Abstract
Background
The emergence of carbapenem and colistin co-resistant Escherichia coli poses a huge challenge to infection control. The purpose of this study was to clarify the mechanism of the carbapenems and colistin co-resistance in E. coli strains.
Methods
Antimicrobial susceptibility test was carried out by agar dilution methods and colistin resistance was confirmed by broth microdilution methods. Whole genome sequencing was carried out, and resistance genes, sequence types and virulence genes of carbapenems and colistin co-resistance E. coli isolates were analyzed.
Results
The results showed that among the 176 carbapenem-resistant Enterobacteriaceae strains, 5 multidrug resistant E. coli strains exhibiting coresistance to carbapenem and colistin. The main mechanism of 5 E. coli strains in this study was generating carbapenem. Four E. coli strains were mcr-positive, while one mcr-negative strain had a new MgrB mutation. The blaNDM-5, blaCTX-M-65, blaOXA-10, blaTEM-1 and mcr-1.1 genes were simultaneously detected in E. coli 20IR1127 strain belonging to ST156 lineage. Other antimicrobial resistance genes encoding aminoglycosides-, sulfonamide-, chloramphenicol-, tetracyclines- and macrolides resistance were also detected.
Conclusion
The main mechanisms of carbapenem and colistin resistance were encoded by blaNDM and mcr1.1, meanwhile mgrB mutations also contribute to colistin resistance. To our knowledge, this study is the first to report of E. coli ST156 strain in which the blaNDM-5, blaCTX-M-65, blaOXA-10, blaTEM-1 and mcr1.1 genes coexist. In addition, there is also an E. coli ST457 strain, which carries blaTEM-1, blaNDM-9, blaCTX-M-199 and is positive for mcr1.1 gene.
Introduction
Multidrug resistance in Escherichia coli has become a concerning issue that is increasingly observed in human but also in veterinary medicine around the world.Citation1 E. coli is essentially sensitive to almost all clinically related antibiotics, but this bacterium has a great ability to accumulate antibiotic resistance genes, mainly through horizontal gene transfer.Citation2 The most serious resistance mechanisms in E. coli is related to the acquisition of genes coding for carbapenemases, extended-spectrum β-lactamases, plasmid-mediated quinolone resistance (PMQR) genes, and mcr genes (conferring resistance to polymyxins).Citation3 The existence of plasmid-mediated antimicrobial resistance genes significantly increases the spread of carbapenem resistance, while further limiting the choice of effective antimicrobials. The spread and emergence of carbapenem-resistance caused by carbapenemase producing Enterobacteriaceae (CPE) and the deficiency of development of new antibiotics have led to the re-use of colistin in the treatment of patients with CPE-related infections.Citation4 Colistin is a cationic amphiphilic lipopeptide antibacterial agent, which is an important antibiotic for human treatment of multiple antibiotic-resistant (MDR) Gram-negative rod-shaped bacteria,Citation5,Citation6 as been referred to as “a last-resort antimicrobial”. Colistin has good activity against all kinds of gram-negative rod-shaped bacteria in vitro, including MDR Pseudomonas aeruginosa, Klebsiella pneumoniae and Acinetobacter baumannii.Citation7 According to literature reports, the mcr-mediated polymyxin resistance rate in clinical cases is about 1%, and the polymyxin resistance rate caused by bacterial chromosome mutation is 0.67%-1.6%.Citation8 Although the antibiotic resistance rate of colistin in population is not high, with the global spread of colistin resistance gene mcr, the clinical application of colistin is under serious threat.
Used colistin in the treatment of carbapenem-resistant bacteria in human patients has given rise to an increase in colistin resistance, which is due to the change in lipid A of lipopolysaccharides caused by chromosome point mutation.Citation9 The emergence and increase of carbapenem and colistin co-resistant to E. coli is an urgent problem to be studied.Citation10
The purpose of this study is to illustrate the mechanism of the carbapenems and colistin co-resistance in E. coli strains. We collected co-resistant E. coli clinical isolates from a children’s hospital, and performed this study through methods such as whole genome sequencing (WGS), antimicrobial susceptibility testing, to provide further understanding for the resistance development of E. coli strains. Finally, we aimed to clarify the mechanism of the carbapenems and colistin co-resistance in carbapenem and colistin co-resistance E. coli strains obtained from children crowd using WGS.
