Abstract
Aggregatibacter aphrophilus is part of the normal flora in the oropharynx and upper respiratory tract, which causes invasive bacteremia in rare cases. However, the culture and identification of Aggregatibacter aphrophilus are challenging, hence easily misdiagnosed or undetected in clinical practice. In this case, a 73-year-old male patient was admitted to the hospital with a fever and right hip pain. Routine blood and C-reactive protein tests showed abnormal inflammatory markers. Positive blood culture revealed the presence of Aggregatibacter aphrophilus through mass spectrometry. The computed tomography examination further revealed the presence of psoas abscess, pulmonary infection, and pleural effusion, which was relieved by ceftriaxone combined with levofloxacin therapy, the drainage of psoas abscess and pleural effusion. Therefore, since multiple anatomic sites infection, including bloodstream, psoas abscess and pulmonary infection caused by Aggregatibacter aphrophilus, is rare, sufficient attention should be paid to its clinical diagnosis and treatment.
Introduction
Aggregatibacter aphrophilus is a gram-negative coccobacillus belonging to the genus Aggregatibacter. It is a fastidious bacterium in the HACEK family with high nutritional requirements.Citation1 Aggregatibacter aphrophilus often causes infective endocarditis,Citation2 brain abscess, liver abscess, empyema, endophthalmitis, epidural abscess, and sacroiliac arthritis.Citation3–8 Herein, we report the first case of bloodstream infection caused by Aggregatibacter aphrophilus accompanied by psoas abscess and pulmonary infection.
Case Presentation
A 73-year-old male patient was admitted to the hospital with a fever (the detailed temperature was not available) and chill for 6 days, and pain in the right hip area for a day. He also developed a headache and had an intermittent dry cough, after which he took over-the-counter drugs (details not available) before admission. The day before admission, the patient experienced a needle-like sharp pain in the right hip, especially when sitting, turning over, or performing strenuous activities, accompanied by radiating pain in the right lower limb. On the day of admission, he was hospitalized in the emergency department with a body temperature of up to 40.1°C. He was treated with cefoperazone/sulbactam and antipyretic and rehydration therapy, then transferred to the infectious disease department on the same day. The patient had no underlying diseases or history of other chronic diseases.
Physical Examination of the Patient on Admission
Basic physical examinations were performed, including pulse rate (86/min), respiratory rate (18/min), blood pressure (106/60mmHg) and oxygen saturation (95%). The breath sounds were rough in both lungs, and no dry or moist rale was heard. A discomfort was felt on the right upper abdomen when pressed, along with positive percussion pain on the right lumbar areas. No other obvious abnormalities were found.
Laboratory Examination
Routine blood tests on admission characterized the white blood cell count (23.29×109/L), neutrophil percentage (0.93), C reaction protein (CRP, 201.2 mg/L), procalcitonin (PCT, 20.76 ng/mL), neutrophil alkaline phosphatase score (286), serum γ-glutamyl transferase (229 U/L), albumin (30.3 g/L), and pro-brain natriuretic peptide (1714.0 pg/mL). Renal functions, including electrolytes, lactic acid, and coagulation indexes, were normal. Infections by HIV and Treponema pallidum were excluded by immunological tests and markers for tumor, diabetes and rheumatoid arthritis in blood were within the normal ranges.
