaging is indicated for the medical triage of patients suspected to have COVID-19, who present with moderate to severe disease. It also helps to determine the proper site for patient’s care: home, hospital ward, or intensive care unit.
Imaging may also be advised to assess disease progression during the follow-up of confirmed COVID-19 cases.
Rationale
Lung imaging is the cornerstone for the diagnosis and severity classification of SARS-CoV-2 infection according to the National Institute of Health guidelines.Citation18 It is essential in diagnosing moderate and severe disease.
The observed abnormalities on chest X-rays vary; however, bilateral multifocal opacities are the most common. The observed abnormalities in chest CT also vary; however, bilateral peripheral ground-glass opacities (GGOs) are the most common findings, with consolidation areas occurring later in the clinical course of COVID-19. Imaging results may be normal early in infection and can be abnormal in the absence of symptoms.Citation19
A meta-analysis of 28 studies involving 2655 patients has reported that chest CT is helpful for not only the diagnosis of the disease but also the assessment of disease progression based on follow-up chest CT scans.Citation20
Latrice et al reported that chest X-ray could be used as the first-line imaging modality in areas with high levels of contagion and in the serial evaluation of hospitalized and critically ill patients. In contrast, high-resolution CT (HRCT) showed a low specificity in areas with a low prevalence of disease and should be considered the modality of choice in determining differential diagnoses with other infectious and noninfectious lung diseases and in managing patients with preexisting lung disease.Citation21
Yassa et al recommended LUS for asymptomatic pregnant patients with positive PCR for whom CT is not planned and those with initial negative CT findings for follow-up. Also, in those with mild symptoms who do not give consent for chest CT. In addition, abnormal LUS imaging in a symptomatic patient with “mild” clinical severity can be suggestive of a probable bad prognosis, particularly in pregnant women.Citation22
Statement 3
Chest CT is more sensitive and effective in triaging or following up patients with COVID-19 than chest X-ray.
The typical HRCT pattern consists of multiple GGOs mainly in the peripheral lung regions and basal distribution.
GGOs may be combined with other features, such as pulmonary consolidation, crazy paving, halo signs, basal reticulations, and vascular enlargement.
Rationale
CT findings differ according to the stage and severity of the disease and associated comorbidities. The sensitivity of CT depends on the duration of symptoms. Negative CT findings were reported in 56% of cases scanned within 2 days after the onset of symptoms, whereas negative scans were reported in 9% of cases who underwent CT within 3–5 days and 4% of those scanned 6–12 days after symptom onset.Citation23,Citation24
CT has a higher sensitivity than RT-PCR. Accordingly, CT has a sensitivity of 97.2%, whereas initial rRT-PCR has a sensitivity of 83.3%. Microbiological tests, such as rRT-PCR, may not be available in emergency situations, and their results take 4–5 days. Moreover, rRT-PCR can provide false-negative results when the viral load is insufficient,Citation25 with other reasons including improper sampling, the timing of sampling, or laboratory issues.Citation26
In the early stages of the disease, the typical HRCT pattern consists of single or multiple GGOs, mainly distributed in the subpleural and basal regions, which continue to expand as the disease progresses. In the later stages of COVID-19, GGO is often combined with other imaging features, such as pulmonary consolidation, crazy paving, halo signs, basal reticulations, and vascular enlargement. Thus, during pandemics, similar to the current situation, chest CT can be used as a tool for screening symptomatic patients as it is cheap, readily available, given its lower cost, ready availability, and rapid results.Citation27–32
Statement 4
The limitations of chest CT during the COVID-19 pandemic in developing countries include burden, cost, unavailability, infection, repetition, and exposure to ionizing radiation.
Rationale
The number of cases may exceed the capability of the radiological department. Moreover, patients may be too ill to be moved, or the lack of staff and PPE may preclude this possibility. Furthermore, equipment disinfection may delay the speed of tests. Finally, in resource-constrained environments, traditional radiology may not be available at all. Thus, the use of CT has been widely used as an initial screening and diagnostic technique for viral pneumonia (including COVID-19). Normal radiology imaging can have certain shortcomings in a pandemic.Citation3
In the early stages of COVID-19, lung involvement may precede clinical manifestations and even positive PCR swab test. Thus, early chest CT is recommended for screening suspected patients.Citation33 The high contagiousness of SARS-CoV-2 and the difficulties of moving sick patients (in ICU), in addition to radiation hazards and its unavailability in primary healthcare centers, are obstacles limiting the use of CT and necessitate the use of a more practical alternative.Citation34
The need for CT increases the burden in many healthcare centers worldwide, including chest and/or fever hospitals. Accordingly, Egypt can be considered one of the lower-middle-income countries with limited resources.Citation35
Statement 5
LUS allows for a rapid bedside testing that does not involve exposure to ionizing radiation, has a lower cost, and can be repeated (whenever indicated) without significant risks to the patient.
Rationale
LUS had an accuracy similar to that of chest CT in detecting lung abnormalities in patients with COVID-19. It is a highly sensitive and specific approach that can be used instead of CT, with the additional value of being rapid, easy to use, readily available. Moreover, it can be used at the bedside and can be repeated without exposure to radiation hazards.Citation35 Hense, LUS can be used in triaging symptomatic cases, assessing lung damage severity, and evaluating disease progression.Citation36 LUS is an excellent option during epidemics due to the lack of ionizing radiation contamination, ease of equipment sterilization, and significantly lower cost. Furthermore, low-cost portable ultrasound machines have recently been developed, which could significantly reduce the costs of LUS implementations, in terms of both buying and shipping the equipment.Citation4
LUS may now be immediately performed at the bedside by a single operator, eliminating the chance of cross-contamination, limiting health care workers’ susceptibility to extreme acute SARS-CoV-2 infection, and alleviating PPE shortages in several health care settings.Citation5 Furthermore, the absence of radiation in LUS is crucial for patients who are more vulnerable to radiation toxicity, such as pregnant women, in whom LUS is a reliable instrument for tracking COVID-19 disease progression.Citation6
Statement 6
a: A normally aerated lung is characterized by the presence of the following:
Bright, thin, smooth pleural line between two ribs.
