Abstract
Background
Infectious diabetic foot ulcers (IDFU) are a widespread health issue that affects people all over the world. IDFU, like other medical disorders, can have negative implications if drug resistance develops. Clinicians will be able to choose the optimal antibiotics to treat impacted patients based on the antibiotic susceptibility pattern of bacterial strains. In this project, we attempted to evaluate the levels of extended-spectrum beta-lactamase (ESBL), carbapenemase, and MRSA in patients with diabetic foot ulcers.
Methods
A sterile swab was used to collect a sample from the leg ulcer, while a sterile needle was used to collect the aspirated pus. Bacteria identification and antibiotic susceptibility tests are carried out based on conventional bacterial culture. The double-disc inactivation method and modified carbapenem (meropenem) were used to screen the production of ESBL and carbapenemase.
Results
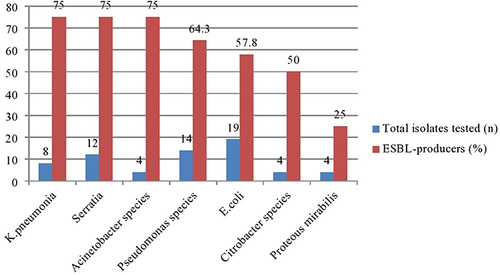
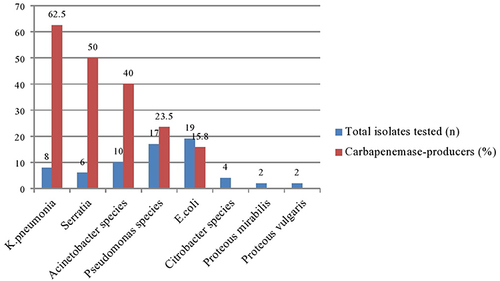
Of the 76 isolates tested, 53.9% (41/76) were phenotypically ESBL producers. K. pneumoniae 75% (6/8), Acinetobacter species 75% (9/12), Serratia species 75% (3/4), Pseudomonas species 64.3% (14/9), E. coli 57.8% (11/19), Citrobacter species 50% (2/4) and Proteus mirabilis 25% (1/4) had the highest frequency of ESBL production. Of the 68 GNB isolates tested, 27.9% (19/68) were carbapenemase-producing organisms. K. pneumoniae 62.5% (5/8), Serratia 50% (3/6), Acinetobacter species 40% (4/10), Pseudomonas species 23.5% (4/17) and E. coli 15.8% (3/19) are the top five major carbapenemase producers. In this study, 32 isolates of Staphylococcus aureus were tested for methicillin resistance. Among them, 81.3% (26/32) were methicillin-resistant Staphylococcus aureus (MRSA), and 18.7% (6/32) of the remaining isolates were methicillin-sensitive Staphylococcus aureus (MSSA).
Conclusion
The result draws attention to the management of diabetic foot ulcer infections based on the results of microbiological analysis and drug susceptibility testing.
