Abstract
Purpose
To explore the trends and correlation between antibiotics consumption and antimicrobial resistance in children in a specialist hospital from 2016–2021 in China.
Patients and Methods
This retrospective study investigated data on the consumption of antibiotics and antimicrobial resistance in children. Antibiotics consumption was expressed as defined daily doses (DDDs)/1000 patient-days based on the Guidelines for Anatomical Therapeutic Chemical. The trends in antibiotics consumption and antimicrobial resistance rates were analyzed by linear regression, while Spearman correlation analysis was employed to evaluate their correlations.
Results
An increasing trend in the annual consumption of carbapenems and monobactams was detected (all P<0.05). A significant upward trend was detected in the annual resistance rates of Enterococcus faecium to ciprofloxacin, Streptococcus pneumonia to ceftriaxone, Acinetobacter baumannii to carbapenems, Enterobacter cloacae to carbapenems, Pseudomonas aeruginosa to ceftazidime, and Escherichia coli to cefepime, while the annual resistance rates of Escherichia coli to carbapenems had a significant downward trend (all P<0.05). The consumption of cephalosporin/β-lactamase inhibitor (C/BLI) combinations and carbapenems had significant positive correlations with the resistance rates of Acinetobacter baumannii to carbapenems (r=0.763, P<0.001; r=0.806, P<0.001), Enterobacter cloacae to carbapenems (r=0.675, P<0.001; r=0.417, P=0.043), and Pseudomonas aeruginosa to ceftazidime (r=0.625, P=0.001; r=0.753, P<0.001), respectively. Also, increasing consumption of monobactams was related to the upward resistance rates of Acinetobacter baumannii to carbapenems (r=0.557, P=0.005) and Enterobacter cloacae to carbapenems (r=0.507, P= 0.011).
Conclusion
This study demonstrated significant positive associations between antibiotics consumption and specific antimicrobial resistance rates. The current findings pointed out some directions to pursue in controlling the prevalence of certain resistant bacterial strains in children.
Introduction
The widespread emergence of antibacterial resistance has become one of the major public health concerns for humankind due to unresponsiveness to treatment, which results in persistent illness and increased risk of death.Citation1 Specifically, multidrug-resistant organisms (MDROs) damage not only the infected patients but also other individuals. On the other hand, antibacterial resistance has brought a tremendous economic burden. The rate of global mortality attributed to antimicrobial resistance is estimated to reach 10 million annual deaths by 2050, with an economic impact of up to US $100 trillion.Citation2
In children, the status of antimicrobial resistance has worsened. One study monitoring the antimicrobial resistance of children in 2019 in China indicated that MDROs were widespread and presented high-level resistance, specifically carbapenem-resistant Acinetobacter baumannii (CR-AB) presenting >70% resistance to most antibacterial agents.Citation3 Additionally, pediatricians face particular challenges related to increasing antibacterial resistance; these include identifying and diagnosing the resistance, lack of novel antibiotics or child-friendly formulations, and limited access to research and clinical trials.Citation4 These facts necessitate advanced nationwide measures. In order to collect data from several laboratories on the temporal trends of bacterial epidemiology and resistance, the China antimicrobial surveillance network (CHINET) system was organized in 2005.Citation5 Also, the Infectious Disease Surveillance of Pediatrics (ISPED) program was established in 2015 to monitor the resistance of antibacterial agents among children in China.Citation3
Since the selection pressure contributed by continued high rates of antibiotic use has resulted in sustained resistant strains, which force a shift to more expensive and more broad-spectrum antibiotics and could be a vicious cycle.Citation6 Consequently, it is crucial to evaluate the association between antibiotic usage and antimicrobial resistance. Although some studies from China, Romanian, Serbia, North America, and Europe have assessed the relationship between antibiotic usage and antimicrobial resistance with precise statistical data,Citation7–17 the studied population, antibiotics and pathogens were different, and results of correlation between antibiotic use and antimicrobial resistance were not exactly the same. Moreover, no study targeting the trends and correlation between antimicrobial resistance and antibiotic use in children have yet been reported. Hence, the current study aimed to describe the trends of antibiotic consumption and antimicrobial resistance and further to access the correlation between antimicrobial resistance and antibiotics exposure in a specialist children’s hospital from 2016 to 2021. Due to the varied prescription behaviors, types of antibiotics, and status of pathogens resistance across countries or regions, the current study could be useful to local physicians and policymakers when planning effective intervention strategies to control the antibiotics use and reduce the antimicrobial resistance in children.