Lines that are repeated horizontal artifacts parallel to the pleural line.
Normal lung sliding.
Rationale
In the normal aerated lung, more than 99.9% of ultrasound beams at the visceral pleura–lung air boundary. This boundary appears as a white, bright, thin, smooth band (pleural line) measuring up to 2 mm, seen 0.5 cm deeper between upper and lower ribs.Citation8,Citation37 The appearance of two ribs and a pleural line in between them is called the bat sign. Beyond this pleural line, reverberation artifacts produced by the bouncing of echoCitation38 between the pleural line and probe can be observed. These motionless, regularly spaced (equal to the distance between the skin and the pleural line) and gradually fading horizontal white lines, which resemble the pleural line, are called A-lines () (A profile).Citation39
Figure 1 Lung ultrasonography of a mild COVID-19 case with a normal aerated lung. (A) A bright, thin, smooth pleural line between the two ribs and A-lines are seen as horizontal repetitions of the pleural line between the shadows of the two ribs. (B) Normal lung sliding (seashore sign using M mode). T: T lines are vertical lines, in time with cardiac pulsation, running from the pleural line to the bottom of the image.
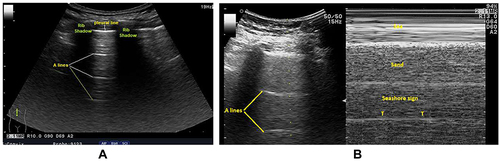
Movement of the visceral pleura over the parietal pleura produces lung sliding, and this white band appears dynamic. Lung sliding is the depiction of a regular rhythmic movement synchronized with respiration occurring between the parietal and visceral pleurae that are either in direct apposition or separated by a thin layer of intrapleural fluid. Lung sliding indicates ventilation in the inspected area. In time motion mode (M mode), the structures until the parietal pleura appear as horizontal lines, and this sandy pattern represents lung sliding. This finding is called the seashore sign (). The presence of the pleural line, lung sliding, A-lines in 2D, and seashore sign in the M mode means an aerated lung.Citation40–43
b: A poorly aerated lung is characterized by multiple B-lines, irregular pleural lines with or without subpleural consolidative patterns on LUS.
Moderate loss of lung aeration (interstitial syndrome): multiple (>3) spaced B-lines. This corresponds to a “ground-glass area” on lung HRCT.
Severe aeration loss (diffuse alveolar edema): diffuse coalescent B-lines occupying most of the intercostal space.
Complete aeration loss (lung consolidation [C]): the presence of a tissue pattern characterized by dynamic air bronchograms.
Rationale
SARS-CoV-2 infection initially presents as first proceeds with an interstitial inflammatory infiltrate, resulting in alveolo-interstitial pneumonia and endothelial damage.Citation44 In the early stages of COVID-19, changes in the lungs are localized and mainly found in the subpleural area of one or both lungs.Citation45 LUS showed irregular thickening of the pleural lines, which progressed to the formation of B-lines and loss of A-lines ().Citation38,Citation46 Later, the pathology involves multiple lobes, leading to more air loss and consolidations of some lesions surrounded by several B-lines ().Citation45 Fluid accumulations in the subpleural interstitium and alveolar spaces change the air–fluid ratio and form this characteristic artifact (ie, B-lines). The B-lines are defined as discrete laser-like vertical hyperechoic reverberation artifacts starting from the pleural line and extend to the bottom of the screen without fading and moving synchronously with lung sliding.Citation47 A positive region “B-pattern” is defined as the presence of three or more B-lines in a longitudinal plane between two ribs.Citation8,Citation47–50 Multiple B-lines are correlated with the ground-glass areas on lung CT of confirmed COVID-19 cases.Citation5 Multiple B-lines range from focal to multifocal, spaced, or continuously fused (confluent) B-lines (white-lung sign) with the disappearance of A-lines according to disease stage.Citation51
Figure 2 LUS of a patient with COVID-19 with a partially de-aerated lung showing the absence of A-lines, bilateral peripheral multiple spaced (B) B-lines (A), and thick and/or irregular pleural line, subpleural consolidation, and confluent B-line (B).
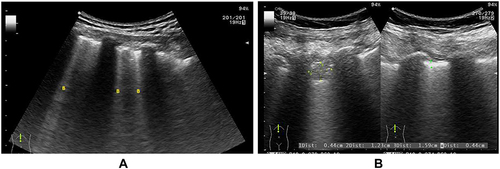
Over time, subpleural consolidations start to appear and spread bilaterally on both the posterior lower lobes on LUS. When a complete consolidation of the lung occurs, the echo structure of the lung itself becomes visible with characteristic air bronchogram, representing the air inside alveoli or bronchi surrounded by inflammation or pus; and the pleural lines are completely obscured.Citation51–54
The characteristic ultrasonographic findings of COVID-19 lung involvement includes thickening irregularity of the pleural line; in various B-lines patterns (ie, focal, multifocal, and confluent); and consolidations with occasional mobile air bronchograms.Citation37,Citation38,Citation52,Citation53,Citation55–60 In COVID −19-induced acute respiratory distress syndrome (ARDS), LUS shows a white area in which neither A-lines nor separated B-lines are visible. This presentation is called a “white lung”.Citation38
However, B-lines are non-specific artifacts associated with increased extravascular lung water or partial loss of lung aeration,Citation46 and they can be detected in a variety of pulmonary diseases, including interstitial lung disease, heart failure, acute respiratory distress syndrome, etc. However, LUS manifestations in COVID-19 patients shared not only the features of an increase in B-lines but also consolidations, irregular or blurred pleural line.Citation61
Statement 7
During the COVID-19 pandemic, the presence of multiple (≥3) B-lines with or without subpleural consolidations distributed bilaterally, peripherally, or basally in patches with spared areas on LUS is highly suggestive of COVID-19 pneumonia in clinically suspected patients.