Keywords:
Introduction
Diabetes mellitus is a chronic disease that can be seen all over the world and over time causes serious damage to many organs and systems in the body. Retinopathy, cardiovascular disease, high blood pressure, kidney failure, neuropathy, diabetic foot ulcers, and many other complications are considered signs of long-term specific effects.Citation1
Diabetic foot ulcer (DFU) is one of the most serious and devastating complications of diabetes mellitus (DM). It is defined as the foot below the ankle affected by ulceration/thickening wound/involving neuropathy and/or peripheral arterial disease of the lower limbs in diabetics.Citation2,Citation3 As various studies report, the main risk factors for developing DFU are diabetic neuropathy (90%), peripheral artery disease (210%), and subsequent table trauma to the legs.Citation2
Other risk factors include deformities and structural abnormalities of the foot, a history of ulcers or amputations of the foot, poor blood sugar control, and smoking. In addition, the risk of foot ulcers and amputation increases with age and duration of diabetes.Citation4,Citation5 According to various parameters (such as extent, size and depth, location, presence of infection, and ischemia), the severity of DFU is divided into different categories by different groups, such as Meggitt–Wagner Classification System, The Infectious Diseases Society of America (IDSA) Classification Scheme and the International Working Group Diabetic Foot (IWGDF).Citation6,Citation7 Meggitt–Wagner classification is one of the most common DFU classification systems and it has six grades based on the depth of ulcer, presence of gangrene, and extent of tissue necrosis.Citation7,Citation8
Although peripheral neuropathy and peripheral arterial disease (PAD) are considered the most significant risk factors for DFU occurrence, microorganisms facilitate the severity of diabetic foot ulcers. As different articles currently show different pathogenic microbes,Citation9 infect greater than 50% of the ulcerated foot of diabetes patients. Signs like inflammation (erythema, oedema, heat, pain) and purulent discharge classically characterize infection, but in diabetic foot wounds, this is not typical due to ischemia and neuropathy. The Infectious Diseases Society of America (IDSA) and International Working Group on the Diabetic Foot (IWGDF) have put criteria (definition) to measure the severity of DFIs such as uninfected, mild, moderate, and severe infection.Citation10,Citation11 Due to DFU, intact skin loses many of its barriers or defense mechanisms, and invading microorganisms can easily enter through the wound portal. Pathogenic microorganisms that colonize diabetic foot wounds cause local tissue damage.
Bacterial growth is promoted by the presence of tissue ischemia (leading to hypoxia) or necrosis, as well as by hyperglycemia affecting the host defenses.Citation12
Infections start as a minor problem, but progress to conditions that cannot be controlled (involving deep tissue, joints, or bones). DFU occurs over a long period and severe infection is often associated with bacterial colonization.Citation7,Citation12
Several authors have reported that both aerobic and anaerobic microorganisms including multidrug resistance microorganisms (MDRO) with the ability to form biofilm are isolated from foot ulcers patients.Citation13 Among gram-positive bacteria; Enterococcus spp.,Bacteroides spp., Peptostreptococcus spp., Veillonella spp., and Clostridium perfringens have been identified.Citation14,Citation15 The most commonly isolated gram-negative bacteria include Enterobacteriaceae (E. coli, Proteus spp.,K. pneumonia, etc) and none fermenters include (P. aeruginosa, and Acinetobacter spp.) and have also been identified.Citation16,Citation17 Additionally, fungi (such as candida) are also common and have been implicated in the delayed healing of DFUs.Citation18
The source of these bacteria is in the environment, adjacent skin, or other endogenous sources, including the gastrointestinal tract.Citation19 Risk factors associated with MRSA, such as invasive devices, previous hospitalization, and comorbid illness, were found to be significantly associated with MRSA.Citation20 Diabetic foot ulcer infection is also a characteristic or comorbid related to immune compromised diseases.
Nowadays, the incidence and prevalence of ESBL have been increasing. ESBL production is an important resistance mechanism hampering the antimicrobial treatment of infections caused by Enterobacteriaceae and poses a serious threat to the arsenal of currently available antibiotics.
Currently, there are little data on ESBL-producing organisms and carbapenemase producers for diabetic foot infections in Ethiopia. Therefore, this study aimed to determine the burden of resistant microorganisms, ESBL and carbapenemase production, and methicillin-resistant Staphylococcus aureus that infect diabetic foot ulcers.
Materials and Methods
A multicenter-institutional-based cross-sectional study was conducted in Addis Ababa, Ethiopia, from November 2020 to May 2021.
Ethical Consideration
The ethical review was first obtained from the ethics and review committee of the Department of Microbiology, Immunology and Parasitology, College of Health Sciences, Addis Ababa University, and was approved by the Department Ethical Review Committee (meeting no. DERC/005/2020). The Addis Ababa Public Health Research and Emergency Management Agency had also approved it. The formal written letter had been distributed to each hospital included in this study. Before collecting data, study participants were informed of the study and obtained their consent, and confidentiality was maintained by omitting their names and personal identifiers throughout the study (Supp1). This study was also conducted per the Declaration of Helsinki.
