Abstract
Background
The elderly people generally have poor tolerance to drugs and an increased risk of adverse effects. Our study was designed to determine the effect and safety of Helicobacter pylori (H. pylori) eradication treatment based on molecular pathologic antibiotic resistance in Chinese elderly people over the age of 60 years.
Methods
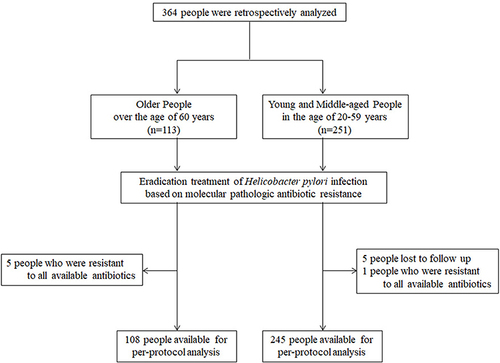
A total of 364 people were retrospectively analyzed, including 113 older people over 60 and 251 young and middle-aged people in the age of 20–59 years. Real-time PCR detection and conventional PCR and sequencing method were used for drug susceptibility testing. As the main outcome measure, the eradication rates (ERs) with their 95% confidence intervals (CIs) were analyzed by intention to treat (ITT) and per protocol (PP). For the safety of therapy, adverse events were analyzed.
Results
For the total people, the resistance rates to clarithromycin (CLR), amoxicillin (AMX), fluoroquinolone (FLQ) and tetracycline (TET) were 65.06%, 7.54%, 61.39% and 20.37%, respectively. After they were divided into two groups, the resistance rates were 62.39% (CLR), 9.09% (AMX), 69.64% (FLQ) and 22.45% (TET) in the 113 older people over 60, and 66.26%, 6.85%, 57.66% and 19.47% in the 251 young and middle-aged people in 20–59. By the ITT analysis, the ERs were 92.04% (95% CI, 86.97–97.10%, n=113) in the older people and 92.43% (95% CI, 89.14–95.73%, n=251) in the young and middle-aged people. By the PP analysis, the ERs were 96.30% (95% CI, 92.68–99.92%, n=108) and 94.69% (95% CI, 91.87–97.52%, n=245), respectively. No significant differences were shown both in the ITT analysis (P=0.896) and in the PP analysis (P=0.517). The three most common adverse events were black stool, dysgeusia and diarrhea, and no serious adverse event was reported.
Conclusion
H. pylori eradication treatment based on molecular pathologic antibiotic resistance showed good effect and safety in Chinese elderly people.
Introduction
Helicobacter pylori (H. pylori) infection has been regarded as the most important cause of chronic gastritis and it can lead to chronic active gastritis in almost all the people infected with H. pylori.Citation1 According to the Kyoto global consensus report on H. pylori gastritis, H. pylori can transmit easily between people and H. pylori gastritis has been defined as an infectious disease.Citation1,Citation2 Moreover, H. pylori infection has been identified as the main cause of a number of upper gastrointestinal diseases, including gastric ulcer, duodenal ulcer, gastric adenocarcinoma and gastric MALT (mucosa associated lymphoid tissue) lymphomas.Citation3,Citation4 Therefore, all H. pylori-infected people should be subjected to the eradication treatment, which can help to heal peptic ulcer, achieve remission of MALT lymphomas, and decrease the risk of gastric cancer.Citation5–7
For H. pylori treatment, clarithromycin-based triple therapy (proton pump inhibitor/ PPI + clarithromycin + amoxicillin/metronidazole) or bismuth quadruple therapy (PPI/H2RA + bismuth + metronidazole + tetracycline) are the recommended primary therapies in the United States, and bismuth-containing quadruple therapy (PPI + bismuth + two antibiotics) is the main recommended empirical therapy in China.Citation1,Citation8 The increasing prevalence of antibiotic resistance is our main concern in treatment of H. pylori infection, which can lead to significant eradication failure.Citation9,Citation10 In China, the resistance rates to clarithromycin, metronidazole, and levofloxacin, are already high. One study from Nanjing showed that the H. pylori resistance rates to clarithromycin, levofloxacin and metronidazole were 47.03%, 33.59% and 80.76%, respectively.Citation11
Ideally, treatment regimens of H. pylori eradication should be determined by the results of drug susceptibility testing. According to the recommendations by multiple authoritative guides, only regimens with eradication rates of ≥90% can be used for empirical treatment.Citation1,Citation2,Citation12,Citation13 H. pylori culture and molecular biology methods can be used for susceptibility testing. However, culture has a high specificity and a relatively low sensitivity, and certain technique is required.Citation1,Citation14 With the rapid development of molecular biology technology, some molecular markers have been used to predict H. pylori resistance, for example mutations of 23S rRNA, PBP1, gyrA and 16S rRNA for clarithromycin, amoxicillin, fluoroquinolone and tetracycline resistance, respectively.Citation14–17 Currently, molecular biology methods are practical for susceptibility testing.
