Abstract
Background
Bloodstream infections (BSIs) are significant causes of morbidity and mortality in Ethiopia and worldwide. Alarming is the rapid global spread of antimicrobial resistance (AMR) in bacteria.
Objective
To determine the microbial profile, antimicrobial susceptibility pattern, and associated risk factors for bloodstream infections in Tikur Anbessa Specialized Hospital (TASH) Addis Ababa Ethiopia.
Methods
A cross-sectional study was conducted between September 2018 and March 2019. Blood collected twice from each septicemia suspected patient were processed following standard bacteriological procedures. AST was performed by using the disk diffusion test according to CLSI 2017 and 2018 guidelines. Data captured in Epidata were cleaned and analyzed by SPSS version 21 software.
Results
The prevalence of BSI was 28.06% and a higher proportion of pathogene detected were gram-negative bacteria (GNB) (54.5%) and gram-positive bacteria (GPB) (45.43%). The most abundant bacterial species were Klebsiella pneumoniae 17.6%, CoNS 15.2%, and Acinetobacter spp 11.0%. Culture positivity was associated with age below 6 years, neonates AOR p=<0.001, infants AOR p=<0.001, Pre-school P=0.002, ICU admission COR p=<0.001, length of admission >5 days COR P=0.016, temperature greater than 38°C, AOR p=0.013, instrument usage during medical care AOR, p=<0.001, chronic illness AOR p=0.027, and neonatal incubation AOR p=0.013. GNB average drug resistance rate was 57.9% of the commonly used antibiotics and the most efficient and inefficient drugs were amikacin (10.8%) and ampicillin (94.6%). The gram-negative isolates showed a 95.3% rate of multi-drug resistance; and MDR, XDR, and PDR were observed at 55.8%, 32.2%, and 7.3%, of isolates respectively. This finding shows children especially neonates were highly affected by drug resistant BSI.
Conclusion
Pediatric patients and ICU patients are more affected by BSI, and drug-resistant bacteria are a major problem. Therefore, appropriate intervention approaches need to be implemented.
Introduction
Bloodstream infections (BSI) are infectious diseases defined by the existence of viable microorganisms in the bloodstream, which are later confirmed by the positivity of one or more blood cultures.Citation1 It is an important cause of morbidity and mortality worldwideCitation2,Citation3 and is of great impact on health care operations.Citation4 It is a preventable infection but the leading cause of complication in critically ill patients.Citation5 Globally, Hospital Acquired Infections (HAIs) are the most frequent adverse event to occur during hospitalization.Citation9 BSI represents about 15–20% of all nosocomial infections and affects approximately 1% of all hospitalized patients.Citation10
In Sub-Saharan countries, including Ethiopia, BSI in children, a mortality rate approaching 53%.Citation13,Citation14 Studies conducted in Ethiopia from septicemia suspected cases the prevalence of BSI showed 18.2% in Gonder,Citation14 28% in Mekelle,Citation16 39.2% in Bahir Dar,Citation17 15.8% in Jimma,Citation18 27.9% and 13.% in Addis Ababa.Citation19,Citation20 Depending on the risk factors, the mortality rate varies between 4.0% and 41.5%.Citation6 Patients with positive blood culture had a fivefold higher death rate than those without bacteremia ie, 50.0% as compared to 9.8% which is the case of those without bacteremia.Citation20
There are several known risk factors for BSI these include immuno-suppressive conditions such as malnutrition, environmental exposures, ICU stay, the prevalence of specific nosocomial pathogens, surgery, invasive devices and procedures, mechanical ventilation, and dialysis, and disruption of anatomical barriers following central vein catheter (CVC) insertionCitation5,Citation21–23 increased age and length of hospital stay, impaired conscious levels, and steroid therapy inadequate and untrained health care personnel may cause contamination leading to BSIs.Citation24 Secondary infections such as urinary tract infections (UTI), surgical wound infections (SWI), gastrointestinal tract infections (GII), lower respiratory infections (LRI) peritonitis, malignancies, and skin infectionCitation2,Citation3,Citation12,Citation25 increases the risk of acquiring BSI.
Antimicrobial resistance (AMR) is a global health and development threat. It requires urgent multisectoral action. The World Health Organization (WHO) has declared that AMR is one of the top 10 global public health threats facing humanity.Citation26 Alarming is the rapid global spread of multi-resistant bacteria that cause common infections and resist treatment with existing antimicrobial medicines.Citation27–29 During the past decades, a shift in the multidrug-resistant (MDR) dilemma has been noted from gram-positive to gram-negative bacteria, due to the scarceness of new antimicrobial agents.Citation11 In this study multidrug-resistant (MDR), extensively drug-resistant (XDR), and pandrug-resistant (PDR) classifications were done according to Magiorakos’s definition.Citation30 These AMR in a wide range of infectious agents is a growing public health threat and concern of health care management.Citation27 Therefore, updated information regarding etiological agents of BSI and their antimicrobial susceptibility patterns is crucial for empirical treatment success. In this regard, continuous assessment of the antibiogram profile is crucial to track changes in etiological agents and antimicrobial susceptibility patterns.
This study was carried out to determine the prevalence of bloodstream infections, microbial profiles and their anti-microbial susceptibility patterns, and associated risk factors at Tikur Anbessa Specialized Hospital.
Materials and Methods
Study Design, Study Area, Study Population, and Sample Size
Cross-sectional studies were conducted from September 2018 up to Mar 11, 2019, in Tikur Anbessa Specialized Hospital (TASH) which is the largest teaching and specialized hospital in Ethiopia, with over 700 beds and serve as the teaching center for undergraduate and postgraduate medical students, and medical-related fields.Citation31 Inpatients from all age groups hospitalized in each ward and outpatients suspected of bloodstream infection and who are willing to participate in the study were included. The conditions of sepsis definitions were established by the 1991 Consensus Conference, which was updated in 2001.Citation32,Citation33 The multidrug resistance, extensive drug resistance, and pan drug resistance categories were used by the consensus definitions proposed by Magiorakos.Citation30 The sample size calculation is based on a single sample size estimation.Citation34,Citation35 The prevalence of 32.8% was taken from the study conducted in Addis Ababa Ethiopia.Citation36 ,
=1354.80 with 10% contingency = 1490. Data on Socio-demographic characteristics and medical information were collected by trained nurses and laboratory technicians.