Sample Collection, Transport, Process, Culture and Identification
A sterile swab was used to collect a sample from the leg ulcers, while a sterile needle was used to collect the aspirated pus. Staurt’s transport medium was used for transporting swabbed and tissue samples within 2 hours. After the sample reaches in the laboratory, Gram stain, culture on (Blood Agar, MacConkey, Manito Salt Agar), subculture, and a panel of biochemical testing were done to isolate the bacteria.
Antibiotics Susceptibility Testing
Per CLSI guidelines (2021), the Kirby–Bauer disk diffusion method was used for antibiotic susceptibility testing.Citation22 The antibacterial discs used for the test are ampicillin (20 µg), aztreonam (30 µg), gentamicin (10 µg), amikacin (30 µg), cefazolin (30 µg), ceftazidime (30 µg), cefotaxime (30 µg), (30 µg), cefepime (30 µg), cefoperazone/sulbactam (75/10 µg), piperacillin/tazobactam (100/10 µg), Imipenem (10 µg), meropenem (10 µg), and polymyxin B (300 units) against gram-negative bacilli.
Penicillin, ampicillin, azithromycin (15µg), cefoxitin (30µg), cefotaxime (30µg), chloramphenicol (30µg), clindamycin (2µg), erythromycin (15µg), oxacillin (1µg), vancomycin (30µg), and teicoplanin (30µg)), ciprofloxacin, ofloxacin (5µg), linezolid (30µg) and tetracycline (30µg) were used to study the susceptibility patterns of the gram-positive cocci. The production of MRSA, ESBL, and carbapenemase had been detected according to the CLSI 2021 guidelines.Citation22
Methicillin-Resistant Staphylococcus aureus (MRSA) Detection
Cefoxitin discs (30 µg) were used for phenotypic testing for MRSA. A zone of inhibition equal to or greater than 22 mm was considered sensitive to cefoxitin and the organism was reported as methicillin-sensitive Staphylococcus aureus (MSSA). Isolates with a zone of inhibition less than or equal to 21 mm were considered methicillin-resistant Staphylococcus aureus (MRSA).
Extended-Spectrum β-Lactamase (ESBL) Production
The production of ESBL was confirmed using ceftazidime tablets (30 µg) and ceftazidime clavulanate (30/10 µg). The test organisms were inoculated on Mueller–Hinton agar plates, and the above discs were placed on the plates.
Plates were incubated overnight at 37°C and checked the next day. Compared with the antimicrobial agent tested alone, the area diameter of the antimicrobial agent tested in combination with clavulanic acid increased by 5 mm or more, indicating that the strain is a producer of ESBL.
Carbapenemase Production Screening
The production of carbapenemase was detected by a modified Hodge test. The 0.5 Mac Farland suspension of ATCC E. coli 25922 was diluted 1 to 10 in sterile saline. As a conventional disk diffusion test, it was inoculated on the MHA media. The plate was dries was for 5 minutes; then a 10 µg meropenem plate was placed in the center of the agar plate. A few colonies were picked from the test organism and directly inoculated on the edge of the disc at least 20 mm away. The plate was incubated overnight at 37°C and checked the next day. Around the test organism, an improvement in growth was observed at the intersection of the straight line and the zone of inhibition. The presence of improved growth indicates that carbapenemase is produced, while no improvement in growth means that the test isolate does not produce carbapenemase.
Data Analysis
The data were entered into EpiData v.4.6.0.4 and cleaned and analyzed with statistical software SPSS 25 version (IBM Corporation, Comp.soft-sys.stat.spss). Descriptive statistics such as frequency and percentage were used to report a numerical summary of the survey results. The quantitative value model is presented through graphical representation and statistical tables.