For the eradication treatment of H. pylori infection in elderly people, the vast majority of gastroenterologists tend to be conservative because the elderly people generally have poor tolerance to drugs and an increased risk of adverse effects.Citation18 So far, there is no special guidelines and consensus reports for the treatment of H. pylori infection in elderly people, and we should comprehensively consider and balance the potential benefit and risk of eradication therapy. Since the influence of age remained uncertain, our study was designed to determine the effect and safety of H. pylori treatment based on molecular pathologic antibiotic resistance in Chinese elderly people over 60.
Materials and Methods
Study Population
A total of 364 people were retrospectively analyzed, including 113 older people over the age of 60 years and 251 young and middle-aged people in the age of 20–59 years. Inclusion criteria included: (1) people over the age of 20 years; (2) people who were Chinese; and (3) people who had been subjected to the gastroscopy and diagnosed with H. pylori infection by the pathological methods (PCR detection of UreA gene and Warthin-Starry silver staining) and 13C-UBT (urea breath test). Exclusion criteria included: (1) people who had been subjected to antimicrobial treatment within two months; (2) people who had received large surgery of upper gastrointestinal tract or malignancies; and (3) people who were suffering from other serious complications of major organs, including heart, liver, lung or kidney. The whole process of our research is in full compliance with the principles of the Declaration of Helsinki and our research project was approved by the Human Research Ethics Committee of our hospital. The written informed consent was obtained from all patients.
Gastroscopy Examination and Pathological Biopsy
All the people had been subjected to the gastroscopy examination and the biopsy specimens from the antrum and/or body of stomach were obtained. These specimens were fixed immediately in 4% paraformaldehyde and subsequently proceeded to be treated with gradient ethanol and xylene. After the gastric samples were prepared, they would be used for the pathological diagnosis, diagnosis of H. pylori infection, and detection of molecular pathologic antibiotic resistance for the four most effective antibiotics by poly-merase chain reaction (PCR) and real-time PCR analysis.
Pathological Diagnosis and Identification of H. pylori Infection
Hematoxylin Eosin (HE) staining was used for the pathological diagnosis, including the diagnosis of chronic non-atrophic gastritis, chronic atrophic gastritis, gastric ulcer and duodenal ulcer. The presence of H. pylori infection was determined by the two pathological methods (PCR detection of UreA gene and Warthin-Starry silver staining) and 13C-UBT. All the people were confirmed simultaneously by these three methods. The simple operation process and primers for PCR detection of UreA gene (F: 5’-GCCAATGGTAAATTAGTT-3′ R: 5’-CTCCTTAATTGTTTTTAC-3′) has been reported by our previous article.Citation14 Following the operation process provided by the manufacturer, the primers of UreA were designed and synthesized, and the products of PCR amplification were analyzed and sequenced at the NewgLife Inc. (China).