Blood Culture and Antimicrobial Susceptibility Test
Duplicate blood samples were collected aseptically from patients for routine blood culture and in the case of coagulase-negative staphylococci (CoNS), similar growth in both bottles was considered positive in addition to essential clinical criteria. About 1–4 mL of blood for pediatrics (less than 12 years) and 5–10 mL of blood for adults (greater than 12 years) were inoculated into a ready-made.Citation37 BacT/ALERT blood culture bottle containing Antimicrobial neutralizing bottles with adsorbent polymeric beads were used.Citation38 Blood culture bottles were incubated in an automatic BacT/ALERT® 3D machine at 37°C of 5% CO2 gas concentration and were inspected daily for the sign of bacterial growth for up to 5 days.Citation38,Citation39 Turbid blood samples from the blood culture bottle were sub-cultured on blood agar (Oxoid, England) (5% sheep blood plates), and chocolate (Oxoid, England), in microaerophilic condition (containing 5% CO2) and MacConkey agar (BD, USA), agar in aerobic conditions at 37°C for 24 hours.Citation40 Bacterial pathogens were identified using standard bacteriological procedures.Citation41 A positive culture from blood samples was characterized by gram stain and further classified at the species level by using biochemical tests.Citation42
Each isolate was spread onto a Mueller–Hinton agar plate. The antimicrobials for disc diffusion testing were obtained from BD and Oxoid in the following concentrations: GNB Ampicillin (AM) (10 µg), Amoxicillin + clavulanic acid (AMC) (20/10µg), Ampicillin – Sulbactam (SAM) (10/10 µg), Piperacillin – Tazobactam (TZP) (100/10µg), Cefotaxime – clavulanate (CTL) (30/20µg), Ceftazidime – clavulanate (CAL) (30/10 µg), Cefotetan (CTT) (30 µg), Cefepime (FEP) (30 µg), Ceftazidime (CAZ) (30 µg), Cefotaxime (CTX) (30 µg), Ceftriaxone (CRO) (30 µg), Cefuroxime (CXM) (30 µg), Ceftaroline (CPT) (30 µg), Imipenem (IMP) (10 µg), Meropenem (MEM) (10 µg), Dorsapenem (DOR) (10 µg), Ertapenem (ETP) (10 µg), Amikacin (AN) (30 µg), Tetracycline (TET) (30 µg), Minocycline (MIN) (30 µg), and Levofloxacin (LEV) (5 µg), were used Cefoxitin (FOX) (30 µg), Trimethoprim-Sulfamethoxazole (SXT) 1(0.25/23.75 µg), Gentamicin (GM) (10 µg), Tobramycin (NN) (10 µg), Ciprofloxacin (CIP) (5 µg), Doxycycline (DOX) (30 µg), Azithromycin (ATM) (30 µg), and Chloramphenicol (C) (30 µg) were used.Citation41 Resistance and susceptibility were interpreted according to the CLSI Laboratory Standards.Citation41 Escherichia coli (ATCC 25922), Staphylococcus aureus (ATCC 25923), and Pseudomonas aeruginosa (ATCC 27853) were used as reference strains for culture and susceptibility testing.
Statistical Analysis and Interpretation
All the data captured in Epi-data were cleaned and analyzed by using SPSS version 21 software for further analysis. The quantitative data collected using different techniques were analyzed using simple descriptive statistics, analyzed using Chi-square, correlation, Univariate (binary) logistic regression, and multiple linear regression model. Variables that showed a significant association with univariate logistic regression analysis were analyzed using multivariate logistic regression models. A p-value < 0.05 was statistically significant and the strength of the association was interpreted using an odds ratio in a 95% confidence interval.
Ethical Clearance
This study was approved by the “College of Natural and Computational Sciences Institutional Research Ethics Review Board (CNS-IRB) on 30/03/2018 minute no IRB/032/2018 at Addis Ababa University.” Permission was obtained from the study site by; the College of Health Science Institutional Review Board (IRB). This study procedure fulfilled the requirements of the declaration of Helenski. For participants whose age is below 18 years, we have collected assent (12–18) and consent from the patient legal guardians but in cases above 18 years, we have collected consent from the patients. The purpose and procedures of the study were explained to the study participant’s parents or guardians during the study and patient results were communicated to the attending physicians.
Results
Study Population (Socio-Demographic Characteristics)
In this study, a total of 1486 patients suspected of bacteremia were included. Among the recruited patients 844 (56.8%) were males and 642 (43.2%) were females with a ratio of 1.3:1. The age range of the patients was from 1 day to 91 years with a mean age of 18.24 and a standard deviation of 20.5; 433 (29.14%) were below 2 years. The majority of them were in-patient, 1483 (99.1%), and the rest, 13 (0.9%), were outpatients. The frequent blood culture request was from Casualty Ward (C/W) 353 (23.8%), Emergency outpatient department (EOPD) 222 (14.9%), and neonatal ICU 195 (13.1%). Majority of participants regarding their departments were from Medical 728/1486 (48.99%), Hematology 306/1486 (20.59%), and NICU 178/1486 (11.98%).
Blood Culture
The overall culture-positive result among the patients was 417/1486 (28.06%), and ten of them were found with double bacterial infections in which the total bacterial isolates were 427. Among the total of 427 bacterial strains, 233 (54.57%) were Gram-negative and 194 (45.43%) were Gram-positive. Among the gram-negative isolates, Klebsiella pneumoniae accounted for 75 (17.56%), Acinetobacter spp 47 (11.01%), and Escherichia coli 38 (8.9%) were the dominant ones. Among 191 gram-positive isolates, the predominant strain was CoNS, 65 (15.22%), followed by Staphylococcus aureus 44 (10.3%), Enterococcus spp 24 (5.62%) as shown ().
Table 1 Bacterial Isolates from BSI Patients at TASH
Factors Associated with Positive Blood Culture
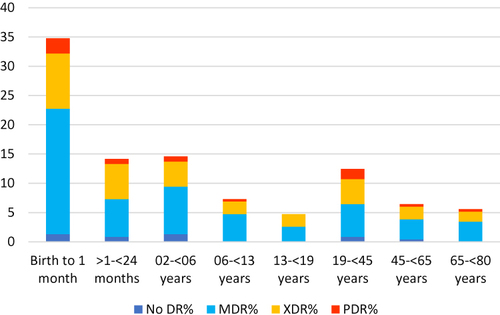
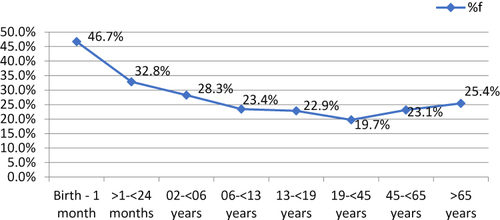
Prevalence of positive blood culture results against the age of participant showed the increased trend at very young age as shown in and the difference in prevalence is associated with age as shown by the adjusted odds ratios for different age groups; birth to one month p ≤ 0.001; greater than 1 month up to less than 24 months, p ≤ 0.001; and two years up to less than six years, p = 0.002, (). An increased trend of positivity was also shown at old age (>45 years); however, the difference was not statistically significant.
Table 2 Socio-Demographic Characteristics and Clinical History of BSI Suspected Patients with Blood Culture-Positive Results Crude and Adjusted Odds Ratio at TASH
Figure 1 Proportion of bacterial identification among the age of the participant in BSI suspected patients at Tikur Anbessa Specialized Hospital.
We analyzed if there was a difference in the type of pathogen isolated with age, as shown in K. pneumoniae 33% was the predominant pathogen isolated from neonates followed by K. oxytoca 15.17% and Acinetobacter spp. 11.6%.