Result
Sociodemographic Data of the Study Participants
One hundred and thirty participants were included and out of the total 88 (67.89%) were males and 42(32.3%) were females. The majority of the study participants were in the age group of 50–75 years. Among the study participants, type-I DM was in 51.9%, and 48.4% participants had type-II DM. In this study, the Meggitt–Wagner classification system was used to classify DFU. The majority of study participants came with grade three in 48.4%, followed by grade two 33.59%, 14.8% with grade four, 2.3% with grade one, and grade five in 0.8%.
Magnitude of ESBL-Productions
In this study, 76 gram-negative isolates were tested for the production of ESBL. Of the tested 76 GNB isolates, 53.9% (41/76) were phenotypically ESBL-producer while 46.05% (35/76) were non-ESBL-producers. High ESBL production rates was observed among K. pneumoniae 75% (6/8), Acinetobacter species 75% (9/12), Serratia 75% (3/4), Pseudomonas species 64.3% (9/14), and followed by E. coli 57.8% (11/19), Citrobacter species 50% (2/4), Proteus mirabilis 25% (1/4) ().
The Magnitude of Carbapenemase Production
Carbapenemase-producers of gram-negative bacteria isolate phenotypical determination of carbapenemase-producer pathogenic gram-negative bacterial isolate. Based on the modified disk inactivation (meropenem) method,Citation22 the carbapenemase test was done for 68 ESBL positive and Imipenem or Meropenem resistant gram-negative isolates.
Out of 68 pathogenic gram-negative bacteria isolates, 27.9% (19/68) were carbapenemase-producer, whereas 73.53% (50/68) were non-carbapenemase-producer. High carbapenemase-producers rate was observed among K. pneumoniae 5/8(62.5%), followed by Serratia 3/6(50%), Acinetobacter species 4/10(40%), Pseudomonas species 4/17(23.5%), E. coli 3/19(15.8%), and the rest of the isolates were non-producers ().
The Burden of Methicillin-Resistant S. aureus (MRSA)
In this study, 32 isolates of Staphylococcus aureus were screened for methicillin resistance. Of these, the majority of the isolates 81.3 (26/32) were methicillin-resistant Staphylococcus aureus (MRSA) and the rest of the isolates were methicillin-sensitive Staphylococcus aureus (MSSA) 18.7% (6/32). Almost 50% of the isolates screened for MRSA were susceptible to amikacin, clindamycin, chloramphenicol, vancomycin, and ciprofloxacin.
Discussion
Antimicrobial resistance is a deep-rooted scientific problem in hospitals and community settings. Rapid tests in clinical laboratories are crucial for the correct identification of antibiotic-resistant microorganisms. The production of extended-spectrum β-lactamases (ESBL) is an important mechanism of drug resistance, which makes antibacterial treatment of Enterobacteriaceae infections difficult and represents a serious threat to the currently available group of antibiotics.Citation23
Of the 76 gram-negative bacteria, more than half of the isolates (53.95%) were ESBL-producers, which are consistent with the study documented in India (53%),Citation24 in Egypt 49%.Citation36
In poor resource settings, the burdens of ESBL producing gram-negative bacteria are more prevalent among DFU patients. Some reports, from the Middle East and North Africa, showed that the ESBL-producing bacteria range from 11% to 53%.Citation25 Other studies also supported this finding 46% in eastern India,Citation26 42% in Odisha, India,Citation27 38% in Istanbul Turkey,Citation28 33% in Nigeria,Citation29 and 31% in Iran.Citation30
The present study indicated that gram-negative ESBL-producers in patients with DFU was high among K. pneumoniae 75% (6/8), Acinetobacter species 75% (9/12), Serratia 75% (3/4), Pseudomonas species 64.3% (9/14), and followed by E. coli 57.8% (11/19), Citrobacter species 50% (2/4), and Proteus mirabilis 25% (1/4). This finding is somehow different from the study conducted in Iran that reported Acinetobacter species (50%) followed by E. coli (36%), P. aeruginosa (33%), and Enterobacter species (25%).Citation30