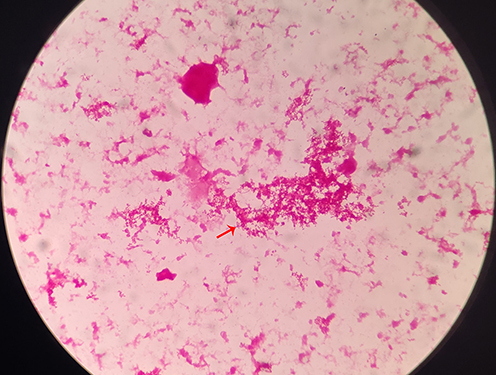
Bacterial Culture, Species Identification and Susceptibility Test
Blood cultures before admission to the emergency department and 1 day after admission were positive for Gram-negative bacteria (). No other bacteria or fungus were grown. Mass spectrometry identified two homologous strains of Aggregatibacter aphrophilus. Drug sensitivity tests based on the guidelines by the Clinical and Laboratory Standards Institute revealed that the bacteria were completely susceptible to ceftriaxone and levofloxacin and moderately susceptible to imipenem.Citation9
Diagnosis and Treatment Process
On the day of admission, chest plain computed tomography (CT) revealed infectious lesions scattered in both lungs, with a small amount of pleural effusion in the left lung (). Initially, the patient was intravenously injected with 2 g of cefoperazone/sulbactam every 8 h. The blood inflammatory markers (PCT and CRP) were slightly decreased upon re-examination. However, the fever recurred with temperatures reaching 38–39°C on certain days. Lung CT re-examination 4 days after admission showed multiple exudations in both lungs and pleural effusion on each side (). Compared to the observations upon admission, pathological changes were significantly increased in both lungs, with increased pleural effusion on each side. In addition, an abdominal enhanced CT revealed a psoas abscess in the right psoas (). Five days after admission, the patient complained of chest tightness. The oxygen saturation without oxygen inhalation was 92–93%. Given the worsened pulmonary infection and psoas abscess revealed by the abdominal CT, a severe infection was considered. Therefore, paracentesis under ultrasound guidance was performed to drain psoas abscess in the right psoas major (). The culture result of the tested pus was negative. Percutaneous thoracic drainage was conducted on the right thoracic cavity 6 days after admission, but the culture was negative.
Figure 2 Images of infection caused by Aggregatibacter aphrophilus. (A) CT images of lung at admission; (B) CT images of lung 4 days after admission, the red and black arrows indicate the infection lesions and the pleural effusion on the right lung, respectively; (C) CT images of abdomen 4 days after admission, the red arrows indicate the abscess; (D) Ultrasonic images of the right psoas muscle 5 days after admission, the red arrows shows the abscess region.
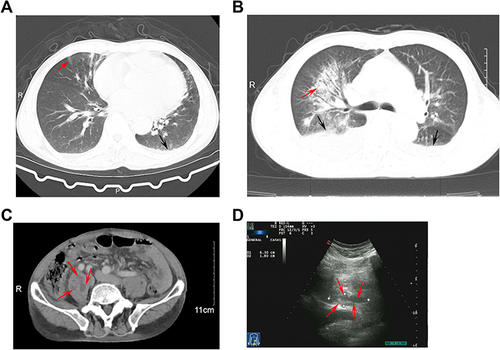
Based on the drug sensitivity results of the blood culture, the treatment was switched to ceftriaxone (2 g, intravenous injection) plus levofloxacin (0.5 g, oral administration) once daily. During this period, methylprednisolone sodium succinate was injected to modulate inflammation and improve oxygenation. After the comprehensive treatments, re-examination revealed a gradual decline in blood inflammatory markers and cleared bacteria (negative blood culture). The patient was discharged after 3 weeks of hospitalization and continued with cefixime (0.1 g twice per day) plus levofloxacin (0.5 g once per day) orally administered for 9 days. The entire treatment period was 30 days. Eventually, the blood inflammatory markers of the patient returned to normal, and the lung images showed that lung lesions () had disappeared and abdominal images revealed the obvious absorption in the psoas abscess ( and ).
Discussion
Aggregatibacter aphrophilus is part of the normal oropharynx and upper respiratory tract flora, commonly isolated from dental plaque and saliva.Citation10 In this case, Aggregatibacter aphrophilus was isolated from the patient with infections in lung, psoas and blood stream.