Materials and Methods
Study Design
This study retrospectively analyzed the data on antibiotics consumption and antimicrobial resistance in a specialist children’s hospital from January 1, 2016 to December 31, 2021. This study was conducted by the Maternal and Child Health Hospital of Hubei Province, a specialized hospital for women and children; it is a tertiary care, university-affiliated, and teaching hospital in the central region of China. A total of 670 beds are available for children in this hospital, which has an average level of 27,664 inpatients and 885,332 outpatients in children each year during the study periods.
This study was approved by the clinical research ethics committee of the Maternal and Child Health Hospital of Hubei Province (2020IEC029) and carried out in accordance with the Helsinki Declaration. The need to obtain individual informed consent was waived because this study utilized existing data collected from the hospital information system and did not pose any additional risks to the patients. Before data analysis, patient records and information were anonymous and unidentified.
Inclusion and Exclusion Criteria and Data Extraction
We only utilized the data of children, including the newborns, while the data regarding the patients, >14-years-old, were excluded. All isolates with data of susceptibility results were recruited, including the positive clinical specimens, such as blood, sputum, urine, cerebrospinal fluid, bronchoalveolar lavage fluid, wound, and anaerobic specimens etc. between 2016 and 2021. The isolates were obtained from community samples and outpatient clinics, and the susceptibilities were assessed using different methods; subsequently, incomplete data and the same susceptibility results for duplicate samples from the same patient were excluded from the study.
The data were extracted from the hospital information system by two researchers (W.G. and Z.J.). W.G. extracted the data on antibiotics consumption from the Pharmacy Department, while Z.J. extracted the antimicrobial data from the Clinical Microbiology Laboratory. The data extraction complied with the procedures stipulated by our hospital. First, the parameters were set according to the above inclusion and exclusion criteria with the help of the medical information staff. Second, the data extraction was based on a template, which included the following factors: age and sex of the patients, types and dosage of antibiotics, time of prescription and withdrawal of antibiotics, length of hospital stay, isolates identified, and drug susceptibility of the isolates (only the first strain was analyzed) etc. Third, strict privacy principles were supervised during data extraction, and no personal information related to the patients was disclosed.
Antibiotics Consumption
Antibiotics consumption was expressed as defined daily doses (DDDs)/1000 patient-days based on the Guidelines for Anatomical Therapeutic Chemical (ATC) classification and DDD assignment 23rd edition,Citation18 developed by the World Health Organization. Antibiotics were categorized according to the ATC. The prophylactic usage of antibiotics was not distinguished in this study.
Microbiology Data
Microbial organisms were identified and cultured according to the routine diagnostic standard operating procedures used in the clinical laboratory of this study hospital during the study period. Positive cultures were subcultured and identified to the species level using Bruker matrix-assisted laser desorption ionization time of flight (MALDI-TOF) mass spectrometry (Bruker Daltonik GmbH, Leipzig, Germany). Bacterial isolates were tested for susceptibility to antibiotics using the VITEK 2 Compact (BioMérieux) or manual Kirby–Bauer disc diffusion method, and yeast-like fungi were tested using ATB FUNGUS3 for susceptibility to antibiotics according to the interpretation criteria established by the Clinical Laboratory Standards Institute (CLSI, USA).Citation19 The quality control procedures were conducted according to the manufacturer’s instructions.
The resistance rate was defined as the percentage of resistant isolates among the tested isolates. Isolates with intermediate susceptibility were not included in the analysis of resistance. It should be pointed out that carbapenem-resistant bacteria in Enterobacteriaceae (CRE) were defined as resistance to either of imipenem, meropenem, and ertapenem in the current study. Because Pseudomonas aeruginosa (P. aeruginosa) and Acinetobacter baumannii (A. baumannii) exhibit natural resistance to ertapenem, CR-AB and carbapenem-resistant Pseudomonas aeruginosa was shown to have resistance to imipenem or meropenem.
Statistical Analysis
Linear regression was applied to evaluate the changing trends of antibiotics consumption and antimicrobial resistance from 2016 to 2021. The line trend by year was reported as the slope of the response with time, which was expressed by the coefficient (β). The Spearman correlation coefficient was used to assess the correlation between antibiotics consumption and antimicrobial resistance rates. All statistical analyses in this study were conducted using SPSS 21.0 (SPSS, USA). P<0.05 indicated a statistically significant difference.