Of the 68 gram-negative bacteria analyzed in this study, 19 (27.9%) were positive for the carbapenemase phenotype. A high rating was recorded among K. pneumoniae followed by Acinetobacter species,E. coli, Pseudomonas species, and Serratia species. The results of the current research are superior to those carried out in Egypt, of which 3.6% are carbapenemase producers,Citation36 including a recent study carried out in the same country that shows 11.7% from carbapenemase producersCitation32 and 3.1% carbapenemase producers in Nigeria.Citation27
Methicillin-resistant Staphylococcus aureus (MRSA) has long been considered a significant human pathogen and the most common cause of hospital-acquired infections. Developing resistance to treatment options for treating infections caused by Methicillin-resistant Staphylococcus aureus is an emerging issue.Citation33
In this study, 32 isolates of Staphylococcus aureus were screened for methicillin resistance. Of these, the majority of the isolates 81.3% (26/32) were methicillin-resistant Staphylococcus aureus (MRSA) and the rest of the isolates were methicillin-sensitive Staphylococcus aureus (MSSA) 18.7% (6/32). This finding is in line with the study documented in Arbaminch, Ethiopia (82.3%) and Eretria 72%.Citation31,Citation32 However, the present prevalence rate is higher than the study documented previously in Egypt 10.1%, 15.8%.Citation25,Citation34
In this study, nearly 50% of the isolates screened for MRSA were sensitive to amikacin and chloramphenicol. These results far exceed previous reports, which showed that methicillin-susceptible isolates of Staphylococcus aureus were susceptible to clindamycin, vancomycin, and ciprofloxacin. However, these results are consistent with studies previously reported in Ethiopia,Citation31 Egypt,Citation25,Citation34 and Sudan.Citation35
Limitations of the Study
Because of the lack of molecular methods and primes, molecular testing of ESBL, carbapenemase producers, and genes encoding MRSA in the analyzed isolates was not performed as a confirmatory test.
Conclusion
The result shows that greater than 50% of the isolated gram-negative bacteria were phenotypically ESBL producers, significant number of isolated gram-negative bacteria were phenotypically carbapenemase producers, and high number of the S. aureus isolates were methicillin-resistant. This draws attention to the management of diabetic foot ulcer infections based on the results of microbiological analysis and drug susceptibility testing.
Abbreviations
CLSI, Clinical and Laboratory Standards Institute; DFU, diabetic foot ulcer; ESBL, extended-spectrum beta-lactamase; MRSA, methicillin-resistant S. aureus; MSSA, methicillin-sensitive S. aureus; MDR, multidrug-resistant organism.
Disclosure
The authors have no conflicts of interest to be declared.
Acknowledgments
Authors would like to acknowledge the data collectors, particularly health extension workers. In addition, the authors are grateful to the study participants for their voluntary participation. Finally, the authors acknowledged their appreciation for the funding provided by Addis Ababa University’s postgraduate school for this research. This paper is based on the thesis of Asegdew Atlaw. It has been published on the institutional website.Citation21
Additional information
Funding
References
- Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications. Phys Ther. 2008;88(11):1254–1264. doi:10.2522/ptj.20080020
- Alexiadou K, Doupis J. Management of diabetic foot ulcers. Diabetes Ther. 2012;3(1):4. doi:10.1007/s13300-012-0004-9
- Amin N, Doupis J. Diabetic foot disease: from the evaluation of the “foot at risk” to the novel diabetic ulcer treatment modalities. World J Diabetes. 2016;7(7):153–164. doi:10.4239/wjd.v7.i7.153