Rationale
Chest ultrasonography showed predominant affection of the posterior and inferior areas of the lung (lower lobes).Citation55 Simultaneous affection of the upper lobe was associated with a more severe clinical course.Citation62 Bilateral, peripheral, and multilobar lung lesions have been frequently found in patients with COVID-19 on chest US and confirmed by CT.Citation26,Citation63,Citation64 Moreover, 94% of patients with confirmed COVID-19 demonstrated pathological B-lines (), with 82% of them showing bilateral distribution in. The multifocal appearance of B-lines was predominantly found in 59% of patients. Pleural irregularities occurred mostly occurred bilaterally (89%). Pulmonary consolidations, which are characterized by a rather focal and mostly subpleural appearance presenting frequently in not only the basal but also apical parts of the lung were found in 77% of COVID-19 cases. Abnormal lung sliding was observed in only 17% of patients, especially those with multifocal consolidations.Citation54,Citation62,Citation65 Patchy distribution () of spaced or confluent B-lines and small white-lung regions were observed in patients with early COVID-19. As the disease progresses, patchy small subpleural consolidations appear with associated areas of white lung.Citation2 The LUS findings of 197 patients (81.1%) were completely coincident with CT findings with a Kappa agreement value of 0.77, and this offered a diagnostic sensitivity of 74%, a diagnostic specificity of 97.9%, positive predictive value of 90.2%, and negative predictive value of 93.6% for LUS in triaging patients with COVID-19.Citation8 The World Health Organization defines cases having the following LUS features as those with probable COVID-19: thickened pleural lines, B-lines (multifocal, discrete, or confluent), and consolidative patterns with or without air bronchograms.Citation22,Citation65
Figure 3 B-lines with patchy distribution and spared areas. Left: Speared area with A-pattern; smooth pleural line and A-lines. Right: B-pattern; irregular pleural line and multiple spaced B-lines (poor lung aeration).
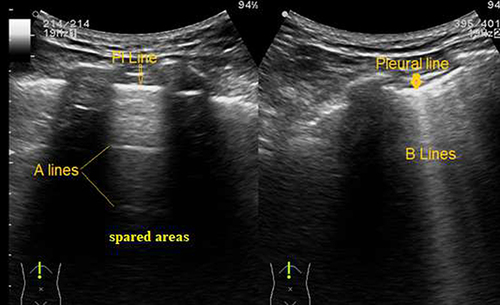
Unlike to COVID-19 pneumonia, ultrasound images of community-acquired pneumonia often show large and circumscribed consolidation accompanied by bronchial gas phase or liquid phase and pleural effusion. Consolidations were more extensive in bacterial pneumonia. Lung tissue was completely degassed and exhibited a solid tissue echo “a pattern showing” “hepatic-like changes”.Citation66
Statement 8
The LUS score based on the examination of 12 standard regions can be used to assess lung aeration changes and follow up disease progression.
Rationale
LUS score can measure the loss of lung aeration produced by diverse pathological situations.Citation67,Citation68 Some studies have proven that LUS could predict the outcomes in patients with SARS-CoV-2 infection. LUS has been strongly correlated with lung involvement and provides risk stratification, including prediction of mechanical ventilation requirement and mortality risk.Citation69,Citation70 To assess the disease severity, different protocols for the LUS scoring system () had been developed. The emergency department LUS protocol for patients with COVID-19 using bedside LUS, can grade disease severity and help clinicians make appropriate decisions and follow up patients with COVID-19. Patients can be examined in the sitting position. When such a position was not possible due to worsening clinical condition or lack of compliance, the examination could be performed in the supine, semi-recumbent, or lateral decubitus positions on both sides.Citation71
Table 2 Different Protocols for the Lung Ultrasound Scoring System
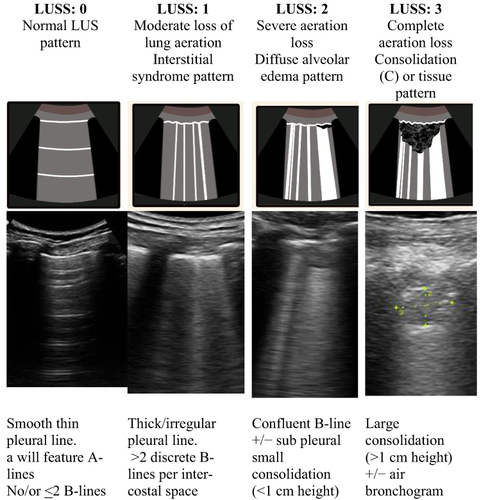
The LUS protocol involves the examination of 12 lung regions, with the entire procedure taking approximately 5 min when performed by an experienced physician.Citation72 On each side, six lung regions of interest (), delineated by a parasternal line, anterior axillary line, posterior axillary line, and paravertebral line, are examined.Citation71 Each region is scored from 0 to 3 according to four ultrasound aeration patterns (): 0 = normal aeration, 1 = interstitial syndrome, 2 = alveolar edema, and 3 = consolidation.Citation70–72 The final LUS score is the sum of the points across in all 12 regions and ranges from 0 to 36.Citation74,Citation75
Figure 4 The lung ultrasonography score, based on the examination of 12 regions of interest (six on the right side and six on the left side), has been proposed to assess lung aeration changes caused by different pathological lung conditions. PSL: AAL: PAL: PVL.
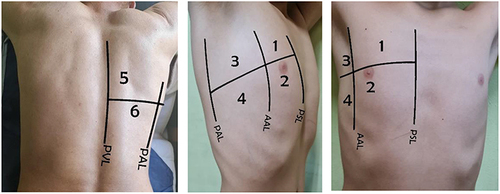
Figure 5 LUS score (LUSS) according to sonographic pattern: For each region, we allocated points, ranging from 0 to 3, according to the poorest ultrasound pattern observed. 0 = normal aeration, 1 = interstitial syndrome, 2 = alveolar edema, and 3 = consolidation. The final LUSS is the sum of the points in all 12 regions, which ranges from 0 to 36. Accordingly, the grading the disease severity index can be estimated: mild (score <5), moderate (<15), and severe (>15).