Results
Selected General Characteristics of Patients
The selected general characteristics of the patients are listed in Supplementary Table 1. Most of the patients treated with antibiotics were diagnosed with respiratory system infection.
Antibiotics Consumption
The annual consumption trends of various categories of antibiotics are illustrated in . The DDDs of each antibiotic are shown in Supplementary Table 2. The usage trend of most of the antibiotics was stable during the study period. The annual use of carbapenems and monobactams increased markedly from 2016 to 2021 (all P < 0.05). The annual consumption of macrolides and oxazolidinone seem to have a decreasing trend, while the annual consumption of penicillins, cephalosporin/β-lactamase inhibitor (C/BLI) combinations, and β-lactam/β-lactamase inhibitor (BL/BLI) combinations seem to have an increasing trend. However, these trends did not show statistical significance. The BL/BLI combination is one of the largest varieties of consumption, especially the C/BLI combinations. The third frequently prescribed class of antimicrobial agent was macrolides. Penicillins [except for the penicillin/β-lactamase inhibitor (P/BLI) combinations] and cephalosporins (except for the C/BLI combinations) were the fourth and fifth frequently prescribed class of antimicrobial agents, respectively.
Table 1 Trends of Annual Consumption of Antibiotics in the Specialist Children’s Hospital During 2016–2021
Isolated Species
A total of 17,226 isolates with data of susceptibility results were recruited. Based on the exclusion criteria, 14,087 isolates with complete, non-repetitive susceptibility results were included for analysis in this study (Supplementary Figure 1). Supplementary Figure 2 shows the numbers of the isolated species in the special children’s hospital during 2016–2021. The top 11 frequently isolated species were Escherichia coli (E.coli), Staphylococcus aureus (S.aureus), Streptococcus pneumonia (S.pneumoniae), Klebsiella pneumoniae (K.pneumonia), Haemophilus influenza (H.influenzae), Candida albicans (C.albicans), A.baumannii, Enterococcus faecium (E.faecium), Enterobacter cloacae (E.cloacae), P.aeruginosa, and Staphylococcus epidermidis (S.epidermidis). Most of S.epidermidis belongs to the coagulase-negative staphylococci, whose pathogenicity needs to be assessed comprehensively according to the clinical situation. Therefore, we focused on the ten most frequently isolated species above (S. epidermidis were excluded) to analyze their resistance rates.
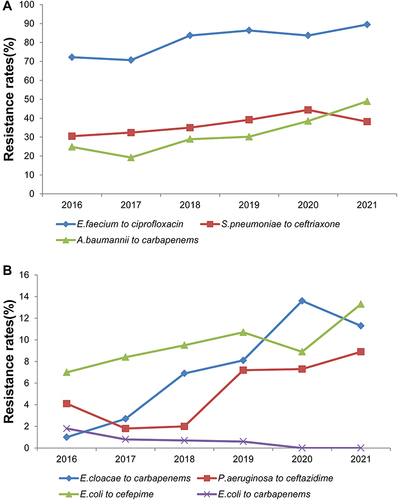
Antimicrobial Resistance
The trend of resistance rates with statistical significance is shown in . From 2016 to 2021, the annual trend showed a significant increase in the resistance rates of E. faecium to ciprofloxacin, S. pneumoniae to ceftriaxone, A. baumannii to carbapenems, E. cloacae to carbapenems, P. aeruginosa to ceftazidime, and E. coli to cefepime (all P < 0.05). Most of the annual resistance rates were maintained stable, while only the annual resistance rate of E. coli to carbapenems had a significant decreasing trend during the study period (P < 0.05). The various resistance rates are shown in Supplementary Table 3. Although most of the resistance rates were stable in this study, certain antimicrobial resistance rates should be under intensive focus as follows: the annual resistance rates of E. coli to ampicillin were >50% in each year, the resistance rates of E. cloacae to third-generation cephalosporins were all >10% and the resistance rates of K. pneumonia to ampicillin sulbactam and aztreonam were all >20% etc.
Figure 1 Annual trends of certain antimicrobial resistance rates during the study period. (A) Annual trends of resistance rates of E.faecium to ciprofloxacin, (S)pneumoniae to ceftriaxone and A.baumannii to carbapenems. (B) Annual trends of resistance rates of E.cloacae to carbapenems, (P)aeruginosa to ceftazidime and E.coli to cefepime and E.coli to carbapenems.