Although Aggregatibacter aphrophilus could cause abscess in several anatomic sites, including the brain, temple, spine, psoas and endocardium, a bloodstream infection with positive culture is rare. Bloodstream infection induces a systematic toxic response characterized by an elevated body temperature and increased inflammatory markers in this study, which might be life-threatening if without timely treatment. Moreover, there is limited information on multiple anatomic sites infection caused by Aggregatibacter aphrophilus.Citation11–13 In this case, lung, psoas and bloodstream were infected with Aggregatibacter aphrophilus, contributing to knowledge on multiple anatomic site infections. However, Aggregatibacter aphrophilus was negative in pus from psoas and effusion fluid cultures, which is possibly due to the effective treatment using cefoperazone/sulbactam. Another reason for the negative culture could be the difficulty in culturing Aggregatibacter aphrophilus, since it was detected by nucleic acid detection in several previous studies.Citation5,Citation13–16 The immunosuppressed status and previous invasive procedures, such as tooth manipulation, subject patients to Aggregatibacter aphrophilus infection.Citation17,Citation18 However, in this case, the patient was not predisposed to these risk factors, implying its potential to infect immunocompetent individuals, as reported previously.Citation17,Citation19–21
In this study, a combined intravenous cefoperazone/sulbactam therapy effective, given the negative results from pus and pleural fluid cultures. Based on the antibiotic susceptibility test, other antibiotic regiments, including cephalosporins and quinolones, have proven also efficient in treating Aggregatibacter aphrophilus-related infections.Citation4,Citation13,Citation16,Citation19,Citation22 The duration of treatment should last for several weeks, which may differ on the infection sites and antibiotic agents.Citation13,Citation18,Citation23 However, the patient experienced recurrent fever during treatment, with obvious poisoning symptoms after the systemic infection. This might be associated with psoas abscess and pleural effusion in the lungs. When an experienced antibiotic treatment presents a poor outcome in the early stage, additional antibacterial drugs and other active interventions, such as drainage, could be combined to enhance a timely positive treatment effect.Citation16
Conclusion
In summary, a case of bloodstream infection accompanied by infections in psoas muscle and lungs caused by Aggregatibacter aphrophilus is rare in clinical practice. With the development of mass spectrometry, rare Aggregatibacter aphrophilus can be timely detected in clinical microbiological examinations. For patients with severe infections, attention should be given to the possibility of invasion and infection at multiple anatomic sites. With regard to treatment, combined administration of antibiotics should be considered. In addition, for local invasive infection sites, active interventions such as drainage are also essential for successful treatment.
Ethics and Consent Statements
Informed consent to participate in this case study and to publish the findings was obtained from the patient. This case study was reviewed and approved by the Ethics Committee and Institutional Review Board of Dongyang People’s Hospital (2022-YX-175).
Disclosure
The authors report no conflicts of interest in this work.
References
- Norskov-Lauritsen N. Classification, identification, and clinical significance of Haemophilus and Aggregatibacter species with host specificity for humans. Clin Microbiol Rev. 2014;27(2):214–240. doi:10.1128/CMR.00103-13
- Revest M, Egmann G, Cattoir V, Tattevin P. HACEK endocarditis: state-of-The-art. Expert Rev Anti Infect Ther. 2016;14(5):523–530. doi:10.1586/14787210.2016.1164032
- Miller DC, Fung M, Carbo A, Furry Friend’s A. Dirty Mouth: brain Abscess Due to Aggregatibacter (Haemophilus) aphrophilus. Am J Med. 2017;130(10):e447–e448. doi:10.1016/j.amjmed.2017.04.020
- Altdorfer A, Gavage P, Moerman F. Aggregatibacter aphrophilus spinal epidural abscess. BMJ Case Rep. 2020;13:7. doi:10.1136/bcr-2020-235320
- Okumura T, Soya K, Hihara Y, et al. The first known case of liver abscess caused by Aggregatibacter aphrophilus in Japan. Internal Medicine. 2020;59(11):1451–1455. doi:10.2169/internalmedicine.4220-19
- Rodriguez-Segade S, Velasco D, Marcos PJ. Empyema due to Aggregatibacter aphrophilus and Parvimonas micra coinfection. Arch Bronconeumol. 2015;51(5):254–255. doi:10.1016/j.arbr.2015.02.029
- Shum JW, Tsang FC, Fung KS, Li KK. Presumed Aggregatibacter aphrophilus endogenous endophthalmitis. Int Ophthalmol. 2015;35(2):269–273. doi:10.1007/s10792-015-0044-z
- Fernando SA, Gottlieb T. Aggregatibacter aphrophilus Sacroiliitis Following Gastroscopy in a Young Sportsman. Clin j sport med. 2017;27(1):e3–e5. doi:10.1097/JSM.0000000000000311
- CLSI. Methods for Antimicrobial Dilution and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria. 3rd ed. Wayne, PA: Clinical and Laboratory Standards Institute; 2016.