Materials and Methods
Bacterial Isolates and Colistin Resistance Screening
A 176 clinical Carbapenem-Resistant Enterobacteriaceae (CRE) isolates were recovered from the Children Hospital, Zhejiang University School of Medicine, from 2015 to 2020. All isolates were identified by MALDI-TOF MS using a Bruker Biotyper mass spectrometer (Bruker Daltonics, Germany). The study has been approved by the Ethics Committee of the Children’s Hospital (2021-IRB-031), Zhejiang University School of Medicine.
The colistin-resistant isolates (MIC > 2) were selected to confirm the resistance phenotype by colistin microdilution in cation-adjusted Mueller-Hinton broth according to standardized methods (EUCAST, http://www.eucast.org/). E. coli ATCC 25922 and Pseudomonas aeruginosa 27,853 was used as quality control. The results showed that five strains of E. coli were co-resistant to carbapenem and colistin.
Antimicrobial Susceptibility Testing
The MIC of six other antibiotics including cefepime (FEP), ceftazidime (CAZ), levofloxacin (LVX), amikacin (AMK), imipenem (IPM) and piperacillin/tazobactam (TZP) in all carbapenem and colistin-resistant E. coli strains were further detected by broth dilution method. All antibiotic sensitivity results were interpreted according to the interpretation criteria of the Institute of Clinical and Laboratory Standards (CLSI).Citation11
Whole Genome Sequencing and Genome Assembly
E. coli strains co-resistant to carbapenem and colistin were identified by Whole Genome Sequencing (WGS), and the genetic characteristics and ST type were determined. Particularly, we determined multi-locus sequence type (MLST), virulence- and antibiotic resistance genes carriage. DNA was purified from carbapenem and colistin co-resistance isolates using QIAGEN-QiaAmp DNA Mini kit (QIAGEN, Hilden, Germany). DNA was quantified using a BioDrop mLite+ (BioDrop, Cambridge, UK) and standardized to 30 ng/uL before being prepared into sequencing, as described previously.Citation4 The extracted DNA was sent to Hangzhou Digital-Micro Biotechnology Co., Ltd. for sequencing. After library construction, WGS was performed on Illumina HiSeq xTen platform using a 2 × 150-bp paired end (PE) configuration. Sequencing reads were trimmed and de novo assembled into contigs using the Shovill pipeline (https://github.com/tseemann/shovill). Genome analysis was performed in the Center for Genomic Epidemiology (CGE) by uploading the contigs files obtained from the de novo assembly of the WGS data.Citation12 The sequence files were compared with the virulence factor database (VFDB) by ABRICATE software (V.0.8.10) (https://github.com/tseemann/abricate) to confirm the virulence factors.
Results
Bacterial Isolates, Antimicrobial Susceptibility Testing and Molecular Epidemiology
From 2015 to 2020, a total of 176 carbapenem-resistant clinical isolates of Enterobacteriaceae were recovered from the studied hospital. The bacterial species included Klebsiella pneumoniae (73%), Escherichia coli (17%), Klebsiella oxytoca (8%), Citrobacter flodi (1%), Raoultella ornithinolytica (1%). According to the results of the antimicrobial susceptibility test (), 5 strains of E. coli were co-resistant to carbapenem and colistin. By determination of MICs of clinical antibiotics, we showed that all the 5 E. coli strains were MDR. E. coli co-resistant to carbapenem and colistin had high resistance to antibiotics commonly used in clinic except for amikacin. In addition, the five strains belonged to five sequence types (STs), namely ST131 (n = 1), ST7125 (n = 1), ST10 (n = 1), ST156 (n = 1), and ST457 (n = 1).