Figure 2 Distribution of bacterial isolated with age category from BSI suspected patients Tikur Anbessa specialized Hospital.
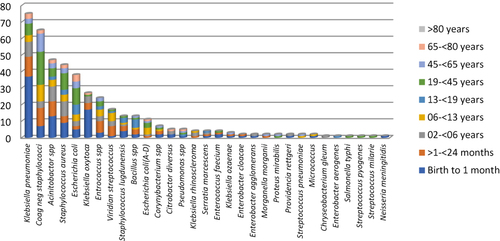
In the age group of >1–<24 months the most prevalent bacteria were again K. pneumoniae 17.39% CoNS 15.9%, and Acinetobacter spp 13%. In the age group of 2–<6 Klebsiella pneumoniae, Acinetobacter spp, and Staphylococcus aureus was the most predominant. Another trend we observed in terms of pathogens isolated is the rate of CoNS 30.7% in adult. A larger proportion of the CoNS were isolated from the age group 19–45 years. In the case of those above 65 years the most prevalent bacteria were E. Coli 24%, K. pneumoniae 18%, and CoNS 12%, ().
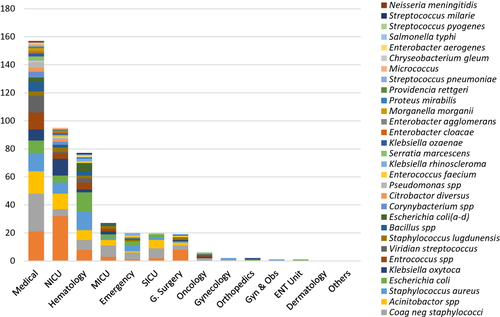
In this study, the top five departments of the blood culture request were from the internal medicine followed by hematology, NICU, MICU, and ER. However, the highest rate of isolation was observed in SICU about 20 (59%) AOR p=<0.001, NICU 91 (51%) AOR p=0.002, General surgery 18 (39.1%) AOR P=0.044, ICU 25 (34.2%) COR p=0.013, and Emergency 19 (26.8%) AOR P=0.024 (). , shows the different types of pathogens isolated from the different departments, and the type of pathogen isolated was also different among the patient attending wards ().
Figure 3 Bacterial isolates and their frequency in patient admission ward from blood culture of BSI suspected patients at Tikur Anbessa Specialized Hospital.
Another factor that is associated with positive blood culture test is the length of stay in the hospital (). In our study, although bivariate analysis has shown an increased trend of positivity following a longer stay multivariate analysis did not show a significant difference in the length of stay in the hospital for positive blood culture results as shown in .
Figure 4 Length of hospital stays with culture positivity of patients from BSI patients in Tikur Anbessa Specialized Hospital.
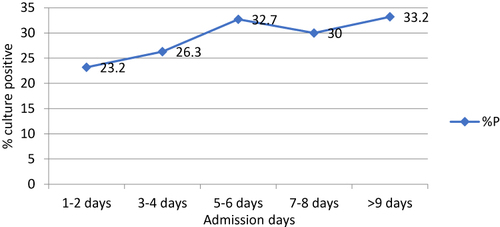
Other medical care factors like ICU admission COR p=<0.001, use of instrument AOR p=<0.001, nasogastric intubation (NG tube) AOR p=<0.042, and incubation AOR p=<0.013 for pediatrics as well as patient factors such as being febrile; having chronic illness AOR p=0.027; wound, urinary tract or respiratory tract infections; were assessed and almost all were shown to be associated with blood stream infections as shown in ().
Antimicrobial Resistance Pattern of the GNB Isolates
Among the total 26 commonly used antibiotics against GNB 25 for Enterobacteriaceae, 16 for Acinetobacter, and 12 for Pseudomonas were used for AST test according to CLSI 2018 standard. Excluding Neisseria meningitidis and Chryseobacterium gleum from the total 17 GNB, 9 of them were resistant to more than 50% of commonly used antibiotics. The percentage of drug resistance of GNB from commonly used antibiotics was S. marcescens accounts 52/76 (68.4%), Acinetobacter spp 489/750 (65.2%), K. pneumoniae 1152/1797 (64.1%), E. coli (A-D) 165/274 (60.2%), E. cloacae 21/38 (55.3%), K. oxytoca 370/675 (54.8%), E. coli 519/950 (54.6%), K. rhinoscleromatis 53/100 (53.0%), M. morganii 22/44 (50.0%), P. mirabilis 23/48 (47.9%), P. Rettgeri 16/44 (36.4%), C. Diversus 45/125 (36.0%), E. aerogenes 6/19 (31.6%), K. ozaenae 23/75 (30.7%), Pseudomonas spp 15/60 (25.0%), E. agglomerans 12/50 (24.0%), and S. typhi 0/25 (0.0%).
Ampicillin was the most resisted drug, 88/93 (94.6%), whereas Amikacin, 25/231 (10.8%), was the least resisted (). It shows S. mercensus, 100% resistant for CTX, CRO, CAZ, ATM, and 75% for FEP. Acinetobacter spp were resistant to CTX, FEP, and CAZ, accounts 91.5%, 89.4%, 76.6%, and 68.1% respectively. K. pneumoniae were resistant to CTX, CRO, FEP, and CAZ account for 93.3%, 94.7%, 92%, and 92%. E. coli were 81.1% resistant to CTX, and 81.8% for CRO, FEP, CAZ. K. oxytoca resistant to CTX 85.5%, CRO 77.8%, FEP 85.2%, CAZ 66.7% and E. coli (A-D) resistant to CTX 71.1%, CRO 73.7%, FEP 65.8%, CAZ 68.4%.
Table 3 Gram-Negative Bacteria and Their Percentage Drug Resistance from Isolates of BSI Patients at TASH
Among the WHO global priority list Carbapenem-resistant Acinetobacter spp were about 30 (63.8%), Carbapenem-resistant Pseudomonas spp were 40% (2/5), Carbapenem-resistant K. pneumoniae were about 20 (26.7%), 3rd generation cephalosporin-resistant K. pneumoniae were 71 (94.7%), Carbapenem-resistant E. coli were 7 (18.4%); and 3rd generation cephalosporin-resistant E. coli 28 (73.7%).
Multidrug Resistance and Their Risk Factors in GNB
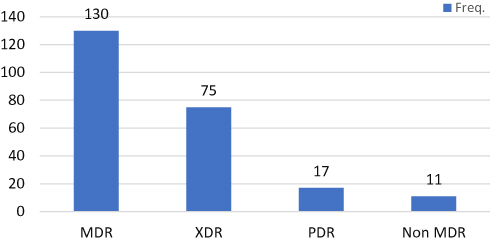
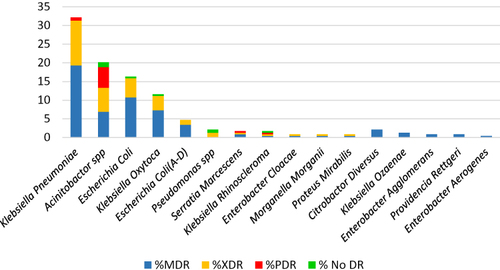
In this study, gram-negative MDR organisms were highly prevalent. As shown in among 233 gram-negative organisms, 222 (95.3%) were MDR and above MDR, and 11 (4.7%) were not. Of the total gram-negative organisms, 130 (55.8%) were MDR, 75 (32.2%) were XDR, and 17 (7.3%) were PDR.