Clarithromycin Resistance by Real-Time PCR Detection
23S rRNA point mutations are the most frequently used molecular markers associated with clarithromycin resistance. A2143G, A2142G and A2142C of domain V, as the three main 23S rRNA point mutations, were determined by a TaqMan real-time PCR allelic discrimination assay (NewgLife, Beijing, China). The sequences of primers and probes for both DNA wild type and mutated DNA have been reported by our previous article.Citation14 Two different fluorescent dyes, including VIC dye and FAM dye, were used for the probes. As an example let us illustrate the A2143G site, the Hp-23S-A2143G-F was 5’-TCAGTGAAATTGTAGTGGAGGTGAAAA-3′ and the Hp-23S-A2143G-R was 5’-CAGTGCTAAGTTGTAGTAAAGGTCCA-3′. The VIC probe was 5’-AAGACGGAAAGACC-3′ for DNA wild type and the FAM probe was 5’-CAAGACGGAGAGACC-3′ for mutated DNA. For each experiment, positive and negative controls were used and all the specimens were repeated twice.
Amoxicillin, Fluoroquinolone and Tetracycline Resistance by PCR and Sequencing
Mutations of PBP1, gyrA and 16S rRNA have been regarded as the most important molecular markers associated with amoxicillin, fluoroquinolone and tetracycline resistance, respectively. These mutation sites were determined by the conventional PCR and sequencing method, and the sequences of primers for these target genes have been reported by our previous article.Citation14 As an example let us illustrate the primer sequences of PBP1 gene (F1: 5’-TAATTACGGCACCATGCTCA-3′ R1: 5’-GTGTTATCGTCCCTCCCAAA-3′; F2: 5’-CTTTCACGCCTATGGAAACC-3′ R2: 5’-CCCTCCCAAACCAGATCACC-3′). The conventional PCR amplifications were performed following the operation process provided by the manufacturer and the PCR amplification products were sequenced at the NewgLife Inc. (Beijing, China).
H. pylori Treatment Based on Molecular Pathologic Antibiotic Resistance
Three hundred and fifty-eight people were subjected to H. pylori infection eradication treatment because six people were resistant to all available antibiotics based on the results of molecular pathologic antibiotic resistance. Bismuth quadruple therapy for fourteen days was used to treat the 358 people, proton pump inhibitors in standard doses were adopted and the two antibiotics were determined by molecular pathologic antibiotic resistance. Within three days after they completed the treatment, adverse events were self-reported by the people and liver and renal functions were tested. Four weeks after treatment, histopathological examinations and/or 13C-UBT were used to determine the effect of eradication. Eight weeks after they concluded the treatment, 13C-UBT was repeated for these people and the eradication rates were calculated.
Statistical Analyses
SPSS 23.0 for Windows (SPSS, Chicago, IL, USA) was used for statistical analyses. Nearly all the parameters were categorical variables except for the age and they were described as numbers and proportions. Pearson chi-square test, continuity correction chi-square test, or Fisher’s exact test were used to compare the older people with the young and middle-aged people, including basic characteristics, results of molecular pathologic antibiotic resistance, eradication treatment regimens, eradication rates, and adverse events. As the main outcome measure, the eradication rates with their 95% confidence intervals were analyzed by intention to treat (ITT) and per protocol (PP). The second aim of our study was to determine the safety of eradication regimens, and the incidences of fifteen kinds of adverse events were recorded and compared.
Results
People’ Characteristics
A total of 364 people were retrospectively analyzed, including 113 older people over the age of 60 years (one group as People Over 60) and 251 young and middle-aged people in the age of 20–59 years (another group as People in 20–59). showed the people’ characteristics. For the total 364 people, their mean age was 52.1 ± 14.4 years and 153 (42.0%) were male. All of them had been subjected to the gastroscopy and the results showed that 364 people (100%) were diagnosed with H. pylori infection by the histopathological examinations and 13C-UBT. Chronic non-atrophic gastritis, chronic atrophic gastritis, duodenal ulcer and gastric ulcer were found in 210 (57.7%), 154 (42.3%), 42 (11.5%) and 10 (2.7%) people, respectively ().