We seek from this statement to help physicians in ICU and ER, not only sonographers, to practice lung sonography in a simple, fast, and applicable technique. This technique includes well-known 12 lung zones and well-known anatomical lines as if they are employing the ultrasound probe as their stethoscope. The LUS score (0–3) does not only aid in the diagnosis of COVID-19 pneumonia but also helps in triaging COVID patients in ER, predicting outcomes and the need for invasive mechanical ventilation, and follow-up of these patients.Citation76 Volpicelli et al conducted an international multisystem study on 1462 patients. In this study, all intercostal spaces were evaluated in 5 scans (see ), additional scans were done to evaluate focal abnormalities, many video clips were captured to evaluate series of intercostal spaces per area, both the ultrasound convex and linear probes were used, intercostal spaces were evaluated in longitudinal and oblique views with additional tilting to optimize visualization of pleura. However, this study helps only in the early diagnosis of COVID-19, lacking the advantage of follow-up and predicting outcomes of COVID-19 patients.Citation77
Statement 9
Bedside LUS, by a well-trained physician or expert, is a useful screening and monitoring tool for suspected or confirmed COVID-19 cases, with an acceptable accuracy rate.
Rationale
LUS has an established accuracy for diagnosing lung diseases. It can be used for daily assessment and monitoring of patients with COVID-19. Growing literature and international networks have encouraged using LUS to diagnose COVID-19 pneumonia.Citation78 LUS results are similar to those obtained by HRCT and outperform the standard chest X-ray results for assessing pneumonia and ARDS, with additional benefits of ease of use in point of care and acceptable accuracy.Citation79
Thus, LUS may assist in tracking the clinical disease course and treatment outcomes and altering ventilator settings in severely ill patients or those undergoing mechanical ventilation.Citation7,Citation80,Citation81 LUS has shown high sensitivity to pulmonary lesions and can overcome the time gap for transferring patients to the CT unit.Citation82 Moreover, it can show the resolution of lung pathology after 96 h of admission.Citation79
In the United States, point of care ultrasonography training is highly recommended in programs for internal medicine residency evaluated the efficacy of a 2-week ultrasound elective training for internal medicine residents including acquisition and retention of knowledge and performing thoracic ultrasonography.Citation83 They concluded that the interactive ultrasound elective training for 2 weeks demonstrated efficacy in knowledge acquisition and retention related to ultrasound.Citation84,Citation79
Statement 10
Infection Control is Paramount
-National and local guidelines on PPE usage should be followed.
-The probe should be disinfected before and after patient examination to avoid nosocomial infections and cross-contamination.
Rationale
SARS-CoV-2 is transmitted mainly through close contact and respiratory droplets in the ultrasound room as LUS is not an aerosol-generating procedure. However, it is different in intensive care units where aerosol-generating procedures may be performed, and airborne transmission can occur.Citation85 Adherence to infection prevention and control measures is essential to protect patients and healthcare workers. We will discuss the following three points:
PPE
Cleaning and disinfection of the ultrasound probe
Environmental cleaning and disinfection
PPE
The ultrasound procedure requires close contact with suspected or infected patient. LUS is not an aerosol-producing procedure. Therefore, the following PPE should be worn: surgical mask, eye protection, gown, and gloves.Citation86
The number of persons in the ultrasound room should be limited when examining a patient with suspected or confirmed COVID-19.Citation87
All persons in the room not in close contact with the patient should wear a surgical mask and eye protection.
During environmental cleaning, workers should wear a surgical mask and goggles.
Adherence to the Five Moments for Hand Hygiene using alcohol-based hand soaps is crucial, especially after removing gloves.Citation88
Proper disposal of PPE after removal is a must.
Environmental Surface Cleaning and Disinfection
The use of furniture, which should be made of easily cleaned and disinfected materials, should be limited as much as possible. All unnecessary decorations and accessories should be removed to facilitate the process of cleaning and disinfection.
The ultrasound room should be thoroughly cleaned using detergent and water daily and when needed.
Surfaces should be disinfected, especially frequently touched surfaces, using hospital-approved disinfectants.Citation89
All surfaces should be disinfected between patients, focusing on the examination bed monitors, computer keyboard, computer mice, gel container, door handles, cabinet knobs, light switches, chairs, and counter tops.Citation90
Any used linen should be disposed between patients in a contaminated linen bag. Using disposable linens is advisable if available.Citation91
Ultrasound Probe Disinfection
Cleaning and disinfection for external probes:
Given that LUS is a noncritical procedure, low- or intermediate-level disinfection of the transducer is enough to denature most bacteria, some fungi, and some viruses, such as COVID-19.Citation90
The transducer should be cleaned, followed by disinfection. Ultrasound gels and any debris should be removed using a paper towel, after which a detergent-impregnated wipe approved for use on medical devices should be used. For disinfection, the probe should be wiped using a low- or intermediate-level disinfectant compatible with the ultrasound probe according to the manufacturer’s instructions.Citation92
The entire ultrasound machine should be disinfected, particularly the keyboard, screen, and ultrasound probe cord, using an approved ultrasound machine disinfectant wipe or solution.Citation93
Plastics or disposable covers can be used to decrease contamination of the probe and the entire ultrasound machine, especially the keyboard and probe cord. All disposable covers should be removed. The ultrasound machine and probe should be disinfected between patients.Citation89
Disinfectants Used for Environmental Cleaning
• Ethanol (70–90%).
• Chlorine-based products (eg, hypochlorite) at 0.1% (1000 ppm) for general environmental disinfection or 0.5% (5000 ppm) for large spills of blood and body fluids.
• Hydrogen peroxide (more than 0.5%).
Contact time of a minimum of 1 min is recommended for these disinfectants.Citation94
Disinfectants for Cleaning the Ultrasound Transducer
Chemical “wet” disinfection:
• 2.4–3.2% glutaraldehyde products (eg, Cidex [ASP, Advanced Sterilization Products, Zug, Switzerland], Metricide [Metrex, Orange, CA, USA], and Procide [Metrex, Orange, CA, USA]).
• Non-glutaraldehyde agents (eg, Cidex OPA [o-phthalaldehyde], Cidex PA [hydrogen peroxide], and peroxyacetic acid).