Figure 5 Antibiotic treatment before 5 days and after 5 days versus culture positive result in Tikur Anbessa Specialized Hospital.
When we looked at the type of pathogens that were either MDR or XDR the large majority of them were Klebsiella pneumoniae, Acinetobacter spp, Escherichia coli, Klebsiella oxytoca as shown in (). The large majority of PDR pathogens were Acinetobacter.
Figure 6 MDR category of BSI suspected patients gram-negative isolates from Tikur Anbessa Specialized Hospital.
The highest percentage of drug resistance was found in neonates and children. Among the total drug resistance bacteria, 148 (66.67%) of them were identified in patients below six years, and from the total of 17 PDR, bacteria 35.29% of them were from the age of <28 days (). This finding shows children especially neonates were highly affected by drug-resistant bacteria.
Discussion
The study result showed microbial profile, antimicrobial susceptibility pattern, and associated risk factors of bloodstream infections caused by GNB in relatively large number of patients. This may help in the management of potentially life-threatening infections caused by MDR organisms in the health care services.
The overall prevalence of culture-positive results in this study, 28.06%, was comparable with the study done in Mekelle, Ethiopia, 28%,Citation16 in Addis Ababa Ethiopia, 27.9%,Citation19 in Weldia, Ethiopia, 25.78%,Citation43 and Athens, Greece, 29%.Citation44 However, the current prevalence is lower than the study done in Addis Ababa, Ethiopia, 40.2%,Citation45 in Bahir Dar, Ethiopia, 39.2%,Citation17 and in Addis Ababa, Ethiopia, 32.8%.Citation36 On the other hand, the current finding is higher than the study done in Addis Ababa, Ethiopia, 20.8%,Citation15 Gonder, Ethiopia, 18.2%,Citation14 and Malawi 30%.Citation46 It is also higher compared to reports from other countries such as Nepal 16.2%,Citation47 Tanzania 13.9%,Citation48 Ghana, 13.08%,Citation49 Iran 11.9%Citation50 and in Atlanta, USA, 11%.Citation51 Meta-analysis data shows in Africa and Asia 19.1 (95 CI: 12.0–27.5); in Africa 15.5 (8.4–24.4) and in Asia 28.0 (13.2–45.8).Citation52 The possible explanation for the lower and higher prevalence compared with other studies could be due to differences in the study population, study design, geographical location, etiological agents, patient clinical case, seasonal variations, and differences in infection prevention policies and implementation between countries and institutions.
The higher involvement of GNB 54.57%, than GPB 45.43%, in BSI, detected in the current study is similar to previous reports from Addis Ababa, Ethiopia,Citation19,Citation45 and Bahir Dar, Ethiopia.Citation15,Citation17 The difference could be due to the greater tendency of Gram-negative organisms in becoming a major drug-resistant cause of nosocomial infections.Citation11 Unlike this study, a lower prevalence was recorded for GNB than for GPB.Citation16,Citation18,Citation36
Among the different gram-negative bacteria, Klebsiella pneumoniae accounted for 75 (17.56%), Acinetobacter spp 47 (11.01%), Escherichia coli 38 (8.9%), Klebsiella oxytoca 27 (6.32%), and Escherichia coli (A-D) 11 (2.58%) were the predominant isolates. This study has similar findings to a study done in Addis Ababa and Ethiopia.Citation17,Citation45
In this study, there was no significant difference between being males 240 (28.3%) and female 185(28.5%) p=0.916 (0.79–1.24) on positivity rate for blood culture results. This finding is in line with the study done in Ethiopia,Citation19 and Nigeria.Citation54
However, a significant association of bacterial growth with patient age was found in this study comparable with studies done in Ethiopia.Citation14,Citation19,Citation36,Citation55 In Africa Ghana shows under 5 ages, the highest bacteremia were recorded.Citation49 Again, in the US severe sepsis occurs more frequently in infants and elderly individuals than in other age groups.Citation4 Similar findings were observed in the study of all age groups in Tanzania.Citation56 From this study, we can understand that the small age groups are more affected by bacterial bloodstream infection. These predominant bacteria are known to cause nosocomial infection in children less than two years.Citation9 The more we go from preschool to neonates in TASH setting the infection rate increases, probably this could be due to the immaturity of their immune system, contamination due to high workload, length of admission, loosen IP protocol, and the optimal temperature for bacterial growth along with crowdedness of neonatal ICU, were the possible reasons. Therefore, due to their susceptibility, health care institutions serving pediatric patients should give special attention to nosocomial infections, and a strong infection prevention protocol should be implemented.
Among admission wards, NICU, MICU, and PEOPD have a high association with bacterial growth. A study done on TASH shows a high rate (44.7%) of positive blood cultures (reported in NICUCitation19,Citation57 and MICU).Citation45 Identification of bacteria in admission wards shows that K. pneumoniae has been identified abundantly from NICU, C/W, and MICU respectively. CoNS were identified from MICU, C/W, and EOPD. The need to report CoNS or not has been a discussion point and in our settings, we Report CoNS only when their isolation is consistent with the clinical findings. Acinetobacter spp was identified from NICU, C/W, and B4.Citation58 In this regard, NICU, and C/W, are highly affected by Klebsiella pneumoniae, Klebsiella Oxytoca, and Acinetobacter spices.Citation57,Citation59
Like wards, we analyzed the association of culture-positive results with departments where the medical service is given. Univariate and multivariate logistic regression analysis show SICU, NICU, General Surgery, MICU, and both Pedi and adult Emergency show strong statistical association with the culture-positive result. Several factors could account for this, the patient attending ICUs have a higher risk of acquiring such infections because of their being immune-compromised, higher incidence of outbreaks, and use of the invasive device that provides access for pathogen entry to BSI. A study done in Tanzania shows patients admitted to ICU had a higher incidence of BSI and surgical wards and ICUs have an increased risk of mortality.Citation56 Prolonged hospital stays greater than five days have an association with positive blood culture. Similarly, a study in Egypt showed a stay greater than one week,Citation8 in Ghana greater than one weekCitation60 in TurkeyCitation61 and Italy longer ICU stay >19.5 days has associated with Nosocomial infection.Citation62 The variation could be their health care IP protocol and implementation.