Table 1 Susceptibility to the Antimicrobial Agents, Clinical Characterization and Phenotypic Detection of E. coli
Resistance Mechanism of Carbapenem Antimicrobials
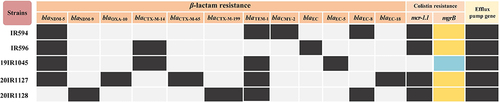
Through WGS analysis, a variety of acquired β-lactamase encoding genes were identified in the five E. coli strains. EC encoding genes were identified in all 5 E. coli isolates with blaEC-8 as the dominant subtype. The blaCTX-M-14 (n = 2), blaCTX-M-65 (n = 1) and blaCTX-M-199 (n = 1) genes were identified in four of our isolates. AmpC encoding genes was found in one isolates harboring blaCMY-2. Furthermore, other β-lactamase encoding genes namely blaTEM-1 (n = 4) and blaOXA-10 (n = 1). Carbapenemase encoding genes were authenticated in all isolates through WGS, including blaNDM-5 (n = 4) and blaNDM-9 (n = 1). Specific results are shown in .
Mechanisms of Colistin Resistance
The MIC of colistin for the five E. coli isolates was 4–64 μg/mL. Four of five E. coli isolates were mcr-1.1 positive. Isolates 19IR1045 was showed the amino acid alterations: Val8Ala in MgrB, the specific results are shown in . The mcr-1.1 coexisted with three or more resistance genes in the mcr-1.1 positive E. coli isolates, demonstrating that the four mcr-1.1-positive isolates were all MDR bacteria. In addition, the five E. coli strains carried all kinds of efflux pump genes, as shown in .
Table 2 Efflux Pump Gene, Integron and Virulence Gene Distribution Characteristics of 5 Strains of Clinically Isolated E. coli
Resistance Mechanisms to Other Antimicrobial Agents
Acquired non-β-lactam-resistance genes were observed for aminoglycosides (n = 5), sulfonamides (n = 4), chloramphenicol (n = 4), tetracyclines (n = 3), and macrolides (n = 3). Aminoglycosides encoding genes were aph(3’)-Ia-like (n = 3), and aph(6)-Id-like (n = 3), while sulfonamides resistance was encoded by sul2 in four isolate. Furthermore, resistance to chloramphenicol and macrolide was encoded by floR (n = 3) and mph(A) (n = 3) genes, respectively. In addition, three E. coli strains carried integrons, being In498, In1411, and In1249 ().
Detection of Virulence Genes
Virulence factors expression is more common in some gene-related populations of E. coli, which form virulent clones in larger E. coli populations. Detection of Virulence Genes The fimA-I, rcsB genes were the most abundant virulence genes detected in the five E. coli strains (). We also detected the virulence genes fimA-I, iroN, papB, papI, rcsB, fyuA/psn, hlyA-D, iucA-D, iutA, papC and papG in our isolates.
Discussion
E. coli can survive in a variety of environment and obtain resistance to various antibiotic by obtaining exogenous resistance genes.Citation13 The emergence of MDR E. coli poses a huge challenge for effective clinical treatment. Carbapenem is a typical β-lactam antibiotic has the best antibacterial effects at present.Citation14 Keeping good sensitivity to Enterobacteriaceae carrying ESBLs, and is the choice for clinical control of MDR E. coli infections. Colistin is an “old” antibiotic, which has been reapplied to the clinic because of its good antibacterial activity against MDR gram-negative rod-shaped bacteria.Citation15
In this study, 5 carbapenem and colistin co-resistant E. coli isolates were screened out from 176 carbapenem-resistant clinical isolates of Enterobacteriaceae in a Children's Hospital in China and all 5 E. coli isolates showed MDR phenotypes. Through our statistical analysis of WGS data, it can provide a large number of results on resistant isolates, such as serotypes, MLST types, integron and resistant genes. It may take longer and more expensive to obtain all of this data through conventional methods.
All the five E. coli strains showed MDR profiles, including resistance to cefepime, ceftazidime, levofloxacin, and piperacillin/tazobactam. These results further reflect the important role of bacterial antibiotic resistance mechanism in clinic. Usually, the carbapenems and colistin were one of the last treatment options in life-threatening multidrug-resistant Enterobacteriaceae infections.Citation16 WGS data show that these isolates contain various determinants of antibiotic resistance, which indicating that carbapenem and colistin co-resistant strains may be selected for any use of antibiotics.