- Bekele F, Chelkeba L, Fekadu G, Bekele K. Risk factors and outcomes of diabetic foot ulcer among diabetes mellitus patients admitted to Nekemte referral hospital, western Ethiopia: prospective observational study. Ann Med Surg. 2020;51:17–23. doi:10.1016/j.amsu.2020.01.005
- Pemayun TG, Naibaho RM, Novitasari D, Amin N, Minuljo TT. Risk factors for lower extremity amputation in patients with diabetic foot ulcers: a hospital-based case-control study. Diabet Foot Ankle. 2015;6:29629. doi:10.3402/dfa.v6.29629
- Schaper NC. Diabetic foot ulcer classification system for research purposes: a progress report on criteria for including patients in research studies. Diabetes Metab Res Rev. 2004;20(Suppl 1):S90–5. doi:10.1002/dmrr.464
- Noor S, Zubair M, Ahmad J. Diabetic foot ulcer–A review on pathophysiology, classification, and microbial etiology. Diabetes Metab Syndr. 2015;9(3):192–199. doi:10.1016/j.dsx.2015.04.007
- Jain A. A simple new classification for diabetic foot ulcers. Med Sci. 2015;4(2):2109–2120. doi:10.5455/medscience.2014.03.8215
- Kwon KT, Armstrong DG. Microbiology and antimicrobial therapy for diabetic foot infections. Infect Chemother. 2018;50(1):11–20. doi:10.3947/ic.2018.50.1.11
- Lipsky BA, Aragón-Sánchez J, Diggle M, et al.; International Working Group on the Diabetic Foot. IWGDF guidance on the diagnosis and management of foot infections in persons with diabetes. Diabetes Metab Res Rev. 2016;32(Suppl 1):45–74. doi:10.1002/dmrr.2699
- Lipsky BA, Berendt AR, Cornia PB, et al. Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2012;54(12):e132–73. doi:10.1093/CID/cis346
- Jneid J, Lavigne JP, La Scola B, Cassir N. The diabetic foot microbiota: a review. Human Microbiome J. 2017;5–6:1–6. doi:10.1016/j.humic.2017.09.002
- Banu A, Noorul hassan MM, Rajkumar J, Srinivasa S. Spectrum of bacteria associated with diabetic foot ulcer and biofilm formation: a prospective study. Australas Med J. 2015;8(9):280–285. doi:10.4066/AMJ.2015.2422
- Charles PG, Uçkay I, Kressmann B, Emonet S, Lipsky BA. The role of anaerobes in diabetic foot infections. Anaerobe. 2015;34:8–13. doi:10.1016/j.anaerobe.2015.03.009
- Patil SV, Mane RR. Bacterial and clinical profile of diabetic foot ulcer using optimal culture techniques. Int J Res Med Sc. 2017;5(2):496–502. doi:10.18203/2320-6012.ijrms20170139
- Najari HR, Karimian T, Parsa H, QasemiBarqi R, Allami A. Bacteriology of moderate-to-severe diabetic foot infections in two tertiary hospitals of Iran. Foot. 2019;40:54–58. doi:10.1016/j.foot.2019.05.001
- Hitam SAS, Hassan SA, Maning N. The significant association between polymicrobial diabetic foot infection and its severity and outcomes. Malays J Med Sci. 2019;26(1):107–114. doi:10.21315/mjms2019.26.1.10
- Xie X, Bao Y, Ni L, et al. Bacterial profile and antibiotic resistance in patients with diabetic foot ulcer in Guangzhou, Southern China: focus on the differences among different Wagner’s grades, IDSA/IWGDF grades, and ulcer types. Int J Endocrinol. 2017;2017:8694903. doi:10.1155/2017/8694903
- Malone M, Gosbell IB, Dickson HG, Vickery K, Espedido BA, Jensen SO. Can molecular DNA-based techniques unravel the truth about diabetic foot infections? Diabetes Metab Res Rev. 2017;33(1):e2834. doi:10.1002/dmrr.2834
- Gubta S, Mishra B, Thakur A, et al. Risk factors associated with MRSA. South African J Infect Dis. 2018;33(3):76–79. doi:10.1080/23120053.2018.1439136
- Atlaw A. Isolation of Pathogenic Bacteria and Antimicrobial Profiling Patterns Among Patients with Diabetic Foot Ulcer in Selected Hospitals in Addis Ababa, Ethiopia. [Masters thesis]. AAU Institute Repository; 2021. Availiable from: http://etd.aau.edu.et/bitstream/handle/123456789/28397.
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing. 31st ed. CLSI supplement M100. CLSI; 2022.