- Lindholm M, Claesson R, Kemoli A, et al. Aggregatibacter actinomycetemcomitans and Aggregatibacter aphrophilus in a Kenyan Maasai adolescent population and inhibition of leukotoxic activity by herbal plants used as part of oral hygiene procedures. J Clin Med. 2021;10(22):22. doi:10.3390/jcm10225402
- Sumer J, Haller S, Sawatzki M, Kellner J, Boggian K. An unusual case of multiple hepatic and pulmonary abscesses caused by Aggregatibacter aphrophilus in a young man: a case report. J Med Case Rep. 2021;15(1):34. doi:10.1186/s13256-020-02650-z
- Daoud H, Abugroun A, Olanipekun O, Garrison D. Infective endocarditis and brain abscess secondary to Aggregatibacter aphrophilus. IDCases. 2019;17:e00561. doi:10.1016/j.idcr.2019.e00561
- Belkacem A, Caseris M, Yazdanpanah Y. A Case of Aggregatibacter aphrophilus multiple abscess. Open Forum Infect Dis. 2015;2(2):ofv031. doi:10.1093/ofid/ofv031
- Bernard F, Rossi P, Lagier JC, Craighero F, Frances Y, Granel B. Lumbar septic arthritis and psoas abscess due to Aggregatibacter aphrophilus. BMJ Case Rep. 2011;2011(apr19 1):bcr0820103215–bcr0820103215. doi:10.1136/bcr.08.2010.3215
- Hirano K, Tokui T, Inagaki M, Fujii T, Maze Y, Toyoshima H. Aggregatibacter aphrophilus infective endocarditis confirmed by broad-range PCR diagnosis: a case report. Int J Surg Case Rep. 2017;31:150–153. doi:10.1016/j.ijscr.2017.01.041
- Wassef N, Sarkar D, Viswanathan G, et al. A rare cause of culture negative bioprosthetic valve endocarditis: a case report of Aggregatibacter aphrophilus infection. Eur Heart J Case Rep. 2021;5(2):ytab003. doi:10.1093/ehjcr/ytab003
- Maraki S, Papadakis IS, Chronakis E, Panagopoulos D, Vakis A. Aggregatibacter aphrophilus brain abscess secondary to primary tooth extraction: case report and literature review. J Microbiol Immunol Infect. 2016;49(1):119–122. doi:10.1016/j.jmii.2013.12.007
- Fernandez Gonzalez R, Gonzalez Noya A, Fernandez-Rodriguez R. Aggregatibacter aphrophilus brain abscess after tooth manipulation. Med Clin (Barc). 2021;157(7):355–356. doi:10.1016/j.medcli.2020.07.049
- Niu T, Tucker AM, Nagasawa DT, Bergsneider M. Solitary Aggregatibacter aphrophilus tectal abscess in an immunocompetent patient. Surg Neurol Int. 2017;8:257. doi:10.4103/sni.sni_211_17
- Inkaya AC, Macin S, Bozkurt G, Gocmen R, Akyon Y, Unal S. Aggregatibacter aphrophilus misidentified as Brucella spp. in an immunocompetent patient with brain abscess. J Pak Med Assoc. 2016;66(8):1032–1034.
- Chien YC, Huang YT, Liao CH, Chien JY, Hsueh PR. Clinical characteristics of bacteremia caused by Haemophilus and Aggregatibacter species and antimicrobial susceptibilities of the isolates. J Microbiol Immunol Infect. 2021;54(6):1130–1138. doi:10.1016/j.jmii.2020.12.002
- Granlund M, Åberg CH, Johansson A, Claesson R. Discrepancies in Antimicrobial Susceptibility between the JP2 and the Non-JP2 Genotype of Aggregatibacter actinomycetemcomitans. Antibiotics. 2022;11:3.
- Chen GB, Lu HZ. Brain abscess due to Aggregatibacter aphrophilus in association with atrial septal defectCase report and literature review. Clin Neurol Neurosurg. 2022;219:107337. doi:10.1016/j.clineuro.2022.107337