Abstract
Purpose
To investigate the phenotypic and genomic characteristics of the multi-drug resistant and hypervirulent Klebsiella pneumoniae strain recovered from bacteremia.
Methods
Antimicrobial susceptibility testing (AST) was performed by the microdilution method. Antimicrobial resistance genes, virulence-associated genes, multilocus sequence typing (MLST), and plasmid replicon were characterized by next-generation sequencing (NGS) and nanopore sequencing. S1 nuclease-pulsed field gel electrophoresis (S1-PFGE) and Southern blotting were performed to characterize the plasmid profile.
Results
The hypervirulent colistin- and carbapenem-resistant K. pneumoniae strain DY2009 was identified as ST5571, co-carrying mcr-1, blaNDM-1, and blaOXA-10. In silico analysis found that it was K2 serotype. AST results revealed that DY2009 was resistant to carbapenems, cephalosporins, ciprofloxacin, chloramphenicol, and colistin but remained susceptible to aztreonam, gentamicin, amikacin, and tigecycline. Through the whole-genome analysis, a variety of virulence determinants were identified, including rmpA. Plasmid analysis confirmed that the mcr-1 and blaNDM-1 gene harbored a ~33 kb IncX4 plasmid and a ~44 kb IncX3 plasmid. In contrast, blaOXA-10 was encoded by chromosome.
Conclusion
To the best of our knowledge, we first report the clinical hypervirulent K. pneumoniae isolate co-producing MCR-1, NDM-1, and OXA-10 causing bacteremia. We found that mcr-1 and blaNDM-1 genes were located on two self-conjugative epidemic plasmids, contributing to the widespread MCR-1 and NDM-1 in China. The results of this work improve our understanding of the genetic background of colistin- and carbapenem-resistant K. pneumoniae isolate from bacteremia and the resistance mechanisms. Our findings highlight the urgent need for infection control of such strain to prevent it from becoming an extensive-drug resistant clone.
Carbapenem-resistant Klebsiella pneumoniae (CRKP) has been recognized as one of the most worrying threats to human health globally.Citation1–5 Due to the limited therapeutic options, infections caused by CRKP result in high mortality.Citation6 Polymyxins, including colistin, are a significant “last-line” treatment for infections caused by CRKP.Citation6 However, since the first plasmid-mediated colistin resistance gene mcr-1 was identified in China, many mcr genes have been detected in Enterobacteriaceae species.Citation7–9 The emergence of mcr genes in CRKP represents a real challenge to clinical treatments.
A low prevalence of mcr-1 in K. pneumoniae was observed,Citation10 although several mcr genes and their variants have been detected in K. pneumoniae.Citation11,Citation12 In this work, we reported a bloodstream infection caused by a colistin-resistant CRKP strain. Whole-genome sequencing (WGS) and microbiological analysis revealed the emergence of colistin-resistant CRKP clinical strain co-producing NDM-1, MCR-1, and OXA-1.
K. pneumoniae strain DY2009 was recovered from an 85-years old female patient with bacteremia in January 2020 from Dongyang, China. The bacterial identification was conducted using Matrix-Assisted Laser Desorption/Ionization Time-of-Flight mass-spectrometer (MALDI-TOF-MS) (Bruker Daltonics, Germany).Citation13 Antimicrobial susceptibility testing was performed by the broth microdilution method. The results were interpreted according to the Clinical and Laboratory Standards Institute standards,Citation14 except for tigecycline and colistin, according to the European Committee on Antimicrobial Susceptibility Testing (EUCAST) guidelines (https://www.eucast.org/). K. pneumoniae strain DY2009 was resistant to imipenem (MIC = 4 mg/L), meropenem (MIC = 4 mg/L), cefotaxime (MIC = 128 mg/L), ceftazidime (MIC ≥128 mg/L), cefpirome (MIC = 32 mg/L), piperacillin/tazobactam (MIC ≥128 mg/L), ciprofloxacin (MIC = 8 mg/L), chloramphenicol (MIC ≥128 mg/L), and colistin (MIC = 32 mg/L). However, this strain was susceptible to aztreonam (MIC = 0.25 mg/L), gentamicin (MIC = 2 mg/L), amikacin (MIC = 2 mg/L), and tigecycline (MIC = 1 mg/L) (). The patient was treated with piperacillin/tazobactam empirically and changed to amikacin after obtaining susceptibility results. The patient recovered gradually and discharged from the hospital.