• Approved multi-step disinfectant wipes containing chlorine dioxide, used extensiveily in the United Kingdom and Australia (eg, Tristel Duo [Tristel, Snailwell, Cambridgeshire, UK]).
• 7.5% hydrogen peroxide solution (works by producing destructive hydroxyl free radicals).
• Sodium hypochlorite 0.21% (Antisapril Blu 2% [Monteroni d’Arbia, Italy]).
Limitation
One of the limitations of this consensus, is the absence of special statements for the use of LUS in pregnant women or child/newborns which may need special consensus. However, Yassa et al reported that the use of LUS in pregnant women while awaiting the RT-PCR results may have an important role specially in low-resource setting, In pregnant women LUS was reported to be more predictive in detecting COVID −19 Infection than the use of symptoms only.Citation22
Recommendation
For symptomatic patients with SARS-CoV-2 infection, initial evaluation may include chest X-ray, ultrasound, or CT, if indicated. Point of care LUS training courses are highly recommended for junior physicians in triage or designated hospitals.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
We want to deeply thank and appreciate Ministry of Health and Population COVID-19 board, Egyptian Society of fever (ESF) and UCHID-COVID-19 special interest group: Gamal Esmat; Hossam Hosny; Hanaa Omer; Ehab Kamal; Hatem Elalfy; Ahmed Cordie; Ahmed A. Gomaa; Ahmed S. Abdalmohsen; Akram Abdelbary; Khaled Teima; Ramadan Zaky; Ahmed Mahdy; Ahmed Maher2; Basem Eisa; Dina Attia; Gamal Rabie; Fatema Abdelsalam; Hamdy Ibrahiem; Mahmoud Khalil; Maysaa A. Saeed; Mohamed El Kassas; Mohamed Hamdy; Nemat Abdelmagiud; Usama Hantiur, Rania Samy; Ibrahim F. Mahmoud; Reham Soliman; El-Sayed Emam; Sherief Musa; Yasser Mahrous; Gamal Shiha; Gehan Elassal.
With affiliations from these organizations: Endemic Medicine and Hepatology Department, Faculty of Medicine, Cairo University, Cairo, Egypt; Division of Tropical Medicine Medical Research, National Research Centre, Giza, Egypt; Department of endemic medicine, Mansoura university; Department of Tropical Medicine, Fayoum University, Egypt; Critical Care Medicine, Cairo University, Cairo, Egypt; Ministry of Health and Population, Egypt; Department of Zoonotic diseases, National Research Center, Egypt; Department of Tropical Medicine, Bani Sweif University, Egypt; Tropical medicine and infectious Diseases department, Faculty of Medicine, Zagazig University, Cairo, Egypt; Department of anesthesiology and intensive care, Al-Azhar university, Egypt; Hepatology and Gastroenterology Unit, Internal Medicine Department, Faculty of Medicine, Mansoura University, Egypt; Chest diseases Department, Faculty of Medicine, Cairo University, Cairo, Egypt.
Additional information
Funding
References
- Alhazzani W, Møller MH, Arabi YM, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Med. 2020;46(5):854–887. doi:10.1007/s00134-020-06022-5
- Soldati G, Smargiassi A, Inchingolo R, et al. Is there a role for lung ultrasound during the COVID-19 pandemic? J Ultrasound Med. 2020;39(7):1459–1462. doi:10.1002/jum.15284
- Wan Y, Shang J, Graham R, Baric RS, Li F, Gallagher T. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol. 2020;94(7):e00127–20. doi:10.1128/JVI.00127-20
- Convissar DL, Gibson LE, Berra L, Bittner EA, Chang MG. Application of lung ultrasound during the COVID-19 pandemic: a narrative review. Anesth Analg. 2020;131(2):345–350. doi:10.1213/ANE.0000000000004929
- Yasukawa K, Minami T. Point-of-care lung ultrasound findings in patients with COVID-19 Pneumonia. Am J Trop Med Hyg. 2020;102(6):1198–1202. doi:10.4269/ajtmh.20-0280
- Buonsenso D, Moro F, Inchingolo R, et al. Effectiveness of rapid lung ultrasound training program for gynecologists and obstetricians managing pregnant women with suspected COVID‐19. Ultrasound Obstet Gynecol. 2020;56(1):110–111. doi:10.1002/uog.22066
- Alrifai A, El-Raey FM, Yousef AM, Zaky S. Ultrasound in suspected pneumonic COVID-19: our experience. Int J Med Art. 2020;2(4):682–689. doi:10.21608/IJMA.2020.43493.1176
- Zaky S, Metwally MA, El Badry M, et al. Utility of lung ultrasound in Decision-making to prioritize hospital admission for COVID-19 patients: a developing country perspective. Curr Med Imag. 2021;17(12):1473–1480. doi:10.2174/1573405617666210506164243
- Qiu Y, Chen X, Shi W. Impacts of social and economic factors on the transmission of coronavirus disease 2019 (COVID-19) in China. J Popul Econ. 2020;33:1127–1172. doi:10.1007/s00148-020-00778-2
- Chowdhury R, Heng K, Shawon MS, et al. Dynamic interventions to control COVID-19 pandemic: a multivariate prediction modelling study comparing 16 worldwide countries. Eur J Epidemiol. 2020;35(5):389–399. doi:10.1007/s10654-020-00649-w
- Dahab M, Van Zandvoort K, Flasche S, et al.COVID-19 control in low-income settings and displaced populations: what can realistically be done? Confl Health. 2020;14(1):1–6. doi:10.1186/s13031-020-00296-8
- Chen D, Tang F, Lu S, Song Q. Toward a clinically based classification of disease severity for paediatric COVID-19–Authors’ reply. Lancet Infect Dis. 2021;21(1):22–23. doi:10.1016/S1473-3099(20)30397-2
- Lipsky BA, Berendt AR, Cornia PB, et al. 2012 infectious diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2012;54(12):e132–73. doi:10.1093/cid/cis346
- Ponikowski P, Anker SD, AlHabib KF, et al. Heart failure: preventing disease and death worldwide. ESC Heart Failure. 2014;1(1):4–25. doi:10.1002/ehf2.12005
- Cobre AD, Böger B, Fachi MM, et al. Risk factors associated with delay in diagnosis and mortality in patients with COVID-19 in the city of Rio de Janeiro, Brazil. Cien Saude Colet. 2020;25:4131–4140. doi:10.1590/1413-812320202510.2.26882020
- Honein MA, Christie A, Rose DA, et al. Summary of guidance for public health strategies to address high levels of community transmission of SARS-CoV-2 and related deaths, December 2020. Morb Mortal Wkly Rep. 2020;69(49):1860. doi:10.15585/mmwr.mm6949e2
- Buonsenso D, De Rose C. Implementation of lung ultrasound in low-to-middle income countries: a new challenge global health? Authorea. 2021. doi:10.22541/au.161449326.65024375/v1
- COVID-19 Treatment Guidelines Panel. Coronavirus disease 2019 (COVID-19) treatment guidelines. National Institutes of Health. Available from: https://www.covid19treatmentguidelines.nih.gov/. Accessed May 21, 2021.
- Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi:10.1016/S1473-3099(20)30086-4
- Ishfaq A, Yousaf Farooq SM, Goraya A, et al. Role of high resolution computed tomography chest in the diagnosis and evaluation of COVID −19 patients -A systematic review and meta-analysis. Eur J Radiol Open. 2021;8:100350. doi:10.1016/j.ejro.2021.100350
- Larici AR, Cicchetti G, Larici AR, et al. Multimodality imaging of COVID-19 pneumonia: from diagnosis to follow-up. A comprehensive review. Eur J Radiol. 2020;131:109217. PMID: 32861174; PMCID: PMC7430292. doi:10.1016/j.ejrad.2020.109217
- Yassa M, Birol P, Mutlu AM, Tekin AB, Sandal K, Tug N. Lung ultrasound can influence the clinical treatment of pregnant women with COVID-19. J Ultrasound Med. 2021;40(1):191–203. PMID: 32478445; PMCID: PMC7300952. doi:10.1002/jum.15367
- World Health Organization. WHO COVID-19 case definition. WHO reference number: WHO/2019-nCoV/Surveillance_Case_Definition/2020.1. Available from: https://apps.who.int/iris/handle/10665/333912?show=ful. Accessed April 2, 2022.
- Bernheim A, Mei X, Huang M, et al. Chest CT findings in Coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295(3):200463. PMID: 32077789; PMCID: PMC7233369. doi:10.1148/radiol.2020200463
- Song F, Shi N, Shan F, et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;297(3):E346. PMID: 33196374. doi:10.1148/radiol.2020209021
- Fang Y, Zhang H, Xie J, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020;296(2):E115–E117. doi:10.1148/radiol.2020200432
- Pan Y, Guan H, Zhou S. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020;30(6):3306–3309.
- Qian L, Yu J, Shi H. Severe acute respiratory disease in a huanan seafood market worker: images of an early casualty. Radiol Cardiothorac Imag. 2020;2(1):e200033. doi:10.1148/ryct.2020200033
- Shi H, Han X, Zheng C. Evolution of CT manifestations in a patient recovered from 2019 novel coronavirus (2019-nCoV) pneumonia in Wuhan, China. Radiology. 2020;295(1):20. doi:10.1148/radio
- Lei J, Li J, Li X, Qi X. CT imaging of the 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295(1):18. doi:10.1148/radiol.2020200236
- Xu X, Yu C, Zhang L, Luo L, Liu J. Imaging features of 2019 novel coronavirus pneumonia. Eur J Nucl Med Mol Imag. 2020;47(5):1022–1023. doi:10.1007/s00259-020-04720-2
- Kong W, Agarwal PP. Chest imaging appearance of COVID-19 infection. Radiol Cardioth Imag. 2020;2(1):e200028. doi:10.1148/ryct.2020200028
- Jin YH, Cai L, Cheng ZS, et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res. 2020;7(1):4. doi:10.1186/s40779-020-0233-6
- Pan F, Ye T, Sun P, et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020;295:200370.
- World bank. Data of Egypt, Arab Rep., lower middle income. Available from: https://data.worldbank.org/?locations=EG-XN. Accessed May 1, 2020.
- Dudea SM. Ultrasonography and SARS-CoV 2 infection: a review of what we know and do not yet know. Med Ultrason. 2020;22(2):129–132. doi:10.11152/mu-2612
- Koegelenberg CF, Von Groote-bidlingmaier F, Bolliger CT. Transthoracic ultrasonography for the respiratory physician. Respiration. 2012;84(4):337–350. doi:10.1159/000339997
- Miller A. Practical approach to lung ultrasound. BJA Educ. 2016;16:39–45. doi:10.1093/bjaceaccp/mkv012
- Lichtenstein DA. The A-profile (normal lung surface): 2) lung sliding. Lung Ultrasound in the Critically Ill. Springer, Cham. 2016. doi:10.1007/978-3-319-15371-1_10
- Bouhemad B, Zhang M, Lu Q, Rouby JJ. Clinical review: bedside lung ultrasound in critical care practice. Crit Care. 2007;11:205. doi:10.1186/cc5668
- Aldrich JE. Basic physics of ultrasound imaging. Crit Care Med. 2007;35(Suppl):S131–7. doi:10.1097/01.CCM.0000260624.99430.22
- Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest. 2008;134:117–125. doi:10.1378/chest.07-2800
- Lichtenstein DA, Mezière GA, Lagoueyte JF, Biderman P, Goldstein I, Gepner A. A-lines and B-lines: lung ultrasound as a bedside tool for predicting pulmonary artery occlusion pressure in the critically ill. Chest. 2009;136:1014–1020. doi:10.1378/chest.09-0001
- Pons S, Fodil S, Azoulay E, Zafrani L. The vascular endothelium: the cornerstone of organ dysfunction in severe SARS-CoV-2 infection. Crit Care. 2020;24(1):353. doi:10.1186/s13054-020-03062-7
- Zanforlin A, Tursi F, Marchetti G, et al. Clinical use and barriers of thoracic ultrasound: a survey of Italian pulmonologists. Eur Respirat J. 2018. doi:10.1183/13993003.congress-2018.PA378
- Volpicelli G, Elbarbary M, Blaivas M, et al. International liaison committee on lung ultrasound (ILC-LUS) for International consensus conference on lung ultrasound (ICC-LUS). International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38:577–591. doi:10.1007/s00134-012-2513-4
- Via G, Storti E, Gulati G, Neri L, Mojoli F, Braschi A. Lung ultrasound in the ICU: from diagnostic instrument to respiratory monitoring tool. Minerva Anestesiol. 2012;78:1282–1296.