Correlation Between Antimicrobial Resistance and Antibiotic Consumption
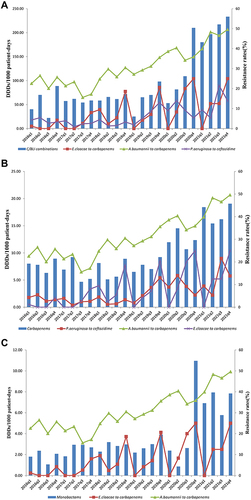
In order to preferably assess the association between antimicrobial resistance and antibiotic consumption, the quarterly data on resistance rates and DDDs were used for statistical analyses. Herein, we included the isolates that showed a significant increasing resistance trend to analyze the correlation between resistance rates and antibiotics consumption. Since most of the quarterly resistance rates of E. coli to carbapenems are 0, which is not suitable for statistical analysis, we did not include the E. coli to carbapenems to analyze the correlation. Similarly, the consumption of aminoglycosides, nitrofuran derivatives, sulfonamides, trimethoprim, lincosamides, streptogramins, and tetracycline was excluded from the correlation analysis.
The statistically significant associations between quarterly antimicrobial resistance rates and consumption of different antibiotics from 2016–2021 are shown in . Significantly positive associations were detected between the consumption of C/BLI combinations and BI/BLI combinations with the rates of E. cloacae to carbapenems (r=0.675, P<0.001; r=0.684, P<0.001), A. baumannii to carbapenems (r=0.763, P<0.001; r=0.770, P<0.001), and P. aeruginosa to ceftazidime (r=0.625, P=0.001; r=0.632, P=0.001), respectively. In the current study, BI/BLI combinations only contained the P/BLI combinations and C/BLI combinations; however, the P/BLI combinations did not show any significant associations with the resistance rates. Hence, the association of BI/BLI combinations and the resistance rates could be attributed to the C/BLI combinations. The usage of carbapenems was also positively correlated with the resistance rates of A. baumannii to carbapenems (r=0.806, P<0.001), E. cloacae to carbapenems (r=0.417, P=0.043), and P. aeruginosa to ceftazidime (r=0.753, P<0.001). Moreover, a significant positive association was detected in the consumption of monobactams to the resistance rates of A. baumannii to carbapenems (r=0.557, P= 0.005) and E. cloacae to carbapenems (r=0.507, P= 0.011). Nonetheless, no significant associations were detected between the consumption of various antibiotics and other resistance rates (Supplementary Table 4).
Figure 2 Associations between antibiotics consumption and antimicrobial resistance rates during the study period. (A) Correlation between C/BLI combinations and A.baumannii to carbapenems, E.cloacae to carbapenems and P.aeruginosa to ceftazidime. (B) Correlation between Carbapenems and A.baumannii to carbapenems, E.cloacae to carbapenems and P.aeruginosa to ceftazidime. (C) Correlation between Monobactams and A.baumannii to carbapenems and E.cloacae to carbapenems. The DDDs are shown on the left y-axis while the resistance rates are shown on the right y-axis.
Discussion
Although studies from different countries and regions have assessed the correlation between antibiotic usage and antimicrobial resistance,Citation7–17 to the best of our knowledge, the current study for the first time explored the correlations between antibiotics use and antimicrobial resistance rates in children. This study also demonstrated that the C/BLI combinations, carbapenems, and monobactams have a positive association with certain bacterial resistance rates in children. Based on the different prescription behaviors, antibiotics, and status of pathogens resistance across countries or regions, our findings might have some implications and reference values to help local pediatricians and decision-makers plan effective intervention strategies to control the antibiotics rationally, reduce antimicrobial resistance, and prevent the MDROs in children.
Most of the consumption of antibiotics remained stable, and the macrolides and oxazolidinone seemed to have a declining trend in the study period, suggesting that antimicrobial stewardship measures applied by our hospital are effective. In this hospital, a multidisciplinary antibiotic team consisting of microbiologists, clinical pharmacists, and clinicians was established in 2017 to improve the rational use of antibiotics. Although the BL/BLI combination is one of the largest varieties of consumption, which was in accordance with a previous study,Citation8 the C/BLI combinations accounted for >90% of BL/BLI combinations in our study, deeming it as the most frequently prescribed antibiotic combination in children. The current results showed that the consumption of carbapenems increased significantly, which was consistence with the global trends.Citation20,Citation21 Therefore, the usage of carbapenems in children is required to have restrictions. Strikingly, the consumption of monobactams increased markedly from 1.82–7.16 DDDs/1000 patient-days in this study, which was inconsistent with the previous studies in adults.Citation9,Citation10 This phenomenon could be partly explained by the fact that a skin test was not needed for monobactams and quinolones while penicillins and cephalosporins and their BLI combinations required a skin test prior to administration in most hospitals in China. Due to the prohibited use of quinolones in children, these phenomena might lead to physicians preferably prescribing the monobactams when encountering cases of allergy or potential allergy and for safety reasons in children.