Table 1 People’ Characteristics
The flow diagram of our study was shown in . The people were subjected to the H. pylori eradication treatment for fourteen days based on the results of antibiotic resistance determined by the molecular pathologic methods. The bismuth quadruple therapy was used for all the people, and after treatment, pathological examinations or 13C-Urea breath test were adopted to determine the positive or negative status of H. pylori infection. As shown in , 199 (54.7%) people had received H. pylori eradication treatment before, including 54 people over the age of 60 and 145 people in 20–59. Finally, there were 353 people available for the PP analysis because five people were lost to follow up and six people were resistant to all available antibiotics.
For the 113 older people over 60, the mean age was 68.4 ± 6.9 years and 81 (71.7%) were diagnosed with chronic atrophic gastritis (CAG). Compared with the younger people in 20–59 (), the elderly people had a higher percentage of CAG (58.4% vs 25.9%, P<0.001) and a lower percentage of chronic non-atrophic gastritis (24.8% vs 61.0%, P<0.001). No significant differences were found for the percentage of male people (P=0.908) and the treatment history of H. pylori eradication (P=0.077).
Molecular Pathologic Antibiotic Resistance of H. pylori Infection
Six antibiotics were recommended by the Fifth Chinese National Consensus Report on the management of H. pylori infection, including amoxicillin (AMX), clarithromycin (CLR), metronidazole (MNZ), fluoroquinolone (FLQ), furazolidone (FZD) and tetracycline (TET).Citation1 For CLR, AMX, FLQ and TET, the drug resistance was determined by the molecular pathologic methods, which had been taken as the most important basis of choosing the treatment regimens of H. pylori eradication.
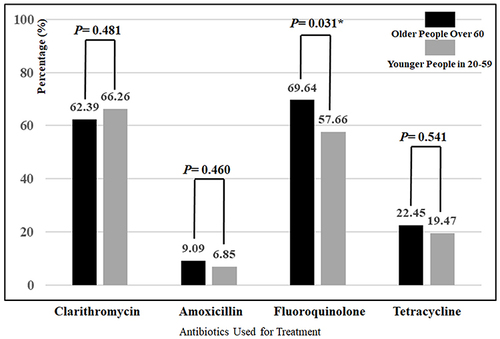
The results of molecular pathologic antibiotic resistance were shown in and . For the total 364 people, the resistance rates to CLR, AMX, FLQ and TET were 65.06%, 7.54%, 61.39% and 20.37%, respectively. After they were divided into two groups, the resistance rates were 62.39% (CLR), 9.09% (AMX), 69.64% (FLQ) and 22.45% (TET) in the 113 older people over the age of 60, and 66.26%, 6.85%, 57.66% and 19.47% in the 251 young and middle-aged people in 20–59. Significant difference was only found for fluoroquinolone (P=0.031), but not for the other three antibiotics. The elderly people had a higher percentage of resistance rate to FLQ.
Table 2 Molecular Pathologic Antibiotic Resistance of H. pylori Infection
Figure 2 The prevalence of molecular pathologic antibiotic resistance in elderly people. The black histogram indicates the percentage of antibiotic resistance in older people over the age of 60 years and the gray histogram indicates the percentage in young and middle-aged people in the age of 20–59 years. As shown, the resistance rates to clarithromycin, amoxicillin, fluoroquinolone and tetracycline were 62.39%, 9.09%, 69.64% and 22.45% in older people, and the rates were 66.26%, 6.85%, 57.66% and 19.47% in younger people, respectively. Significant difference was only found for fluoroquinolone (P=0.031). Data were available in the 352, 358, 360 and 324 patients for the above four antibiotics. *P<0.05.