Among departments, bacterial identification in NICU K. pneumoniae, K. oxytoca, and Acinetobacter spp were found in high numbers compared with other bacteria whereas, in G. Surgery K. pneumoniae, CoNS, Acinetobacter spp, and S. Lugdunensis and in Emergency CoNS, S. aureus, and E. coli were found abundantly. In SICU and MICU shows Acinetobacter spp, K. pneumoniae, CoNS, and E. coli were found abundantly in addition to S. aureus in SICU. In general K. pneumoniae, CoNS, and Acinetobacter spp, were found predominantly in ICU and surgeryCitation58 in Leal study similar results were found except for CoNS.Citation63 Therefore, intervention on fumigation, minimizing patient load, and strong infection prevention protocol should be implemented focusing on above-mentioned wards and departments.
Among the total culture-positive patients, 67.6% of them have acquired bloodstream infections after three days of admission, due to the admission other than BSI clinical diagnosis. Length of admission greater than five days in General Surgery, SICU, and MICU shows 71.7%, 67.6%, and 67.1% percentage culture-positive results respectively. The similarity of organisms identified from EOPD, MICU, NICU, SICU, and general surgery shows that nosocomial infection is the major source of BSI in the hospital. Due to different mentioned factors ICU patients are vulnerable to nosocomial infection.Citation7,Citation8,Citation11,Citation62
In this study Body temperature greater than 38°C have an association with positive blood culture. This finding is in line with a study in Thailand.Citation64 Usage of medical instrumentation or indwelling medical devices during medical care has an association with positive blood culture. Studies were done on the peripheral intravenous devices and any surgery in Arba Minch,Citation65 on catheters and central venous lines in Gonder,Citation55 mechanical ventilation, and extracorporeal membrane oxygenation in ItalyCitation62 intravenous line in EgyptCitation8 invasive procedures in TurkeyCitation61 have statistically significant for BSI.
Having a history of chronic illness is one of the factors of BSI. Similar results were found in the study of Endris in Ethiopia.Citation55 Among chronic illnesses; wound infection, ureteral tract infection, and respiratory tract infection was associating factors for BSI. These results are in line with the study done in Finland on wound infection.Citation7 In this case, chronic illness causes depletion of the patient immune status, increased length of admission, and exposure to different medical devices can cause a high chance of acquiring nosocomial infection.
Among neonates, a history of incubation in NICU was a factor associated with positive blood culture. Review result in developing countries shows neonatal infections were 3–20 times higher in hospital-borne babies.Citation66 Similarly in the US NICU was a risk factor for neonatal BSI.Citation67 As long as our hospital is in developing countries, we expect similar results to Zaidi’s findings. This is because sharing limited resources of medical instruments, crowdedness, humidity, and optimal temperature for bacterial growth in NICU wards were aggravating factors for nosocomial infection.
In this study educational level of the family, place of delivery, mode of delivery, Prolonged rupture of membranes, history of maternal fever, and neonatal body weight during delivery do not have an association in logistic regression with positive blood culture. Among all selected antibiotics for gram-negative bacteria antimicrobial susceptibility test, the isolates were resistant to 57.9% of the drug tested, and more than half of bacteria have resisted the antibiotics above 72.7%. In terms of the pathogens isolated Serratia marcescens 52/76 (68.4%) and Salmonella typhi 0/25 (0.0%), the highest and lowest bacteria resistant to the drugs tested even though their rate of isolation is lower n < 5 compared to other pathogens. Whereas among the common pathogens isolated, Acinetobacter spp, K. pneumoniae, and E. coli (A-D) were resistant to commonly used antibiotics at the rate of 65.2%, 64.1%, 60.2% respectively. The top drug resistance was observed against Ampicillin 88 (94.6%) followed by Tetracycline 94.3%, and Ampicillin–Sulbactam 94.1%. and the list was against Amikacin 25 (10.8%) followed by Ertapenem 21.2%, and Cefotetan 23.8%. Almost similar resistance findings were reported from Jimma against Ampicillin, cephalothin, and tetracycline accounting 85.7%, 71.4%, and 71.4% respectively.Citation18 In our country, Amikacin is one of Anti TB treatments. It is reserved for RR/MDR-TB treatment and not used for routine purposes, it is still one of the most effective drugs against similar pathogens reported by.Citation68 Another study was done in Ethiopia also showed Amikacin has similar efficacy against Enterobacteriaceae 13.8% and K. pneumoniae 21.3%.Citation69,Citation70 Our study and similar findings by others show the importance of the implementation of antibiotic stewardship in Ethiopia. The highest number of resisted drugs by non-fermenter bacteria were Cefotaxime 91.5%, Ceftriaxone 89.4%, Doxycycline 87.2%, and the lowest number of resisted drugs by non-fermenter bacteria were Amikacin 34.6%, Levofloxacin 36.5%, and Imipenem 46.2%. Among the total gram-negative bacteria, the highest Amikacin-resistant bacteria were Acinetobacter spp accounts 38.3% but still less resistance compared with other non-fermenter drugs. Study done In India, on ICU instruments all Acinetobacter baumanii, were resistant to Amikacin.Citation53 Highly susceptible drug Cefotetan was resistant 25.3% to K. pneumoniae and 31.6% to E. coli (A-D) other bacteria were below 18.2%.
Among gram-negative bacteria, S. marcescens, K. pneumoniae, E. coli (A-D), Acinetobacter spp, K. oxytoca, and E. coli were in average resistant to 93.8%, 93.0%, 81.6%, 81.4%, 78.8%, and 69.8% for cephalosporin (Cefotaxime, Ceftriaxone, Cefepime, Ceftazidime) drugs. K. pneumoniae had the highest number of carbapenem-resistant bacteria with a rate of resistance to Dorsapenem 26.7%, Meropenem 20% Imipenem 22.7% next to Acinetobacter, with Dorsapenem 63.8%, Meropenem 59.6%, and Imipenem 46.8%. These organisms are the known cause of nosocomial infection and acquire drug-resistant genes from surrounding organisms by different mechanisms. A study done in India shows that >80% K. pneumoniae and E. coli were resistant to commonly used antibiotics.Citation53 Therefore, reducing bacterial colonization in the health care setup means reducing the occurrence of nosocomial infection and drug-resistant organisms.Citation8,Citation22,Citation53
In this study, MDR organisms were predominant. Among gram-negative bacteria, 95.3% were multi-drug resistant and only 4.7% were not. Among the total drug-resistant gram-negative organisms MDR, XDR, and PDR accounted for 55.8%, 32.2%, and 7.3% respectively. A study was done in Jimma also showed similar findings among GNB 80% P=0.438 of them were MDR and above,Citation18 and in Gaza, Palestine, and Addis Ababa, 92.7% were MDR and above.Citation19,Citation71 This is worrisome to ICU patients treating physicians. Lesser rate amount was observed in Tanzania from nosocomial infection 70.5% of isolates were MDR.Citation56 In Italy, 56% of MDR,Citation62 and in Egypt 52% of MDR was identified.Citation8 Among the 17 total PDR bacteria isolated, Acinetobacter spp accounts for 76.47%, and K. pneumoniae accounts for 11.76% the rest of each account 5.88%. Among 13 PDR Acinetobacter, 9(52.9%) of them were isolated from B4 (MICU) and B6 (NICU) account for 5(29.4%) and 4(23.53%) respectively Other studies showed similar findings neonatal and pediatric ICUs were more affected by PDR Acinetobacter species.Citation72,Citation73
K. pneumoniae, Acinetobacter spp, E. coli, K. oxytoca, and E. coli (A-D) were the most prevalent multi-drug resistance bacteria isolates in our study. Drug resistance with age category shows that the highest percentage of drug resistance is found in neonates and children. Among the total of 222 drug resistance bacteria, 66.67% of them were identified in patients below six years. The highest amount of the pathogens isolated in the age group of birth to <1 month 81 (36.49%), >1–<24 months 33 (14.86%), and 02–<06 years 34 (15.32%). Of the total 17 PDR, 35.29% of them were found in the age of 1 day–<28 days. This finding shows children were highly affected by drug-resistance bacterial and bloodstream infections in our study and similar findings were also reported elsewhere.Citation74
MDR distribution in the admission ward shows that B6 (NICU), C/W, and B4, were the top three most affected wards that account for 75 (32.19%), 36 (15.45%) 25 (10.73%) by drug-resistant bacteria. This result demonstrates that hospital pediatric patients are more affected by drug-resistant bacterial bloodstream infections.Citation75 Usage of Indwelling medical devices has exposure to multidrug resistance bloodstream infection. History of incubation has exposure to MDR bacterial infection.