Most of the resistance rates stabilized with time in this study. Moreover, most of the resistance rates were similar to the levels reported in ISPED, despite the annual resistance trends not being statistically analyzed by ISPED.Citation3,Citation22–24 As expected, E. coli was highly sensitive to carbapenems, corroborating to the national level,Citation25 and the resistance rates presented a declining trend in our study. According to CHINET, the integrated data of children and adults exhibited that the rates of CRAB were >50% from 2010–2021.Citation25–27 Although the rates of CRAB were all <50% in this study period, the trend was significantly increasing and the resistance rate was up to 48.9% in 2021. Inconsistence with previous study that there was a significant decreased trend in the resistance rates of E.cloacae to carbapenems,Citation8 there was an obvious upward trend in our study; however, our result was in agreement with the CHINET data. These findings implied that we should focus on the two carbapenems-resistant bacteria in children.
Our results showed that increased consumption of the carbapenems was significantly associated with rising resistance rates of A. baumannii to carbapenems, which was in accordance with a multicenter study with data from 153 tertiary hospitals in China.Citation13 Previous studies from high-income countries, such as Korea and Saudi Arabia, also had similar results that increasing resistance of A. baumannii to carbapenems was correlated to carbapenems exposure.Citation28,Citation29 Moreover, the resistance rate of E. cloacae to carbapenems was positively correlated with carbapenems consumption in our study. However, a contradictory result was detected in a tertiary hospital in China from 2012 to 2019.Citation8 As mentioned above, the main factor was the resistance rate of E. cloacae to carbapenems in different trends, while the consumption of carbapenems showed increasing trends, which provided opposite statistical results. Furthermore, one study conducted by another tertiary hospital in another region in China demonstrated that carbapenem was an independent risk factor for infection of imipenem-heteroresistant E. cloacae.Citation30
Under selective antibiotic pressure, P. aeruginosa clinical isolates have a remarkable capacity for acquiring new resistance mechanisms,Citation16 which included expressing metallo-enzymes that are active against the most stable of the β-lactam classes, the carbapenems.Citation31 Therefore, the antibiotics of β-lactam classes and carbapenems could have a mutual effect on the resistance of P. aeruginosa to these antibiotics. The current results demonstrated a significant positive association between the consumption of carbapenems and the resistance of P. aeruginosa to ceftazidime, which was consistent with a previous study in Germany.Citation14 In addition, previous studies from middle-income countries, such as China and Serbia, showed that the resistance rate of P. aeruginosa to carbapenems had a positive correlation with the usage of antipseudomonal third-generation cephalosporins and β-lactam, respectively.Citation10,Citation17 As mentioned above, these could be attributed to the mutual effect on the resistance of P. aeruginosa to the antibiotics of β-lactam classes and carbapenems. Furthermore, the upward resistance rate of P. aeruginosa to ceftazidime was closely related to the increasing consumption of C/BLI combinations in this study, which might imply this similar effect even when combining BLI.