Moreover, the rates of multidrug resistance (MDR) and the differences between the elderly people and the younger people were analyzed (). For dual drug resistance, 170 (48.71%), 53 (16.51%) and 45 (14.02%) people had drug resistance to CLR + FLQ, CLR + TET and FLQ + TET, respectively. For triple drug resistance, compared with the younger people, the elderly people had higher rates of antibiotic resistance to CLR + AMX + TET (6.19% vs 1.35%, P=0.042) and AMX + FLQ + TET (5.15% vs 0.90%, P=0.049). For quadruple drug resistance, six people were resistant to CLR + AMX + FLQ + TET, and five people were over the age of 60.
Eradication Treatment Regimens of H. pylori Infection
Five antibiotics were used in our study, including AMX, CLR, FLQ, FZD and TET (). FZD was fit for empirical therapy because the resistance rate was very low in our country.Citation19,Citation20 There were 358 people subjected to bismuth quadruple therapy for fourteen days because six people were resistant to all available antibiotics. The PPIs in standard doses were used and the two antibiotics were determined by the molecular pathologic antibiotic resistance. As shown in , the four most common treatment regimens were AMX + TET (105 people, 29.3%), AMX + FLQ (84 people, 23.5%), AMX + CLR (63 people, 17.6%) and AMX + FZD (54, 15.1%). Between the older people over 60 and younger people in 20–59, significant difference was only found for the usage of AMX + CLR (24.1% vs 14.8%, P=0.034).
Table 3 Eradication Treatment Regimens of H. pylori Infection
Effect of H. pylori Eradication Treatment
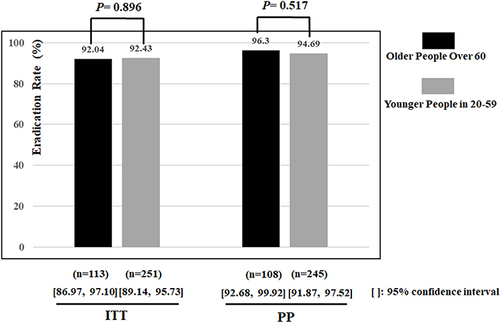
By the ITT analysis, the eradication rates (ERs) were 92.04% (95% confidence interval/CI, 86.97–97.10%, n=113) in the older people over the age of 60 and 92.43% (95% CI, 89.14–95.73%, n=251) in the young and middle-aged people in 20–59. By the PP analysis, the ERs were 96.30% (95% CI, 92.68–99.92%, n=108) and 94.69% (95% CI, 91.87–97.52%, n=245) in the older and younger people, respectively (). The statistical data showed that no significant differences were found both in the ITT analysis (P=0.896) and in the PP analysis (P=0.517). Seventeen people failed in the eradication treatment, including four elderly people and thirteen younger people. Among these 17 people, 16 (n=17), 0 (n=16), 14 (n=17) and 4 (n=16) people were found to have antibiotic resistance to CLR, AMX, FLQ and TET, respectively.
Figure 3 Eradication rates of H. pylori treatment based on antibiotic resistance in elderly people. The black and gray histograms indicate the eradication rates in older people over the age of 60 and in young and middle-aged people in the 20–59.
Adverse Events and Safety of Eradication Regimens
The 353 people were analyzed because five people were lost to follow up. As shown in , fifteen kinds of adverse events were reported during the treatment and the three most common symptoms were black stool (325 people, 92.1%), dysgeusia (72 people, 20.4%) and diarrhea (13 people, 3.7%). Compared with the younger people, the elderly people had a higher rate of constipation (5.6% vs 1.2%, P=0.044).
Table 4 Adverse Events and Safety
Discussion
H. pylori infects about half of the world’s population, including plenty of elderly people. Currently, bismuth-containing quadruple therapy for fourteen days is the main recommended therapy in our country.Citation1 According to the recommendations by the Fifth National Consensus Report, six antibiotics and seven treatment regimens are commonly used, including amoxicillin, clarithromycin, tetracycline, metronidazole, levofloxacin and furazolidone.Citation1,Citation14 As one physician, we are likely to somewhat hesitant when we prepare to prescribe these antibiotics for elderly people over the age of 60, because they generally have poor tolerance to drugs and an increased risk of adverse effects.Citation18 Our study was designed to determine the effect and safety of H. pylori treatment based on molecular pathologic antibiotic resistance in elderly people.