Conclusion
In conclusion, the study determined the prevalence of BSI among septicemic patients and the most abundant bacteria and their susceptibility pattern. Our findings showed both GNB and GPB cause BSI. The most common bacteria isolated include K. pneumoniae, CoNS, Acinetobacter spp, S. aureus, and Escherichia coli. Like, in the other part of the world the isolates were highly resistant to commonly prescribed antibiotics and their rate of resistance against carbapenem is alarming. Among the factors associated with BIS infection age, ICU admission, indwelling medical devices, and chronic illness were the most important. In the neonate, incubation has the most significant association with bloodstream infection. Individuals below 6 years old were more vulnerable to bacterial bloodstream infection. Special attention and intervention are needed for neonatal and pediatric patients that are more affected by drug-resistant bacterial bloodstream infections.
Abbreviation
AMR, Antimicrobial resistance; AST, Antimicrobial susceptibility tests; BSI, Blood Stream Infection; CVC, Central Vein Catheter; GII, Gastrointestinal Tract Infection; GNB, Gram-negative bacteria; GPB, Gram-positive bacteria; HABS, Hospitals acquire bloodstream infection; HAI, Hospital Acquire Infection; HCAI, Health Care Acquire Infection; ICU, Intensive Care Unit; IP, Infection Prevention; NICU, Neonatal Intensive Care Unit; LRI, lower respiratory infections; MDR, Multi-drug resistance; PDR, Pan drug-resistant; SWI, Surgical Wound Infections; TASH, Tikur Anbessa Specialized Hospital; UTI, Urinary Tract Infections; XDR, Extensively drug-resistant.
Disclosure
The authors declare no conflicts of interest in relation to this work.
Acknowledgments
The authors would like to acknowledge Addis Ababa University College of Health Sciences Tikur Anbessa Specialized hospital for sponsorship and facilitation to do research in the microbiology laboratory. Addis Ababa university college of natural and computational science microbial cellular molecular biology infection biology stream for teaching coaching and mentorship.
Additional information
Funding
References
- Viscoli C. Bloodstream infections: the peak of the iceberg. Virulence. 2016;7(3):248–251. doi:10.1080/21505594.2016.1152440
- Timsit JF, Soubirou JF, Voiriot G, et al. Treatment of bloodstream infections in ICUs. BMC Infect Dis. 2014;14(1):489. doi:10.1186/1471-2334-14-489
- Gaynes R, Band J. Epidemiology, pathogenesis and microbiology of intravascular catheter infections. UpTo Date versión; 2009.
- Martinez RM, Wolk DM, Hayden RT, Wolk DM, Carroll KC, Tang Y-W. Bloodstream infections. Microbiol Spectrum. 2016;4(4). doi:10.1128/microbiolspec.DMIH2-0031-2016
- Hugonnet S, Sax H, Eggimann P, Chevrolet J-C, Pittet D. Nosocomial bloodstream infection and clinical sepsis. Univ Geneva Hospitals. 2004;10(1):76.
- Ahmed D, Nahid MA, Sami AB, et al. Bacterial etiology of bloodstream infections and antimicrobial resistance in Dhaka, Bangladesh, 2005–2014. Antimicrob Resist Infect Control. 2017;6(1):2. doi:10.1186/s13756-016-0162-z
- Tauriainen T, Kinnunen E-M, Laitinen I, et al. Transfusion and blood stream infections after coronary surgery. Interact Cardiovasc Thorac Surg. 2017;26:325–327.
- Hassan EA, Elsherbiny NM, Abd El-Rehim AS, Soliman AMA, Ahmed AO. Health care-associated infections in pre-transplant liver intensive care unit: perspectives and challenges. J Infect Public Health. 2017;11:398–404. doi:10.1016/j.jiph.2017.09.006
- Labib JR, Ibrahim SK, Salem MR, Youssef MRL, Meligy B. Infection with gram-negative bacteria among children in a tertiary pediatric hospital in Egypt. Am J Infect Control. 2018;46(7):798–801. doi:10.1016/j.ajic.2017.12.008
- Bassetti M, Molinari MP, Mussap M, Viscoli C, Righi E. Candidaemia in internal medicine departments: the burden of a rising problem. Clin Microbiol Infect. 2013;19(6):E281–284. doi:10.1111/1469-0691.12155
- Brusselaers N, Vogelaers D, Blot S. The rising problem of antimicrobial resistance in the intensive care unit. Ann Intensive Care. 2011;1(1):47. doi:10.1186/2110-5820-1-47
- Goto M, Al-Hasan MN. Overall burden of bloodstream infection and nosocomial bloodstream infection in North America and Europe. Clin Microbiol Infect. 2013;19(6):501–509.