- Shaikh S, Fatima J, Shakil S, Rizvi SM, Kamal MA. Antibiotic resistance and extended-spectrum beta-lactamases: types, epidemiology, and treatment. Saudi J Biol Sci. 2015;22(1):90–101. doi:10.1016/j.sjbs.2014.08.002
- Jain SK, Barman R. Bacteriological profile of diabetic foot ulcer with special reference to drug-resistant strains in a tertiary care center in North-East India. Indian J Endocrinol and Metabol. 2017;21(5):688.
- Onduru OG, Mkakosya RS, Aboud S, Rumisha SF. Genetic determinants of resistance among ESBL-producing enterobacteriaceae in community and hospital settings in East, Central, and Southern Africa: a systematic review and meta-analysis of prevalence. Can J Infect Dis Med Microbiol. 2021;2021:5153237. doi:10.1155/2021/5153237
- Jain SK, Barman R. Bacteriological profile of diabetic foot ulcer with special reference to drug-resistant strains in a tertiary care center in North-East India. Indian J Endocrinol Metab. 2017;21(5):688–694. doi:10.4103/ijem.IJEM_546_16
- Oates PJ. Polyol pathway and diabetic peripheral neuropathy. Int Rev Neurobiol. 2002;50:325–392. doi:10.1016/s0074-7742(02)50082-9
- Saltoglu N, Ergonul O, Tulek N, et al.; Turkish Society of Clinical Microbiology and Infectious Diseases, Diabetic Foot Infections Study Group. Influence of multidrug resistant organisms on the outcome of diabetic foot infection. Int J Infect Dis. 2018;70:10–14. doi:10.1016/j.ijid.2018.02.013
- Adeyemo AT, Kolawole B, Rotimi VO, Aboderin AO. Multicenter study of the burden of multidrug-resistant bacteria in the etiology of infected diabetic foot ulcers. Afr J Lab Med. 2021;10(1):1261. doi:10.4102/ajlm.v10i1.1261
- Akhi MT, Ghotaslou R, Asgharzadeh M, et al. Bacterial etiology and antibiotic susceptibility pattern of diabetic foot infections in Tabriz, Iran. GMS Hygiene Infect Control. 2015;10. doi:10.3205/dgkh000245
- Ismail AA, Meheissen MA, Elaaty TAA, Abd-Allatif NE, Kassab HS. Microbial profile, antimicrobial resistance, and molecular characterization of diabetic foot infections in a university hospital. Germs. 2021;11(1):39–51. doi:10.18683/germs.2021.1239
- Mama M, Aklilu A, Misgna K, Tadesse M, Alemayehu E. Methicillin- and inducible clindamycin-resistant Staphylococcus aureus among patients with wound infection attending Arba Minch Hospital, South Ethiopia. Int J Microbiol. 2019;2019:2965490. doi:10.1155/2019/2965490
- Gary EY, Gebreab YB, Archila OO, et al. Methicillin-resistant Staphylococcus aureus (MRSA): prevalence and antimicrobial sensitivity pattern among patients-a multicenter study in Asmara, Eritrea. Can J Infect Dis Med Microbial. 2019;8321834. doi:10.1155/2019/8321834
- Ahmed EF, Gad GF, Abdalla AM, Hasaneen AM, Abdelwahab SF. Prevalence of Methicillin resistant Staphylococcus aureus among Egyptian patients after surgical interventions. Surg Infect. 2014;15(4):1–6. doi:10.1089/sur.2013.212
- Abdalla AE, Kabashi AB, Elobaid ME. Methicillin and inducible clindamycin-resistant Staphylococcus aureus isolated from postoperative wound samples. J Pure Appl Microbiol. 2019;13(3):1605–1609. doi:10.22207/JPAM.13.3.33
- Dwedar, R., Ismail, D. K. & Abdulbaky, A. 2015. Diabetic foot infection: microbiological causes with special reference to their antibiotic resistance pattern. The Egyptian Journal of Medical Microbiology, 38;3174, 1–8.