A total of 364 people were included in our study and 113 (31.04%) were over the age of 60 years. Molecular biology methods, including real-time PCR and conventional PCR and sequencing, were used to determine the molecular pathologic antibiotic resistance. The results showed that the resistance rates to clarithromycin, amoxicillin, fluoroquinolone and tetracycline were 62.39%, 9.09%, 69.64% and 22.45% in the 113 elderly people, respectively. The eradication rates were 92.04% (95% CI, 86.97–97.10%) and 96.30% (95% CI, 92.68–99.92%) by the ITT and PP analyses. No significant differences were found between the younger people and elderly people. In addition, no serious adverse event was reported, even in the elderly people.
H. pylori culture and molecular biology methods can be used for drug susceptibility testing. Compared with the culture, molecular biology methods are relatively simpler and more economic approaches, which are practical for H. pylori susceptibility testing.Citation1,Citation14 Currently, some molecular markers have been used to predict the antibiotic resistance of H. pylori treatment, for example 23S rRNA point mutations which can be detected in more than 90% of people with clarithromycin resistance.Citation14 Mutations of 23S rRNA (A2143G, A2142G and A2142C of domain V), PBP1, gyrA and 16S rRNA associated with CLR, AMX, FLQ and TET resistance were detected by real-time PCR and conventional PCR and sequencing method in our study. Their sequences of primers and probes have been reported by our previous article.Citation14
Primary resistance and secondary resistance (post-treatment) are the two kinds of H. pylori antibiotic resistance. Our previous study included 111 patients treated for the first time and 150 patients who failed at least once in bismuth-containing quadruple therapy.Citation14 The results showed that the primary resistance rates were 42.1% (CLR), 5.5% (AMX), 41.7% (FLQ) and 12.9% (TET), and the secondary resistance rates were 79.7%, 11.7%, 70.7% and 30.0%, respectively. In our current study, 165 (45.3%) people were treated for the first time and no statistical difference was found between the elderly people and younger people (). As yet, the studies on H. pylori resistance in elderly patients are very limited.Citation21 One Bulgarian study showed that the resistance rates were 22.6% (clarithromycin), 32.3% (levofloxacin), 1.6% (tetracycline) and 1.6% (amoxicillin) in elderly patients aged 66–93 years.Citation21
For the H. pylori treatment in elderly people, our study showed good effect that the eradication rates (ERs) were 92.04% and 96.30% by the ITT and PP analyses. The results were compared with those reported by the researches focusing on the elderly people in the other countries over the world.Citation22–26 Fifteen elderly patients with type B gastritis were included in one study from the United Kingdom and the ER was 85% (12/15).Citation22 Two studies were conducted to treat the elderly patients with H. pylori infection in the Italy.Citation23,Citation25 In one study from Vicenza, 88 older patients aged 60–89 years were included and the ER was 63.6% (56/88).Citation23 In another study from the University of Turin, 361 patients aged more than 65 years were included and the ERs were 70.9% (256/361) and 73.1% (256/350) by the ITT and PP analyses.Citation25 Compared with these studies, better effect was obtained in our study, indicating that H. pylori treatment based on molecular pathologic antibiotic resistance was practical.
For the safety of H. pylori eradication in elderly people, our study showed good safety and no serious adverse event was reported. In our study, the three most common adverse events were black stool, dysgeusia and diarrhea, and no one was discontinued because of adverse events. One retrospective study from Japan included 1271 patients with H. pylori infection and they were divided into three groups according to their ages (<65, 65–74, >75 years old).Citation26 The ERs for the first and second treatment were 92.1% (1044/1133) and 84.2% (123/146). The rates of adverse events were 9.1% and 8.9% for the first and second treatment. No significant differences were found for both the ERs and rates of adverse events between the three groups.Citation26 We gained the similar results, which indicated that H. pylori eradication is safe for elderly people.