As previously mentioned, the increasing consumption of carbapenems was strongly associated with the increasing resistance rates of A. baumannii to carbapenems and E. cloacae to carbapenems. Not only that, this study found that the usage of the C/BLI combinations and monobactams had positive correlations with the resistance rates of A. baumannii to carbapenems and E. cloacae to carbapenems, respectively. These phenomena might be partially explained by the fact that resistance to one antimicrobial agent is related to cross-resistance to other antibiotics.Citation10 Similarly, these could be regarded as the phenomena of multidrug-resistance. Additionally, biofilm production that could be induced by low-dose, sub-inhibitory, and nonlethal concentrations of antibiotics in various pathogens, including the A. baumannii and E. cloacae,Citation32–35 which could contribute to increase the tolerance to antibiotics, should be one of multidrug-resistant factors.Citation36–38 The increasing usage of C/BLI combinations related to the rising carbapenems-resistance rates of A. baumannii corroborates to the previous study;Citation8 however, the association of consumption of C/BLI combinations with the carbapenems-resistance rates of E. cloacae in our study was inconsistent to that result in the study described previously.Citation8 As the similar reason analyzed above, the different trends of resistance rates of E.cloacae to carbapenems in the two studies should be the reason of the contradictory result. Due to the scarcity of research on this correlation between C/BLI combination usage and the resistance rate of E. cloacae to carbapenems, further studies are required to substantiate this association. Typically, monobactams and carbapenems belonged to the special-restriction antibiotics in China, with an extremely strong effect on the Gram-negative bacteria. Therefore, the increasing usage of monobactams could result in the rising carbapenems-resistance rates of some Gram-negative bacteria, which might partially explain the positive association between the monobactams and the carbapenems-resistance rates of A. baumannii and E. cloacae in the current study. Whatever, the C/BLI combinations, monobactams, and carbapenems should be administered under stricter restrictions in children.
Nevertheless, the present study has several limitations. First, it was a single-center study. Although multicenter monitoring networks for antimicrobial resistance, including the data from adults and children, have been established in China, data on antibiotics consumption were not fully included and may vary widely across the hospitals. Second, the antibiotics use may be one of the multiple interactive factors for the development of antimicrobial resistance. The mechanisms underlying antimicrobial resistance were extremely complicated, including the inherent, acquired, and adapted factors, such as impermeability of the outer membrane, mutation or the acquisition of new genetic material, and the specific environmental signal (for example, stress, growth state, pH, concentrations of ions, nutrient conditions, and sub-inhibitory levels of antibiotics).Citation39 These could explain why not all antibiotics were verified to correlate with selected antimicrobial resistance in our study. Even so, various antibiotics and doses should be used rationally because even the sub-inhibitory concentrations and low doses of the antibiotics could induce biofilm production in various bacteria, causing further antimicrobial resistance.Citation32–35 Third, this was a retrospective study; hence, some confounders, such as the change in the length of hospital stay, infection control practices, and certain factors influencing antimicrobial resistance as mentioned above, could not be evaluated. Therefore, multicenter and well-designed studies are required to substantiate the present findings and elucidate the correlation between antibiotics consumption and antimicrobial resistance.
Conclusions
This study demonstrated a significant positive association between consumption of antibiotics and specific antimicrobial resistance rates. These findings suggested the directions to pursue in controlling the prevalence of certain resistant bacterial strains in children, which need to be verified in future studies.
Disclosure
The authors declare there are no conflicts of interest regarding the publication of this paper.
Additional information
Funding
References
- Tacconelli E, Sifakis F, Harbarth S, et al. Surveillance for control of antimicrobial resistance. Lancet Infect Dis. 2018;18(3):e99–e106. doi:10.1016/s1473-3099(17)30485-1
- Alawi MM, Darwesh BM. A stepwise introduction of a successful antimicrobial stewardship program. Experience from a tertiary care university hospital in Western, Saudi Arabia. Saudi Med J. 2016;37(12):1350–1358. doi:10.15537/smj.2016.12.15739
- Fu P, Leiyan H, Wang C, et al. Antimicrobial resistance profile of clinical isolates in pediatric hospitals in China: report from the ISPED Surveillance Program in 2019. Chin J Evid Based Pediatr. 2021;16(01):43–49. doi:10.3969/j.issn.1673-5501.2021.01.002