Table 1 Antimicrobial Susceptibilities of Strain Klebsiella pneumoniae DY2009
Genomic DNA of K. pneumoniae DY2009 was extracted using the Gentra Puregene Yeast/Bact. Kit (Qiagen, Germany) according to the manufacturer’s instructions. The sequencing library was prepared by using Illumina Nextera XT kit and sequenced using the Illumina HiSeq X 10-PE150 platform (Illumina, San Diego, CA, USA). A-tailed fragments were ligated with paired-end adaptors and PCR-amplified with a 500-bp insert. A mate-pair library with an insert size of 5 kb was used for library construction, at the Beijing Novogene Bioinformatics Technology Co., Ltd. PCR adapter reads and low-quality reads from the paired-end and mate-pair library were filtered during a quality control step using the Novogene pipeline. To investigate the genetic environment of plasmids carrying blaNDM-1 and mcr-1 genes, DY2009 was further analyzed by Nanopore sequencing (Oxford, UK). Unicycler was used for hybrid assembling K. pneumoniae DY2009 genome from Illumina short reads and Nanopore long reads.Citation15 Three modes (conservative, normal and bold) of Unicycler were run to generate the best-assembled results. Antimicrobial resistance genes (ARGs) were identified using the ResFinder 3.1 database.Citation16 Plasmid Finder 1.3 was used to determine the incompatibility type of the plasmids.Citation17 We identified the virulence loci with the assembled genome sequences using the BIGSdb Klebsiella genome database (http://bigsdb.pasteur.fr/klebsiella/).
By searching against the K. pneumoniae locus/sequence definitions database (https://cge.cbs.dtu.dk/services/MLST/), we found that K. pneumoniae DY2009 was classified as ST5571. An IncX4 plasmid-mediated colistin resistance gene, mcr-1, was identified using ResFinder 3.1 (). A total of 19 ARGs was found in DY2009 (). Of note, one class D β-lactamase encoding gene, blaOXA-10, was found in the chromosome of strain DY2009. In contrast, NDM-1 was encoded by an IncX3 plasmid (). PCR detection and Sanger sequencing confirmed that K. pneumoniae DY2009 was positive for blaNDM-1 and mcr-1. OXA-10 type was known to have narrow spectrum β-lactamase activity and shown to be weak carbapenemases.Citation18 These results is consistent with the antimicrobial profile observed in K. pneumoniae DY2009. Additionally, screening of virulence factors found that this isolate harbored several virulence determinants. These virulence factors include the regulator of the mucoid phenotype (rmpA), ABC transporter (iroC), yersiniabactin polyketide synthase (irp1 and irp2), type VI secretion protein (icmF), enterobactin synthase subunit F (entF), acriflavine resistance protein B (acrB), ferric aerobactin receptor (iutA), aerobactin siderophore biosynthesis protein (iucC), and aerobactin synthetase (iucA) encoded genes. Furthermore, in silico analysis indicates that DY2009 is capsule type K2. It is well known that a significant virulence factor for K. pneumoniae is the capsule, and capsule type K2 isolates produce a capsule that causes hypermucoidy. These results revealed that DY2009 is likely a hypervirulent strain.
Table 2 Antimicrobial Resistance Genes Encoded by Klebsiella pneumoniae DY2009
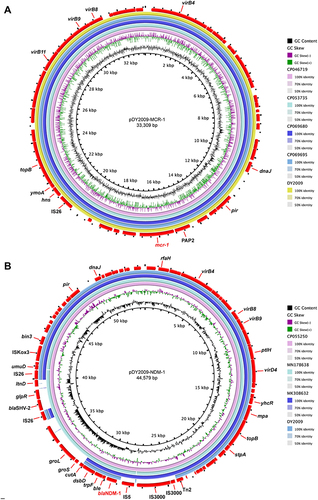
Figure 1 Alignment of mcr-1/blaNDM-1-harboring plasmids detected in this study. (A) Genomic map of the mcr-1-carrying Inx4 pDY2009-MCR-1 plasmid with four closely related plasmids (CP046719, CP053735, CP069680, CP069695). (B) Circular genome alignment of pDY2009-NDM-1 with three blaNDM-bearing IncX3 plasmids (CP055250, MN178638, MK308632). Arrows portrayed genes. The circular map was generated with the BLAST Ring Image Generator.