Although there are not few studies on the resistance of E. coli to carbapenem or colistin, the reports on strains isolated from children are not perfect. To the best of our knowledge, this study is the first to report an E. coli ST156 strain 20IR1127 in which the genes blaNDM-5, blaCTX-M-65, blaOXA-10, blaTEM-1 and mcr1.1 coexist, thereby expounding the molecular characteristics and resistance gene diversity of this strain. In addition, there is an E. coli ST457 strain, which carries blaTEM-1, blaNDM-9, blaCTX-M-199 and is positive for mcr1.1 gene. The referential results of these genome sequences are helpful for further comparative analysis of the genomes of E. coli strains, and provides genetic background information of the antimicrobial resistance.
Specific mutations in regulators MgrB and the carrying of mcr gene are associated with colistin resistance in bacterial, including K. pneumoniae, K. aerogenes, and Salmonella enterica, as well as P.aeruginosa, and A.baumannii.Citation17–19 However, colistin resistance mechanisms in E. coli remain to be characterized. A mutation in MgrB was found in only one E. coli isolate, and mcr1.1 gene was found in 4 strains in this study. In the present study, a mutation Val8Ala in MgrB was observed in 19IR1045 isolate. After reading the published studies, the mutation of Val8Ala in MgrB has not been reported in the literature.
According to the literature,Citation20,Citation21 ST131 and ST10 E. coli is one of the high-risk multidrug-resistant clones with a global distribution and the ability to survive and colonize in a variety of niches. In our study, IR596 and 19IR1045 isolate belongs to ST10 and ST131 colistin-resistant E. coli, respectively. Studies have reported that, E. coli ST131 is a great model organism to investigate the emergence of superbugs.Citation20 CTX-M-15-producing E. coli often belongs to a sequence type called ST131.Citation20 However, our study shows that this strain belongs to CTX-M-14-producing ST131 strain. E. coli ST131 also showing high virulence and high antibiotic resistance.Citation22 Indeed, in our study, we also found that ST131 carries more virulence genes and has stronger resistance.
Conclusion
Carbapenem and colistin co-resistant E. coli strains cause serious public concern worldwide. To sum up, the main mechanism of carbapenem resistance in this study is production carbapenemase. The plasmid-mediated mcr genes contribute to the transfer and occurrence of colistin resistance in 5 E. coli strains. In addition, colistin resistance in E. coli was related to mutations in regulators by antibiotic selective pressure. Efforts to reduce colistin consumption should be redoubled, to prevent the occurrence of carbapenem and colistin co-resistant E. coli strains.
Data Sharing Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: NCBI; SAMN28858598, SAMN28858599, SAMN28858600, SAMN28858601, SAMN28858602.
Ethics Statement
The studies involving human participants were reviewed and approved by The Research and Ethics committee of The Children’s Hospital, Zhejiang University School of Medicine (2021-IRB-031). Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
Additional information
Funding
References
- Allocati N, Masulli M, Alexeyev MF, Di Ilio C. Escherichia coli in Europe: an overview. Int J Environ Res Public Health. 2013;10(12):6235–6254. doi:10.3390/ijerph10126235
- Snyman Y, Whitelaw AC, Reuter S, Maloba MRB, Newton-Foot M. Colistin resistance mechanisms in clinical Escherichia coli and Klebsiella spp. Isolates from the Western Cape of South Africa. Microb Drug Resist. 2021;27(9):1249–1258. doi:10.1089/mdr.2020.0479
- Liu YY, Wang Y, Walsh TR, et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis. 2016;16(2):161–168. doi:10.1016/S1473-3099(15)00424-7