- Aiken AM, Mturi N, Njuguna P, et al. Risk and causes of paediatric hospital-acquired bacteraemia in Kilifi District Hospital, Kenya: a prospective cohort study. Lancet. 2011;378(9808):2021–2027. doi:10.1016/S0140-6736(11)61622-X
- Dagnew M, Yismaw G, Gizachew M, et al. Bacterial profile and antimicrobial susceptibility pattern in septicemia suspected patients attending Gondar University Hospital, Northwest Ethiopia. BMC Res Notes. 2013;6(1):283. doi:10.1186/1756-0500-6-283
- Endalafer N, Gebre-Selassie S, Kotiso B. Nosocomial bacterial infections in a tertiary hospital in Ethiopia. J Infect Prev. 2011;12(1):38–43. doi:10.1177/1757177410376680
- Wasihun AG, Wlekidan LN, Gebremariam SA, et al. Bacteriological profile and antimicrobial susceptibility patterns of blood culture isolates among febrile patients in Mekelle Hospital, Northern Ethiopia. SpringerPlus. 2015;4(1):314. doi:10.1186/s40064-015-1056-x
- Hailu D, Abera B, Yitayew G, Mekonnen D, Derbie A. Bacterial blood stream infections and antibiogram among febrile patients at Bahir Dar Regional Health Research Laboratory Center, Ethiopia. Ethiopian J Sci Technol. 2016;9(2):103–112. doi:10.4314/ejst.v9i2.3
- Kumalo A, Kassa T, Daka D, Tadesse AH. Bacterial profile of adult sepsis and their antimicrobial susceptibility pattern at Jimma University Specialized Hospital, South West Ethiopia. Health Sci J. 2016;10(2):45.
- Negussie A, Mulugeta G, Bedru A, et al. Bacteriological profile and antimicrobial susceptibility pattern of blood culture isolates among septicemia suspected children in selected hospitals Addis Ababa, Ethiopia. Int j Biol Med Res. 2015;6(1):4709.
- Seboxa T, Amogne W, Abebe W, et al. High mortality from blood stream infection in Addis Ababa, Ethiopia, is due to antimicrobial resistance. PLoS One. 2015;10(12):e0144944. doi:10.1371/journal.pone.0144944
- Russotto V, Cortegiani A, Graziano G, et al. Bloodstream infections in intensive care unit patients: distribution and antibiotic resistance of bacteria. Infect Drug Resist. 2015;8:287–296. doi:10.2147/IDR.S48810
- Bond A, Teubner A, Taylor M, et al. Assessing the impact of quality improvement measures on catheter related blood stream infections and catheter salvage: experience from a national intestinal failure unit. Clin Nutr. 2017;37:2097–2101. doi:10.1016/j.clnu.2017.10.002
- von Baum H, Ober JF, Wendt C, Wenzel RP, Edmond MB. Antibiotic-resistant bloodstream infections in hospitalized patients: specific risk factors in a high-risk population? Infection. 2005;33(5–6):320–326. doi:10.1007/s15010-005-5066-4
- Ozdemir K, Dizbay M. Nosocomial infection and risk factors in elderly patients in intensive care units. J Microbiol Infect Dis. 2015;5(01). doi:10.5799/ahinjs.02.2015.01.0174
- Ghadiri H, Vaez H, Khosravi S, Soleymani E. The antibiotic resistance profiles of bacterial strains isolated from patients with hospital-acquired bloodstream and urinary tract infections. Crit Care Res Pract. 2012;2012:890797. doi:10.1155/2012/890797
- World Health Organization. Global antimicrobial resistance and use surveillance system (GLASS) report: 2021; 2021.
- World Health Organization. Global antimicrobial resistance surveillance system; 2015.
- World Health Organization. Antimicrobial resistance: fact sheet; 2016.
- CDC. Antibiotic Resistance Threats in the United States. Centres for Disease Control and Prevention, US Department of Health and Human Services; 2013.
- Magiorakos AP, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281. doi:10.1111/j.1469-0691.2011.03570.x
- AAU. Addis Ababa university background information of the college of health sciences; 2017.
- Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest. 1992;101(6):1644–1655. doi:10.1378/chest.101.6.1644
- Levy MM, Fink MP, Marshall JC, et al. 2001 sccm/esicm/accp/ats/sis international sepsis definitions conference. Intensive Care Med. 2003;29(4):530–538. doi:10.1007/s00134-003-1662-x
- Naing L, Winn T, Rusli B. Practical issues in calculating the sample size for prevalence studies. Arch Orofacial Sci. 2006;1:9–14.
- Daniel WW, Cross CL. Biostatistics: a foundation for analysis in the health sciences. Biometrics. 1995;51:386. doi:10.2307/2533362
- Kitila KT, Tadesse BD, Tinsae K. Assessment of bacterial profile and antimicrobial resistance pattern of bacterial isolates from blood culture in Addis Ababa regional laboratory, Addis Ababa, Ethiopia. Clin Microbiol. 2018;7:2.
- Dreyer AW. Blood culture systems: from patient to result. In: Sepsis-An Ongoing and Significant Challenge. InTech; 2012.
- Lee D-H, Kim SC, Bae I-G, Koh E-H, Kim S. Clinical evaluation of BacT/Alert FA plus and FN plus bottles compared with standard bottles. J Clin Microbiol. 2013;51(12):4150–4155. doi:10.1128/JCM.01935-13
- Flayhart D, Borek AP, Wakefield T, Dick J, Carroll KC. Comparison of BACTEC PLUS blood culture media to BacT/Alert FA blood culture media for detection of bacterial pathogens in samples containing therapeutic levels of antibiotics. J Clin Microbiol. 2007;45(3):816–821. doi:10.1128/JCM.02064-06
- Cheesbrough M. District Laboratory Practice in Tropical Countries. Cambridge university press; 2006.
- CLSI. Performance standards for antimicrobial susceptibility testing; 27th informational supplement. Clin Lab Stand Inst. 2017;37(1):e34.
- Rods GP. UK standards for microbiology investigations; 2014.
- Alemnew B, Biazin H, Demis A, Abate Reta M. Bacterial profile among patients with suspected bloodstream infections in Ethiopia: a systematic review and meta-analysis. Int J Microbiol. 2020;2020:8853053. doi:10.1155/2020/8853053
- Apostolopoulou E, Zikos D, Tselebis A, et al. Clinical outcomes and economic variables in critically ill patients with bloodstream infections. Health Sci J. 2014;8(4):519.
- Mitiku M, Ayenew Z, Desta K. Multi-drug resistant, extended spectrum beta-lactamase and carbapenemase producing bacterial isolates among septicemia suspected under five children in tikur anbesa specialized hospital, Addis Ababa Ethiopia: cross-sectional study; 2019.