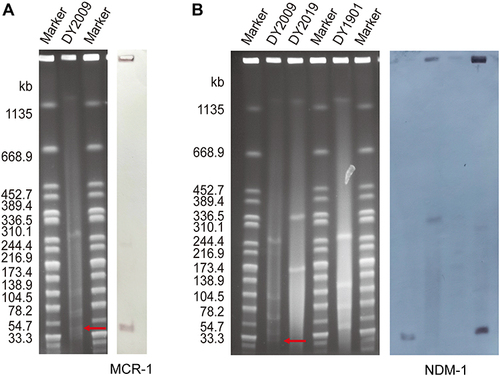
S1 Nuclease-Pulsed Field Gel Electrophoresis (S1-PFGE) and Southern blotting was conducted to determine the location of mcr-1 and blaNDM-1 with a digoxigenin-labeled mcr-1 and blaNDM-1 probe.Citation13 Transconjugation assay was performed by mating E. coli J53 as the recipient strain. Transconjugants were selected on agar (OXOID, Hampshire, UK) medium at a 200 mg/L sodium azide concentration with two mg/L colistin/meropenem. Finally, MALDI-TOF-MS was used to identify transconjugants, and PCR verified the target gene. Nanopore sequencing revealed that DY2009 carried seven plasmids (Table S1). S1-PFGE and Southern blotting confirmed the existence of 33.3 kbp IncX4 pDY2009-MCR-1 and 44.6 kbp IncX3 pDY2009-NDM-1 (). The transconjugants carrying the 33.3 kbp IncX4 pDY2009-MCR-1 plasmid showed a MIC of colistin of 4 mg/L and 44.6 kbp IncX3 pDY2009-NDM-1 plasmid showed a MIC of imipenem of 4 mg/L. These data confirmed that IncX4 pDY2009-MCR-1 plasmid and 44.6 kbp IncX3 pDY2009-NDM-1 are both conjugative and responsible for colistin resistance and carbapenem resistance, respectively. Importantly, eight mutations were found in phoP gene and three mutations were found in phoQ gene, which result in increased colistin resistance resistance in DY2009.
Figure 2 Plasmid analysis of the ST5571 colistin-resistant CRKP strain DY2009 via S1-PFGE and Southern blotting using mcr-1 and blaNDM-1 probes. (A) Analysis of pDY2009-MCR-1. (B) Analysis of pDY2009-NDM-1. Due to the similar plasmid size of pDY2009-MCR-1 and pDY2009-NDM-1, NDM-1-producing clinical isolates DY2019 and DY1901 recovered from the same hospital were used as control. The red arrows indicate the locations of the resistance plasmid.
By Blastn against NCBI database, we found that pDY2009-MCR-1 shared the highest similarity (99.99% identity with 99% coverage) with pT16R-3 (CP046719), pCP55-IncX4 (CP053735), pMUB-MIN6-MCR (CP069695), and pMUB-MIN10-MCR (CP069680). Of note, plasmids pT16R-3 and pCP55-IncX4 were identified from animal-originated Escherichia coli isolates in China, in contrast, pMUB-MIN6-MCR and pMUB-MIN10-MCR were identified from clinical E. coli isolates in Poland.Citation19 Lo and colleagues proved that 33 kb IncX4 plasmid is highly transmissible, showing ~100-fold higher transfer frequencies relative to epidemic IncFII plasmid.Citation20 In vitro assay confirmed the fitness advantage of mcr-1-harboring IncX4 plasmids.Citation21 These results suggest that self-transmissible IncX4-type plasmids may contribute to the global dissemination of the mcr-1 gene.Citation22,Citation23 Our study further highlights that an effective prevention strategy should be taken to restrain the further dissemination of mcr-1-bearing IncX4 plasmids.