- Mathis G. Thoraxsonography–Part 1: chest wall and pleura. Praxis. 2004;93::615–621. doi:10.1024/0369-8394.93.15.615
- Copetti R, Soldati G, Copetti P. Chest sonography: a useful tool to differentiate acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc Ultrasound. 2008;6:16. doi:10.1186/1476-7120-6-16
- Reissig A, Kroegel C. Transthoracic sonography of diffuse parenchymal lung disease: the role of comet tail artifacts. J Ultrasound Med. 2003;22:173–180. doi:10.7863/jum.2003.22.2.173
- Sultan LR, Sehgal CM. a review of early experience in lung ultrasound in the diagnosis and management of covid-19. Ultrasound Med Biol. 2020;46(9):2530 2545. doi:10.1016/j.ultrasmedbio.2020.05.012
- Peng QY, Wang XT, Zhang LN, et al. Findings of lung ultrasonography of novel Corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med. 2020;46:849–850. doi:10.1007/s00134-020-05996-6
- Thomas A, Haljan G, Mitra A. Lung ultrasound findings in a 64-year-old woman with COVID-19. Can Med Assoc J. 2020;192:E399. doi:10.1503/cmaj.200414
- Lomoro P, Verde F, Zerboni F, et al. COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and CT: single-center study and comprehensive radiologic literature review. Eur J Radiol Open. 2020;7:7100231.
- Yi H, Wang S, Liu Y, et al. A preliminary study on the ultrasonic manifestations of peripulmonary lesions of non-critical novel coronavirus pneumonia (COVID-19); February 26, 2020. doi: 10.2139/ssrn.3544750.
- Buonsenso D, Raffaelli F, Tamburrini E, et al. Clinical role of lung ultrasound for the diagnosis and monitoring of COVID-19 pneumonia in pregnant women. Ultrasound Obstet Gynecol. 2020;56(1):106–109. doi:10.1002/uog.22055
- Vetrugno L, Bove T, Orso D, et al. Our Italian experience using lung ultrasound for identification, grading and serial follow-up of severity of lung involvement for management of patients with COVID-19. Echocardiography. 2020;37(4):625–627. doi:10.1111/echo.14664
- Kalafat E, Yaprak E, Cinar G, et al. Lung ultrasound and computed tomographic findings in pregnant woman with COVID-19. Ultrasound Obstet Gynecol. 2020;55(6):835–837. doi:10.1002/uog.22034
- Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004;100:9–15. doi:10.1097/00000542-200401000-00006
- Buonsenso D, Piano A, Raffaelli F, Bonadia N, de Gaetano DK, Franceschi F. Point-of-care lung ultrasound findings in novel coronavirus disease-19 pnemoniae: a case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020;24:2776–2780. doi:10.26355/eurrev_202003_20549
- Ji L, Cao C, Gao Y, et al. Prognostic value of bedside lung ultrasound score in patients with COVID-19. Crit Care. 2020;24:700. doi:10.1186/s13054-020-03416-1
- Shumilov E, Hosseini A, Petzold G, et al. Comparison of chest ultrasound and standard X-ray imaging in COVID-19 patients. Ultrasound Int Open. 2020;6(2):E36–E40. doi:10.1055/a-1217-1603
- Ng M-Y, Lee EYP, Yang J, et al. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiology. 2020;2:e200034. doi:10.1148/ryct.2020200034
- Chung M, Bernheim A, Mei X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology. 2020;295:202–207. doi:10.1148/radiol.2020200230
- Egyptian ministry of health official report; 2020. Available from: www.mohp.gov. Accessed April 2, 2022.
- Tan G, Lian X, Zhu Z, et al. Use of lung ultrasound to differentiate coronavirus disease 2019 (COVID-19) pneumonia from community-acquired pneumonia. Ultrasound Med Biol. 2020;46(10):2651–2658. PMID: 32622684; PMCID: PMC7274602. doi:10.1016/j.ultrasmedbio.2020.05.006.