- Enane LA, Christenson JC. Global emerging resistance in pediatric infections with TB, HIV, and gram-negative pathogens. Paediatr Int Child Health. 2021;41(1):65–75. doi:10.1080/20469047.2020.1853350
- Hu F, Wang M, Zhu D, Wang F. CHINET efforts to control antimicrobial resistance in China. J Glob Antimicrob Resist. 2020;21:76–77. doi:10.1016/j.jgar.2020.03.007
- Laxminarayan R, Duse A, Wattal C, et al. Antibiotic resistance-the need for global solutions. Lancet Infect Dis. 2013;13(12):1057–1098. doi:10.1016/s1473-3099(13)70318-9
- Wushouer H, Zhang ZX, Wang JH, et al. Trends and relationship between antimicrobial resistance and antibiotic use in Xinjiang Uyghur Autonomous Region, China: based on a 3 year surveillance data, 2014–2016. J Infect Public Health. 2018;11(3):339–346. doi:10.1016/j.jiph.2017.09.021
- Liang C, Zhang X, Zhou L, Meng G, Zhong L, Peng P. Trends and correlation between antibacterial consumption and carbapenem resistance in gram-negative bacteria in a tertiary hospital in China from 2012 to 2019. BMC Infect Dis. 2021;21(1):444. doi:10.1186/s12879-021-06140-5
- Zeng S, Xu Z, Wang X, et al. Time series analysis of antibacterial usage and bacterial resistance in China: observations from a tertiary hospital from 2014 to 2018. Infect Drug Resist. 2019;12:2683–2691. doi:10.2147/idr.S220183
- Zou YM, Ma Y, Liu JH, et al. Trends and correlation of antibacterial usage and bacterial resistance: time series analysis for antibacterial stewardship in a Chinese teaching hospital (2009–2013). Eur J Clin Microbiol Infect Dis. 2015;34(4):795–803. doi:10.1007/s10096-014-2293-6
- Bronzwaer SL, Cars O, Buchholz U, et al. A European study on the relationship between antimicrobial use and antimicrobial resistance. Emerg Infect Dis. 2002;8(3):278–282. doi:10.3201/eid0803.010192
- Mutnick AH, Rhomberg PR, Sader HS, Jones RN. Antimicrobial usage and resistance trend relationships from the MYSTIC Programme in North America (1999–2001). J Antimicrob Chemother. 2004;53(2):290–296. doi:10.1093/jac/dkh039
- Yang P, Chen Y, Jiang S, Shen P, Lu X, Xiao Y. Association between antibiotic consumption and the rate of carbapenem-resistant Gram-negative bacteria from China based on 153 tertiary hospitals data in 2014. Antimicrob Resist Infect Control. 2018;7:137. doi:10.1186/s13756-018-0430-1
- Lepper PM, Grusa E, Reichl H, Högel J, Trautmann M. Consumption of imipenem correlates with beta-lactam resistance in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2002;46(9):2920–2925. doi:10.1128/aac.46.9.2920-2925.2002
- Wang H, Wang H, Yu X, et al. Impact of antimicrobial stewardship managed by clinical pharmacists on antibiotic use and drug resistance in a Chinese hospital, 2010–2016: a retrospective observational study. BMJ Open. 2019;9(8):e026072. doi:10.1136/bmjopen-2018-026072
- Baditoiu L, Axente C, Lungeanu D, et al. Intensive care antibiotic consumption and resistance patterns: a cross-correlation analysis. Ann Clin Microbiol Antimicrob. 2017;16(1):71. doi:10.1186/s12941-017-0251-8
- Mladenovic-Antic S, Kocic B, Velickovic-Radovanovic R, et al. Correlation between antimicrobial consumption and antimicrobial resistance of Pseudomonas aeruginosa in a hospital setting: a 10-year study. J Clin Pharm Ther. 2016;41(5):532–537. doi:10.1111/jcpt.12432
- Guidelines for atc classification and ddd assignment 23rd edition (2020); 2020. Available from: https://www.whocc.no/atc_ddd_index/. Accessed September 15, 2022.
- Weinstein MP, Lewis JS. The clinical and laboratory standards institute subcommittee on antimicrobial susceptibility testing: background, organization, functions, and processes. J Clin Microbiol. 2020;58(3). doi:10.1128/jcm.01864-19
- Klein EY, Van Boeckel TP, Martinez EM, et al. Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc Natl Acad Sci U S A. 2018;115(15):E3463–E3470. doi:10.1073/pnas.1717295115
- Van Boeckel TP, Gandra S, Ashok A, et al. Global antibiotic consumption 2000 to 2010: an analysis of national pharmaceutical sales data. Lancet Infect Dis. 2014;14(8):742–750. doi:10.1016/s1473-3099(14)70780-7
- Fu P, Wang C, Yu H, et al. Antimicrobial resistance profile of clinical isolates in pediatric hospitals in China: report from the ISPED Surveillance Program, 2017. Chin J Evid Based Pediatr. 2018;13(06):406–411. doi:10.3969/j.issn.1673-5501.2018.06.002
- Fu P, Wang C, Yu H, et al. Antimicrobial resistance profile of clinical isolates in pediatric hospitals in China: report from the ISPED Surveillance Program, 2018. Chin J Evid Based Pediatr. 2019;14(05):321–326. doi:10.3969/j.issn.1673-5501.2019.05.001
- Leiyan H, Fu P, Xia W, et al. Antimicrobial resistance profile of clinical stains isolated from children in China: a report from the ISPED Program of 2020. Chin J Evid Based Pediatr. 2021;16(06):414–420. doi:10.3969/j.issn.1673-5501.2021.06.002
- Hu F, Guo Y, Yang Y, et al. Resistance reported from China antimicrobial surveillance network (CHINET) in 2018. Eur J Clin Microbiol Infect Dis. 2019;38(12):2275–2281. doi:10.1007/s10096-019-03673-1
- Resistance reported from China antimicrobial surveillance network (CHINET) in 2021; 2022. Available from: https://www.chinets.com/Data/AntibioticDrugFast. Accessed September 15, 2022.