The best effort of our study was that the eradication regimens were determined by the results of molecular pathologic antibiotic resistance. Satisfactory eradication rates and good safety were obtained in our current study, which indicated that this method used for H. pylori treatment was practical for elderly people. The first limitation was that our study population was from one large-scale medical center and the selection bias may not be avoided. The second limitation was that only 113 older people over 60 were included in our study. More people, more centers and more studies are required.
In conclusion, eradication treatment of H. pylori infection based on the results of molecular pathologic antibiotic resistance showed good effect and safety in Chinese elderly people over the age of 60 years. Compared with H. pylori culture, molecular biology methods are relatively simpler and more economic approaches, and we hope that they could be used widely for H. pylori resistance testing, even in elderly people.
Ethics Approval and Informed Consent
The whole process of our research is in full compliance with the principles of the Declaration of Helsinki and our research project was approved by the Human Research Ethics Committee of China-Japan Friendship Hospital, Ministry of Health. The written informed consent was obtained from all patients.
Author Contributions
Both authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- Liu WZ, Xie Y, Lu H, et al. Fifth Chinese National Consensus Report on the management of Helicobacter pylori infection. Helicobacter. 2018;23(2):e12475. doi:10.1111/hel.12475
- Sugano K, Tack J, Kuipers EJ, et al. Kyoto global consensus report on Helicobacter pylori gastritis. Gut. 2015;64(9):1353–1367. doi:10.1136/gutjnl-2015-309252
- Cho J, Prashar A, Jones NL, Moss SF. Helicobacter pylori infection. Gastroenterol Clin North Am. 2021;50(2):261–282. doi:10.1016/j.gtc.2021.02.001
- Jessurun J. Helicobacter pylori: an evolutionary perspective. Histopathology. 2021;78(1):39–47. doi:10.1111/his.14245
- Sanaei MJ, Shirzad H, Soltani A, et al. Up-regulated CCL18, CCL28 and CXCL13 expression is associated with the risk of gastritis and peptic ulcer disease in Helicobacter pylori infection. Am J Med Sci. 2021;361(1):43–54. doi:10.1016/j.amjms.2020.07.030
- Della Bella C, Soluri MF, Puccio S, et al. The Helicobacter pylori CagY protein drives gastric Th1 and Th17 inflammation and B cell proliferation in gastric MALT lymphoma. Int J Mol Sci. 2021;22(17):9459. doi:10.3390/ijms22179459
- Ford AC, Yuan Y, Moayyedi P. Helicobacter pylori eradication therapy to prevent gastric cancer: systematic review and meta-analysis. Gut. 2020;69(12):2113–2121. doi:10.1136/gutjnl-2020-320839
- Graham DY, Megraud F. Classification system for Helicobacter pylori therapies: compared and contrasted to traditional infectious disease therapy. Helicobacter. 2021;26(1):e12773. doi:10.1111/hel.12773
- Gong EJ, Ahn JY, Kim JM, et al. Genotypic and phenotypic resistance to clarithromycin in Helicobacter pylori strains. J Clin Med. 2020;9(6):1930. doi:10.3390/jcm9061930
- Gong M, Han Y, Wang X, et al. Effect of temperature on metronidazole resistance in Helicobacter pylori. Front Microbiol. 2021;12:681911. doi:10.3389/fmicb.2021.681911
- Jiang ZD, He BS, Zhang ZY, Wang SK, Ran D, Wang ZB. Analysis of the primary and post-treatment antibiotic resistance of Helicobacter pylori in the Nanjing area. Curr Pharm Biotechnol. 2021;22(5):682–685. doi:10.2174/1389201021666200722162613