Blastn search further revealed that pDY2009-NDM-1 shared the highest similarity (100% identity with 91% coverage) with pZY-NDM1 (CP055250), pNDM1_SCW13 (MN178638), and pNDM5-LDR (MK308632). A conserved gene-environment around blaNDM-1 (IS5- blaNDM-1-trpF-dsbC-cutA1-groEL) was observed in pDY2009-NDM-1 (). Previous studies indicated that most of the IncX3 plasmids were present in E. coli, followed by K. pneumoniae.Citation24 Of note, blaNDM has been rapidly spreading in China mainly due to the national dissemination of blaNDM-bearing IncX3 plasmid.Citation25,Citation26 Our study highlights that IncX3 plasmid may accelerate the occurrence of the carbapenem-resistant K. pneumoniae isolate in China.
In general, we isolated a hypervirulent colistin-resistant ST5571 CRKP strain DY2009 from a blood sample in China. The WGS and microbiological analysis were performed to elucidate its antimicrobial resistance mechanisms, which found that this strain contained 19 ARGs associated with its resistance phenotype. This is the first report in China of a clinical bacterial isolate co-producing MCR-1, NDM-1, and OXA-10, highlighting the necessity of active surveillance efforts for colistin- and carbapenem-resistant organisms in clinical practice settings. Thus, our findings improve the understanding of the genetic context of colistin- and carbapenem-resistant K. pneumoniae isolate from bacteremia and the resistance mechanisms.
Nucleotide Sequence Accession Numbers
The whole-genome sequencing of K. pneumoniae strain DY2009 has been deposited into DDBJ/EMBL/GenBank under the Biosample accession number SAMN25509743.
Ethics Approval and Consent to Participate
This study was conducted following the Declaration of Helsinki and obtained approval from the Medical Ethics Committee at The First Hospital of Jiaxing. The patient provided written informed consent to allow the case details to be published.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No. 82072314) and Zhejiang Medical and Health Science and Technology Project (No. 2020KY950 and No. 2022KY373).
References
- Zhang J, Zhou K, Zheng B, et al. High Prevalence of ESBL-Producing Klebsiella pneumoniae Causing Community-Onset Infections in China. Front Microbiol. 2016;7:1830.
- Zheng B, Zhang J, Ji J, et al. Emergence of Raoultella ornithinolytica coproducing IMP-4 and KPC-2 carbapenemases in China. Antimicrob Agents Chemother. 2015;59(11):7086–7089.
- Zheng B, Li A, Jiang X, et al. Genome sequencing and genomic characterization of a tigecycline-resistant Klebsiella pneumoniae strain isolated from the bile samples of a cholangiocarcinoma patient. Gut Pathog. 2014;6(1):40.
- El-Badawy MF, El-Far SW, Althobaiti SS, Abou-Elazm FI, Shohayeb MM. The First Egyptian Report Showing the Co-Existence of bla NDM-25, bla OXA-23, bla OXA-181, and bla GES-1 Among Carbapenem-Resistant K. pneumoniae Clinical Isolates Genotyped by BOX-PCR. Infect Drug Resist. 2020;13:1237–1250.
- Gondal AJ, Saleem S, Jahan S, Choudhry N, Yasmin N. Novel Carbapenem-Resistant Klebsiella pneumoniae ST147 Coharboring bla NDM-1, bla OXA-48 and Extended-Spectrum beta-Lactamases from Pakistan. Infect Drug Resist. 2020;13:2105–2115.
- Rojas LJ, Salim M, Cober E, et al. Colistin Resistance in Carbapenem-Resistant Klebsiella pneumoniae: laboratory Detection and Impact on Mortality. Clin Infect Dis. 2017;64(6):711–718.
- Zheng B, Yu X, Xu H, et al. Complete genome sequencing and genomic characterization of two Escherichia coli strains co-producing MCR-1 and NDM-1 from bloodstream infection. Sci Rep. 2017;7(1):17885.
- Luo Q, Wan F, Yu X, et al. MDR Salmonella enterica serovar Typhimurium ST34 carrying mcr-1 isolated from cases of bloodstream and intestinal infection in children in China. J Antimicrob Chemother. 2020;75(1):92–95.