- Maciuca IE, Cummins ML, Cozma AP, et al. Genetic features of mcr-1 mediated colistin resistance in CMY-2-producing Escherichia coli from Romanian poultry. Front Microbiol. 2019;10:2267. doi:10.3389/fmicb.2019.02267
- Nation RL, Velkov T, Li J. Colistin and polymyxin B: peas in a pod, or chalk and cheese? Clin Infect Dis. 2014;59(1):88–94. doi:10.1093/cid/ciu213
- Biswas S, Brunel JM, Dubus JC, Reynaud-Gaubert M, Rolain JM. Colistin: an update on the antibiotic of the 21st century. Expert Rev Anti Infect Ther. 2012;10(8):917–934. doi:10.1586/eri.12.78
- Ling Z, Yin W, Shen Z, Wang Y, Shen J, Walsh TR. Epidemiology of mobile colistin resistance genes mcr-1 to mcr-9. J Antimicrob Chemother. 2020;75(11):3087–3095. doi:10.1093/jac/dkaa205
- Lentz SAM, Dalmolin TV, Barth AL, Martins AF. mcr-1 Gene in Latin America: how is it disseminated among humans, animals, and the environment? Front Public Health. 2021;9:648940. doi:10.3389/fpubh.2021.648940
- Xu Y, Chen H, Zhang H, Ullah S, Hou T, Feng Y. The MCR-3 inside linker appears as a facilitator of colistin resistance. Cell Rep. 2021;35(7):109135. doi:10.1016/j.celrep.2021.109135
- Kumar M, Saha S, Subudhi E. More furious than ever: Escherichia coli-acquired co-resistance toward colistin and carbapenems. Clin Infect Dis. 2016;63(9):1267–1268. doi:10.1093/cid/ciw508
- Sahu C, Jain V, Mishra P, Prasad KN. Clinical and laboratory standards institute versus European committee for antimicrobial susceptibility testing guidelines for interpretation of carbapenem antimicrobial susceptibility results for Escherichia coli in urinary tract infection (UTI). J Lab Physicians. 2018;10(3):289–293. doi:10.4103/JLP.JLP_176_17
- Larsen MV, Cosentino S, Rasmussen S, et al. Multilocus sequence typing of total-genome-sequenced bacteria. J Clin Microbiol. 2012;50(4):1355–1361. doi:10.1128/JCM.06094-11
- Jang J, Hur HG, Sadowsky MJ, Byappanahalli MN, Yan T, Ishii S. Environmental Escherichia coli: ecology and public health implications-a review. J Appl Microbiol. 2017;123(3):570–581. doi:10.1111/jam.13468
- El-Gamal MI, Brahim I, Hisham N, Aladdin R, Mohammed H, Bahaaeldin A. Recent updates of carbapenem antibiotics. Eur J Med Chem. 2017;131:185–195. doi:10.1016/j.ejmech.2017.03.022
- Liu S, Fang R, Zhang Y, et al. Characterization of resistance mechanisms of Enterobacter cloacae Complex co-resistant to carbapenem and colistin. BMC Microbiol. 2021;21(1):208. doi:10.1186/s12866-021-02250-x
- Sun H, Zhang Q, Wang R, et al. Resensitizing carbapenem- and colistin-resistant bacteria to antibiotics using auranofin. Nat Commun. 2020;11(1):5263. doi:10.1038/s41467-020-18939-y
- Jin X, Chen Q, Shen F, et al. Resistance evolution of hypervirulent carbapenem-resistant Klebsiella pneumoniae ST11 during treatment with tigecycline and polymyxin. Emerg Microbes Infect. 2021;10(1):1129–1136. doi:10.1080/22221751.2021.1937327
- D’Onofrio V, Conzemius R, Varda-Brkic D, et al. Epidemiology of colistin-resistant, carbapenemase-producing Enterobacteriaceae and Acinetobacter baumannii in Croatia. Infect Genet Evol. 2020;81:104263. doi:10.1016/j.meegid.2020.104263
- Meletis G, Skoura L. Polymyxin resistance mechanisms: from intrinsic resistance to mcr genes. Recent Pat Antiinfect Drug Discov. 2018;13(3):198–206. doi:10.2174/1574891X14666181126142704
- Taati Moghadam M, Mirzaei M, Fazel Tehrani Moghaddam M, et al. The challenge of global emergence of novel colistin-resistant Escherichia coli ST131. Microb Drug Resist. 2021;27(11):1513–1524. doi:10.1089/mdr.2020.0505
- Ali A, Fontana H, Sano E, et al. Genomic features of a high-risk mcr-1.1-positive Escherichia coli ST10 isolated from cattle farm environment. Environ Sci Pollut Res Int. 2021;28(38):54147–54152. doi:10.1007/s11356-021-15437-6
- Baquero F, Tedim AP, Coque TM. Antibiotic resistance shaping multi-level population biology of bacteria. Front Microbiol. 2013;4:15. doi:10.3389/fmicb.2013.00015