- Deng Q, Zhang Y, Wang H, et al. Semiquantitative lung ultrasound scores in the evaluation and follow-up of critically ill patients with COVID-19: a single-center study. Acad Radiol. 2020;27(10):1363–1372. doi:10.1016/j.acra.2020.07.002
- Soummer A, Perbet S, Brisson H, et al. Ultrasound assessment of lung aeration loss during a successful weaning trial predicts postextubation distress. Crit Care Med. 2012;40(7):2064–2072. doi:10.1097/CCM.0b013e31824e68ae
- Lichter Y, Topilsky Y, Taieb P, et al. Lung ultrasound predicts clinical course and outcomes in COVID-19 patients. Intensive Care Med. 2020;46(10):1873–1883. doi:10.1007/s00134-020-06212-1
- Brahier T, Meuwly J-Y, Pantet O, et al. Lung ultrasonography for risk stratification in patients with COVID-19: a prospective observational cohort study. Clin Infect Dis. 2020. doi:10.1093/cid/ciaa1408
- Caltabeloti F, Monsel A, Arbelot C, et al. Auler Jr JOC and Rouby JJ. Early fluid loading in acute respiratory distress syndrome with septic shock deteriorates lung aeration without impairing arterial oxygenation: a lung ultrasound observational study. Crit Care. 2014;18(3):R91. doi:10.1186/cc13859
- De Alencar JCG, Marchini JFM, Marino LO, et al. Lung ultrasound score predicts outcomes in COVID-19 patients admitted to the emergency department. Ann Intensive Care. 2021;11:6. doi:10.1186/s13613-020-00799-w
- Bouhemad B, Brisson H, Le-guen M, Arbelot C, Lu Q, Rouby JJ. Bedside ultrasound assessment of positive end-expiratory pressure-induced lung recruitment. Am J RespirCrit Care Med. 2011;183:341–347. doi:10.1164/rccm.201003-0369OC
- Volpicelli G, Lamorte A, Villén T. What’s new in lung ultrasound during the COVID-19 pandemic. Intensive Care Med. 2020;46(7):1445–1448. doi:10.1007/s00134-020-06048-9
- Manivel V, Lesnewski A, Shamim S, Carbonatto G, Govindan T. CLUE: COVID-19 lung ultrasound in emergency department. Emerg Med Australas. 2020;32:694–696. doi:10.1111/1742-6723.13546
- Mafort TT, Lopes AJ, Costa CH, et al. Changes in lung ultrasound of symptomatic healthcare professionals with COVID -19 pneumonia and their association with clinical findings. J Clin Ultrasound. 2020;48(9):515–521. doi:10.1002/jcu.22905
- Volpicelli G, Gargani L, Perlini S, et al. Lung ultrasound for the early diagnosis of COVID-19 pneumonia: an international multicenter study. Intensive Care Med. 2021;47(4):444–454. doi:10.1007/s00134-021-06373-7
- Kruser JM, Schmidt GA, Kory PD. COUNTERPOINT: should the use of diagnostic point-of-care ultrasound in patient care require hospital privileging/credentialing? No. Chest. 2020;157(3):498–500. doi:10.1016/j.chest.2019.10.037
- Buonsenso D, Piano A, Raffaelli F, Bonadia N, Donati KDG, Franceschi F. novel coronavirus disease-19 pnemoniae: a case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020;24:2776–2780.
- Lin H, Zhang B, Kou H, et al. Application value of lung ultrasound in asymptomatic patients with confirmed COVID-19. Adv ultrasound diagn ther. 2020;4(2):67–72. doi:10.37015/AUDT.2020.200025
- Sartori S, Tombesi P. Emerging roles for transthoracic ultrasonography in pulmonary diseases. World J Radiol. 2010;2(6):203. doi:10.4329/wjr.v2.i6.203
- Boero E, Schreiber A, Rovida S, Vetrugno L, Blaivas M. The role of lung ultrasonography in COVID‐19 disease management. J Am Coll Emerg Physicians Open. 2020;1(6):1357–1363. doi:10.1002/emp2.12194
- Di Pan DO, Salonia J, de Lara FV, Mathew J. Efficacy of a two-week ultrasound elective in knowledge acquisition and retention of thoracic ultrasonography among internal medicine residents. Chest. 2019;156. doi:10.1016/j.chest.2019.08.1453
- Jonson B. Training for Lung ultrasound score measurement in critically Ill patients. Am J Respir Crit Care Med. 2018;198(3):396–398. doi:10.1164/rccm.201801-0093LE
- World Health Organization. Modes of transmission of virus causing COVID-19: implications for IPC precaution: scientific brief. Geneva; 2020. Available from: https://www.who.int/publications-detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations. Accessed April 4, 2022.
- World Health Organization. Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages: interim guidance. World Health Organization; April 6, 2020. Available from: https://apps.who.int/iris/handle/10665/331695. Accessed April 4, 2022.
- World Health Organization. 2020: infection prevention and control during health care when COVID-19 is suspected interim guidance; March 19, 2020.
- Centers for disease control and Prevention. Hand hygiene recommendations. guidance for healthcare providers about hand hygiene and COVID-19; 2019. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/hand-hygiene.html. Accessed April 4, 2022.
- Centers for disease control and Prevention. Recommendations for disinfection and sterilization in healthcare facilities: guideline for disinfection and sterilization in healthcare facilities (2008); 2008. Available from: https://www.cdc.gov/infectioncontrol/guidelines/disinfection/recommendations.html. Accessed April 4, 2022.
- Abramowicz JS, Akiyama I, Evans D, et al.; World Federation for Ultrasound in Medicine and Biology Safety Committee. World federation for ultrasound in medicine and biology position statement: how to perform a safe ultrasound examination and clean equipment in the context of COVID-19. Ultrasound Med Biol. 2020;46(7):1821–1826. doi:10.1016/j.ultrasmedbio.2020.03.033
- Centers for disease control and Prevention. Background G. laundry and bedding. guidelines for environmental infection control in health-care facilities (2003); 2003. Available from: https://www.cdc.gov/infectioncontrol/guidelines/environmental/background/laundry.html. Accessed April 4, 2022.
- Basseal JM, Westerway SC, McAuley T. COVID‐19: infection prevention and control guidance for all ultrasound practitioners. Australas J Ultrasound Med. 2020;23(2):90–95. doi:10.1002/ajum.12210
- ACEP. Guideline on COVID-19: ultrasound machine and transducer cleaning approved march 31, 2020. Available from: https://www.acep.org/globalassets/new-pdfs/guideline-on-covid-19–ultrasound-machine-and-transducer-cleaning_policy_033120.pdf. Accessed April 4, 2022.
- World Health Organization. Cleaning and disinfection of environmental surfaces in the context of COVID-19: interim guidance 16 May 2020 WHO reference number: WHO/2019-nCoV/disinfection/2020.1; 2020.
- Ochagavia A, Baigorri F, Mesquida J, et al. Hemodynamic monitoring in the critically patient. Recommendations of the Cardiological Intensive Care and CPR working group of the Spanish society of intensive care and coronary units. Medicina Intensiva. 2014;38:154–169. doi:10.1016/j.medin.2013.10.006
- Buonsenso D, Pata D, Chiaretti A. COVID-19 outbreak: less stethoscope, more ultrasound. Lancet Respir Med. 2020;8(5):e27. doi:10.1016/S2213-2600(20)30120-X