- Archibald LK, McDonald LC, Nwanyanwu O, et al. A hospital-based prevalence survey of bloodstream infections in febrile patients in Malawi: implications for diagnosis and therapy. J Infect Dis. 2000;181(4):1414–1420. doi:10.1086/315367
- Aryal SC, Upreti MK, Sah AK, et al. Plasmid-mediated AmpC β-lactamase CITM and DHAM genes among gram-negative clinical isolates. Infect Drug Resist. 2020;13:4249. doi:10.2147/IDR.S284751
- Blomberg B, Manji KP, Urassa WK, et al. Antimicrobial resistance predicts death in Tanzanian children with bloodstream infections: a prospective cohort study. BMC Infect Dis. 2007;7(1):1–14. doi:10.1186/1471-2334-7-43
- Deku JG, Dakorah MP, Lokpo SY, et al. The epidemiology of bloodstream infections and antimicrobial susceptibility patterns: a nine-year retrospective study at St. Dominic Hospital, Akwatia, Ghana. J Trop Med. 2019;2019:1–10. doi:10.1155/2019/6750864
- Behmadi H, Borji A, Taghavi-Rad A, Soghandi L, Behmadi R. Prevalence and antibiotic resistance of neonatal sepsis pathogens in Neyshabour, Iran. Arch Pediatr Infect Dis. 2016;4(2). doi:10.5812/pedinfect.33818
- Klevens RM, Edwards JR, Richards JCL, et al. Estimating health care-associated infections and deaths in US hospitals, 2002. Public Health Rep. 2007;122(2):160–166. doi:10.1177/003335490712200205
- Droz N, Hsia Y, Ellis S, Dramowski A, Sharland M, Basmaci R. Bacterial pathogens and resistance causing community acquired paediatric bloodstream infections in low-and middle-income countries: a systematic review and meta-analysis. Antimicrob Resist Infect Control. 2019;8(1):1–12. doi:10.1186/s13756-019-0673-5
- Khan ID, Basu A, Kiran S, Trivedi S, Pandit P, Chattoraj A. Device-Associated Healthcare-Associated Infections (DA-HAI) and the caveat of multiresistance in a multidisciplinary intensive care unit. Med J Armed Forces India. 2017;73(3):222–231. doi:10.1016/j.mjafi.2016.10.008
- Omoregie R, Egbe C, Ogefere H, Igbarumah I, Omijie R. Effects of gender and seasonal variation on the prevalence of bacterial septicaemia among young children in Benin City, Nigeria. Libyan J Med. 2009;4(3):153–157. doi:10.4176/090206
- Endris M, Takele Y, Woldeyohannes D, et al. Characteristics of bacterial sepsis among patients with visceral leishmaniasis. Asian Pac J Trop Biomed. 2014;4(11):871–875. doi:10.12980/APJTB.4.2014C1133
- Manyahi J, Kibwana U, Mgimba E, Majigo M. Multi-drug resistant bacteria predict mortality in bloodstream infection in a tertiary setting in Tanzania. PLoS One. 2020;15(3):e0220424. doi:10.1371/journal.pone.0220424
- Ghiorghis B. Neonatal sepsis in Addis Ababa, Ethiopia: a review of 151 bacteremic neonates. Ethiop Med J. 1997;35(3):169–176.
- McKay R, Bamford C. Community-versus healthcare-acquired bloodstream infections at groote schuur hospital, Cape Town, South Africa. South Afr Med J. 2015;105(5):363–369. doi:10.7196/SAMJ.8183
- Zarrilli R, Bagattini M, Esposito EP, Triassi M. Acinetobacter infections in neonates. Curr Infect Dis Rep. 2018;20(12):1–5. doi:10.1007/s11908-018-0654-5
- Adatara P, Afaya A, Salia SM, et al. Risk factors associated with neonatal sepsis: a case study at a specialist hospital in Ghana. Scientific World J. 2019;2019:1–8. doi:10.1155/2019/9369051
- Özmeral Odabaşı I, Bülbül A. Neonatal sepsis. The Medical Bulletin of Sisli Etfal Hospital; 2020.
- Grasselli G, Scaravilli V, Di Bella S, et al. Nosocomial infections during extracorporeal membrane oxygenation: incidence, etiology, and impact on patients’ outcome. Crit Care Med. 2017;45(10):1726–1733. doi:10.1097/CCM.0000000000002652
- Leal HF, Azevedo J, Silva GEO, et al. Bloodstream infections caused by multidrug-resistant gram-negative bacteria: epidemiological, clinical and microbiological features. BMC Infect Dis. 2019;19(1):1–11. doi:10.1186/s12879-019-4265-z
- Phungoen P, Lerdprawat N, Sawanyawisuth K, et al. Clinical factors associated with bloodstream infection at the emergency department. BMC Emerg Med. 2021;21(1):30. doi:10.1186/s12873-021-00426-2
- Birru M, Woldemariam M, Manilal A, et al. Bacterial profile, antimicrobial susceptibility patterns, and associated factors among bloodstream infection suspected patients attending Arba Minch General Hospital, Ethiopia. Sci Rep. 2021;11(1):1–13. doi:10.1038/s41598-021-95314-x
- Zaidi AK, Huskins WC, Thaver D, Bhutta ZA, Abbas Z, Goldmann DA. Hospital-acquired neonatal infections in developing countries. Lancet. 2005;365(9465):1175–1188. doi:10.1016/S0140-6736(05)71881-X
- Perlman SE, Saiman L, Larson EL. Risk factors for late-onset health care–associated bloodstream infections in patients in neonatal intensive care units. Am J Infect Control. 2007;35(3):177–182. doi:10.1016/j.ajic.2006.01.002
- Worku K. Ethiopia-National Guidelines for TB, DR-TB and Leprosy in Ethiopia. 6th ed. Vol. 6. Addis Ababa, Ethiopia: Minisrtry of health of FDRE; 2017:1–217.
- Teklu DS, Negeri AA, Legese MH, Bedada TL, Woldemariam HK, Tullu KD. Extended-spectrum beta-lactamase production and multi-drug resistance among Enterobacteriaceae isolated in Addis Ababa, Ethiopia. Antimicrob Resist Infect Control. 2019;8(1):1–12. doi:10.1186/s13756-019-0488-4
- Tola H, Holakouie-Naieni K, Mansournia MA, et al. National treatment outcome and predictors of death and treatment failure in multidrug-resistant tuberculosis in Ethiopia: a 10-year retrospective cohort study. BMJ open. 2021;11(8):e040862. doi:10.1136/bmjopen-2020-040862
- Elamreen FA. Neonatal sepsis due to multidrug-resistant Klebsiella terrigena in the neonatal intensive care unit in Gaza, Palestine. Critical Care. 2007;11(4):1. doi:10.1186/cc5991
- Coskun Y, Atici S. Successful treatment of Pandrug-resistant Klebsiella pneumoniae infection with ceftazidime-avibactam in a preterm infant: a case report. Pediatr Infect Dis J. 2020;39(9):854–856. doi:10.1097/INF.0000000000002807
- Gainey AB, Burch AK, Brownstein MJ, et al. Combining bacteriophages with cefiderocol and meropenem/vaborbactam to treat a pan‐drug resistant Achromobacter species infection in a pediatric cystic fibrosis patient. Pediatr Pulmonol. 2020;55(11):2990–2994. doi:10.1002/ppul.24945
- Oishi T, Saito A, Fukuda Y, et al. Analysis of risk factors for multidrug-resistant pathogens and appropriate treatment indications for pneumonia in children with neurologic impairment. J Infect Chemother. 2021;27(2):342–347. doi:10.1016/j.jiac.2020.12.007
- Chukwumeze F, Lenglet A, Olubiyo R, et al. Multi-drug resistance and high mortality associated with community-acquired bloodstream infections in children in conflict-affected northwest Nigeria. Sci Rep. 2021;11(1):1–12. doi:10.1038/s41598-021-00149-1