- Hu FP, Guo Y, Zhu DM, et al. Resistance trends among clinical isolates in China reported from CHINET surveillance of bacterial resistance, 2005–2014. Clin Microbiol Infect. 2016;22(Suppl 1):S9–S14. doi:10.1016/j.cmi.2016.01.001
- Kim YA, Park YS, Youk T, Lee H, Lee K. Abrupt increase in rate of imipenem resistance in acinetobacter baumannii complex strains isolated from general hospitals in Korea and correlation with carbapenem administration during 2002–2013. Ann Lab Med. 2018;38(2):179–181. doi:10.3343/alm.2018.38.2.179
- Abdallah M, Badawi M, Alzaagi I, Issa KN, Rasheed A, Alharthy A. Effect of short-term carbapenem restriction on the incidence of non-pseudomonal multi-drug resistant Gram-negative bacilli in an intensive care unit. J Chemother. 2019;31(5):261–266. doi:10.1080/1120009x.2019.1601802
- Zhou Y, Jia X, He J, Xia Y. Study on clinical characteristics and risk factors for infection of Imipenem-heteroresistant Enterobacter cloacae. Chin Med Herald. 2019;16(16):147–150.
- Rice LB. Challenges in identifying new antimicrobial agents effective for treating infections with Acinetobacter baumannii and Pseudomonas aeruginosa. Clin Infect. 2006;43(Suppl 2):S100–S105. doi:10.1086/504487
- Avila-Novoa MG, Solís-Velázquez OA, Rangel-López DE, González-Gómez JP, Guerrero-Medina PJ, Gutiérrez-Lomelí M. Biofilm formation and detection of fluoroquinolone- and carbapenem-resistant genes in multidrug-resistant acinetobacter baumannii. Can J Infect Dis Med Microbiol. 2019;2019:3454907. doi:10.1155/2019/3454907
- Donadu MG, Mazzarello V, Cappuccinelli P, et al. Relationship between the biofilm-forming capacity and antimicrobial resistance in clinical acinetobacter baumannii isolates: results from a laboratory-based in vitro study. Microorganisms. 2021;9(11). doi:10.3390/microorganisms9112384
- Kaplan JB. Antibiotic-induced biofilm formation. Int J Artif Organs. 2011;34(9):737–751. doi:10.5301/ijao.5000027
- Yuksel FN, Karatug NT, Akcelik M. Does subinhibitory concentrations of clinically important antibiotic induce biofilm production of Enterococcus faecium strains? Acta Microbiol Immunol Hung. 2018;65(1):27–38. doi:10.1556/030.64.2017.041
- Jepsen K, Falk W, Brune F, et al. Prevalence and antibiotic susceptibility trends of selected enterobacteriaceae, enterococci, and candida albicans in the subgingival microbiota of German periodontitis patients: a retrospective surveillance study. Antibiotics. 2022;11(3). doi:10.3390/antibiotics11030385
- McCarthy H, Rudkin JK, Black NS, Gallagher L, O’Neill E, O’Gara JP. Methicillin resistance and the biofilm phenotype in Staphylococcus aureus. Front Cell Infect Microbiol. 2015;5:1. doi:10.3389/fcimb.2015.00001
- Khasawneh AI, Himsawi N, Abu-Raideh J, et al. Status of biofilm-forming genes among Jordanian nasal carriers of methicillin-sensitive and methicillin-resistant Staphylococcus aureus. Iran Biomed J. 2020;24(6):386–398. doi:10.29252/ibj.24.6.381
- Christaki E, Marcou M, Tofarides A. Antimicrobial resistance in bacteria: mechanisms, evolution, and persistence. J Mol Evol. 2020;88(1):26–40. doi:10.1007/s00239-019-09914-3