- Hu S, Lv Z, Wang Y, Shen J, Ke Y. Rapid detection of human origin colistin-resistance genes mcr-1, mcr-3, mcr-8, mcr-10 in clinical fecal samples. Arch Microbiol. 2021;203(7):4405–4417.
- Zheng B, Xu H, Yu X, et al. Low prevalence of MCR-1-producing Klebsiella pneumoniae in bloodstream infections in China. Clin Microbiol Infect. 2018;24(2):205–206.
- Wang X, Li Q, Kang J, et al. Co-Production of NDM-1, CTX-M-9 Family and mcr-1 in a Klebsiella pneumoniae ST4564 Strain in China. Infect Drug Resist. 2021;14:449–457.
- Sun S, Gao H, Liu Y, et al. Co-existence of a novel plasmid-mediated efflux pump with colistin resistance gene mcr in one plasmid confers transferable multidrug resistance in Klebsiella pneumoniae. Emerg Microbes Infect. 2020;9(1):1102–1113.
- Xu H, Wang X, Yu X, et al. First detection and genomics analysis of KPC-2-producing Citrobacter isolates from river sediments. Environ Pollut. 2018;235:931–937.
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing. 27th ed. PA, USA: Clinical and Laboratory Standards Institute; 2017.
- Wick RR, Judd LM, Gorrie CL, Holt KE. Unicycler: resolving bacterial genome assemblies from short and long sequencing reads. PLoS Comput Biol. 2017;13(6):e1005595.
- Zankari E, Hasman H, Cosentino S, et al. Identification of acquired antimicrobial resistance genes. J Antimicrob Chemother. 2012;67(11):2640–2644.
- Carattoli A, Zankari E, Garcia-Fernandez A, et al. In silico detection and typing of plasmids using PlasmidFinder and plasmid multilocus sequence typing. Antimicrob Agents Chemother. 2014;58(7):3895–3903.
- Kotsakis SD, Flach CF, Razavi M, Larsson DGJ. Characterization of the First OXA-10 Natural Variant with Increased Carbapenemase Activity. Antimicrob Agents Chemother. 2019;63(1):743.
- Majewski P, Gutowska A, Smith DGE, et al. Plasmid Mediated mcr-1.1 Colistin-Resistance in Clinical Extraintestinal Escherichia coli Strains Isolated in Poland. Front Microbiol. 2021;12:547020.
- Lo WU, Chow KH, Law PY, et al. Highly conjugative IncX4 plasmids carrying blaCTX-M in Escherichia coli from humans and food animals. J Med Microbiol. 2014;63(Pt 6):835–840.
- Wu R, Yi LX, Yu LF, et al. Fitness Advantage of mcr-1-Bearing IncI2 and IncX4 Plasmids in Vitro. Front Microbiol. 2018;9:331.
- Fernandes MR, McCulloch JA, Vianello MA, et al. First Report of the Globally Disseminated IncX4 Plasmid Carrying the mcr-1 Gene in a Colistin-Resistant Escherichia coli Sequence Type 101 Isolate from a Human Infection in Brazil. Antimicrob Agents Chemother. 2016;60(10):6415–6417.
- Ageevets V, Lazareva I, Mrugova T, Gostev V, Lobzin Y, Sidorenko S. IncX4 plasmids harbouring mcr-1 genes: further dissemination. J Glob Antimicrob Resist. 2019;18:166–167.
- Wu W, Feng Y, Tang G, Qiao F, McNally A, Zong Z. NDM Metallo-beta-Lactamases and Their Bacterial Producers in Health Care Settings. Clin Microbiol Rev. 2019;32(2):764.
- Ho PL, Li Z, Lo WU, et al. Identification and characterization of a novel incompatibility group X3 plasmid carrying bla NDM-1 in Enterobacteriaceae isolates with epidemiological links to multiple geographical areas in China. Emerg Microbes Infect. 2012;1(11):e39.
- Zhai R, Fu B, Shi X, et al. Contaminated in-house environment contributes to the persistence and transmission of NDM-producing bacteria in a Chinese poultry farm. Environ Int. 2020;139:105715.