- Liou JM, Malfertheiner P, Lee YC, et al. Screening and eradication of Helicobacter pylori for gastric cancer prevention: the Taipei global consensus. Gut. 2020;69(12):2093–2112. doi:10.1136/gutjnl-2020-322368
- Ding SZ, Du YQ, Lu H, et al. Chinese consensus report on family-based Helicobacter pylori infection control and management (2021 Edition). Gut. 2022;71(2):238–253. doi:10.1136/gutjnl-2021-325630
- Gao C, Du SY, Fang L, Fan YH, Song AP, Chen H. Eradication treatment of Helicobacter pylori infection based on molecular pathologic antibiotic resistance. Infect Drug Resist. 2020;13:69–79. doi:10.2147/IDR.S232169
- Albasha AM, Elnosh MM, Osman EH, et al. Helicobacter pylori 23S rRNA gene A2142G, A2143G, T2182C, and C2195T mutations associated with clarithromycin resistance detected in Sudanese patients. BMC Microbiol. 2021;21(1):38. doi:10.1186/s12866-021-02096-3
- Haumaier F, Schneider-Fuchs A, Backert S, Vieth M, Sterlacci W, Wöhrl BM. Rapid detection of quinolone resistance mutations in gyrA of Helicobacter pylori by real-time PCR. Pathogens. 2022;11(1):59. doi:10.3390/pathogens11010059
- Gantuya B, El Serag HB, Saruuljavkhlan B, et al. Advantage of 16S rRNA amplicon sequencing in Helicobacter pylori diagnosis. Helicobacter. 2021;26(3):e12790. doi:10.1111/hel.12790
- Peng C, Hu Y, Ge ZM, Zou QM, Lyu NH. Diagnosis and treatment of Helicobacter pylori infections in children and elderly populations. Chronic Dis Transl Med. 2020;5(4):243–251. doi:10.1016/j.cdtm.2019.12.003
- Ji CR, Liu J, Li YY, et al. Safety of furazolidone-containing regimen in Helicobacter pylori infection: a systematic review and meta-analysis. BMJ Open. 2020;10(10):e037375. doi:10.1136/bmjopen-2020-037375
- Wang J, Cao Y, He W, Li X. Efficacy and safety of bismuth quadruple regimens containing tetracycline or furazolidone for initial eradication of Helicobacter pylori. Medicine. 2021;100(51):e28323. doi:10.1097/MD.0000000000028323
- Boyanova L, Gergova G, Markovska R, et al. Primary Helicobacter pylori resistance in elderly patients over 20 years: a Bulgarian study. Diagn Microbiol Infect Dis. 2017;88(3):264–267. doi:10.1016/j.diagmicrobio.2017.05.001
- Safe AF, Warren B, Corfield A, et al. Role of serology in monitoring treatment for Helicobacter pylori infection in elderly patients. Age Ageing. 1993;22(4):256–259. doi:10.1093/ageing/22.4.256
- Pilotto A, Franceschi M, Leandro G, et al. The clinical usefulness of serum pepsinogens, specific IgG anti-HP antibodies and gastrin for monitoring Helicobacter pylori treatment in older people. J Am Geriatr Soc. 1996;44(6):665–670. doi:10.1111/j.1532-5415.1996.tb01829.x
- Pilotto A, Di Mario F, Franceschi M, et al. Cure of Helicobacter pylori infection in the elderly: effects of eradication on gastritis and serological markers. Aliment Pharmacol Ther. 1996;10(6):1021–1027. doi:10.1046/j.1365-2036.1996.88260000.x
- Durazzo M, Ferro A, Fagoonee S, Staiano MT, Saracco GM, Pellicano R. Helicobacter pylori eradication with a clarithromycin-based triple therapy in elderly patients. Panminerva Med. 2021;63(3):332–335. doi:10.23736/S0031-0808.21.04500-6
- Kobayashi S, Joshita S, Yamamoto C, et al. Efficacy and safety of eradication therapy for elderly patients with Helicobacter pylori infection. Medicine. 2019;98(30):e16619. doi:10.1097/MD.0000000000016619