Abstract
Background and objectives
Atherosclerosis causes reduction of the oxygen supply to structures in the far arterial wall, provoking the release of factors that drive angiogenesis of vasa vasorum, including VEGF. Other studies have revealed the inflammatory response in atherosclerosis and the role of platelet factor 4 (PF4) as an anti-angiogenic chemokine through the inhibition of VEGF. This cross-sectional study aims at measuring the effect of atherosclerosis assessed through carotid intima-media thickness (CIMT) against plasma VEGF levels in patients with post-acute thrombotic stroke.
Materials and methods
CIMT was assessed sonographically using GE Logiq S6 with 13 MHz frequency linear probe. VEGF-A plasma levels were measured using enzyme-linked immunosorbent assay (ELISA) method. Differences among variables were compared statistically. The data were analyzed using Pearson correlation.
Results
A total of 25 patients with post-acute thrombotic stroke were identified in days 7 to 90. CIMT thickening was indicated in 88% of patients (1.202 ± 0.312 mm), while an increase in plasma VEGF was identified in all patients (178.28 ± 93.96 ng/mL). There was no significant correlation between CIMT and plasma VEGF levels in patients with post-acute thrombotic stroke (p=0.741). A significant correlation was recognized between CIMT and total cholesterol (p=0.029) and low-density lipoprotein (p=0.018).
Conclusion
There were no significant correlations between CIMT and plasma VEGF levels in patients with post-acute thrombotic stroke. However, plasma VEGF increased in patients with thrombotic stroke. CIMT measurement is a promising noninvasive modality to assess the vascular condition of patients with stroke and diabetes, while plasma VEGF cannot specifically assess vascular condition as it can be triggered by ischemic conditions in tissues of the whole body.
Keywords:
Introduction
Stroke is the leading cause of death and disability worldwide. In Indonesia, the average age of stroke patients is 58.8 years old and stroke is the leading cause of a high mortality rate in people above 50 years old.Citation1–Citation3 The number of stroke patients is inclined to increase every year, not only among elderly people, but also young and productive people.Citation4 The most common type of stroke is thrombotic stroke with atherosclerosis as the most common cause.Citation5,Citation6 In atherosclerosis, thickening of the intima causes a decrease in the supply of oxygen to the far arterial wall, causing ischemia in blood vessels which provokes the release of factors stimulating angiogenesis of vasa vasorum, such as EPO, VEGF, and Ets-1.Citation7 Other studies have shown the existence of inflammatory responses in the atherosclerotic process, such as the role of PF4 which inhibits the degradation of low-density lipoprotein (LDL), facilitating the oxidation of LDL, recruiting monocytes, and facilitating their differentiation into macrophages. In addition, platelet factors also act as an anti-angiogenic chemokine by inhibiting VEGF.Citation8 Differences in the theory of relationship between atherosclerosis and VEGF emphasize the examination of the relationship between atherosclerosis and plasma VEGF levels assessed by carotid artery ultrasound.
Angiogenesis denotes a vital process in the growth and development of tissues which also takes place in pathological conditions, such as stroke, malignancy, inflammation, and diabetes mellitus.Citation7,Citation8 Currently, treatment for stroke which amplifies angiogenic and neurogenic processes has been developed.Citation9 In Indonesia, the blood test for VEGF is not yet widely available. This research aims at describing the effects of atherosclerosis examined through carotid intima-media thickness (CIMT) on the angiogenic process examined through the levels of VEGF, which seems to be able to assist clinicians in assessing vascular health, so as to provide management and selection of appropriate therapy.
Methods
Research subjects
The research design was observational analytic. The data were collected cross-sectionally from in patients and out patients with post-acute thrombotic stroke in days 7 to 90 in Dr. Saiful Anwar General Hospital Malang, Indonesia. The research subjects were 25 patients who were chosen consecutively.
Inclusion criteria
Patients with clinically diagnosed post-acute thrombotic stroke identified through computed tomography scan or magnetic resonance imaging.
Patients must be willing to participate in the research (by filling in informed consent form).
For patients with loss of consciousness/Glasgow Coma Scale of less than 15, the consent was obtained from authorized family.
Exclusion criteria
Patients who had received intra-arterial thrombolytic therapy.
Patients who were agitated which causes difficulties in carotid ultrasound examination.
Patients with myocardium infarction and malignancy.
Place and time of research
This research was conducted at Radiology and Neurology Units for in patients and out patients at Dr. Saiful Anwar General Hospital Malang and at Physiology Laboratory of Faculty of Medicine, Universitas Brawijaya.
Materials and tools
Materials and tools used in this research were USG GE Logiq S6 with linear probe (5–13 MHz) and enzyme-linked immunosorbent assay (ELISA) with VEGF-A Elab science kit.
Working technique and informed consent
This research was approved by the Medical Research Ethics Committee of Dr. Saiful Anwar General Hospital Malang with certificate no. 400/12/K.3/302/2016. Patients provided written informed consent prior to the examination and participation in this study.
Procedures
Carotid ultrasonography was performed under the supervision of two radiology specialists with background experience of more than 5 years. Measurements were taken at the bilateral carotid artery in three sites, namely the common carotid artery (1 cm distal segments before the bulb), the bulb, and the proximal internal carotid artery (1 cm proximal segment after branching) on the thickest CIMT by excluding plaque protruding into intravascular. The results were averaged.
In the same day, an amount of 3 cc venous blood sampling was performed on cubital vein location and then put into ethylenediaminetetraacetic acid tubes. The blood was then centrifuged and kept frozen until all the samples were collected and analyzed concurrently using ELISA with VEGF-A Elabscience kit at the Physiology department of University of Brawijaya.
Secondary data were obtained from medical records of patients comprising ages, the onset of stroke, results of blood lipid examination, previous stroke history, and history of diabetes mellitus.
Statistical analysis
All the data were recorded in a log book and stored as computer files. The relations between CIMT and plasma VEGF levels were tested using Pearson correlation with confidence level of 95%, α = 0.05, and is significant when p<0.05.
Results
In a 3-month period, 25 research subjects who met the inclusion criteria were gained. They comprised 40% male and 60% female patients. The age ranged from 46 to 82 years old with the majority ranging from 51–60 years (40%). For most patients (88%) this was their first stroke and 24% of patients had a history of diabetes mellitus ().
Table 1 Distribution of patients based on research variables
Following data normality test, Pearson correlation test was performed which resulted in the coefficient and significance as shown in .
Table 2 Correlation between CIMT and plasma VEGF levels
The result presented in indicates no apparent significant correlation between CIMT and plasma VEGF levels (p=0.741).
demonstrates the means of CMIT assessed with one-way analysis of variance which resulted in a significant difference by age group. Comparative analysis on multiple post hoc tests exhibits a result of significant difference in the age group <50 years and 51–60 years old (p=0.005), while the differences in other age groups were not significant. also displays no difference in CIMT by sex, history of diabetes mellitus, and earlier stroke.
Table 3 Comparison of average CIMT by sex, age group, history of diabetes, and history of previous stroke
From , it can be seen that there is no significant difference based on the average VEGF by sex, age group, history of diabetes mellitus, and history of stroke with p>0.05.
Table 4 Comparison of average VEGF by sex, age group, history of diabetes, and history of previous stroke
exhibits a significant correlation between CIMT with total cholesterol and LDL with p<0.05. As for profile of other fats, such as high-density lipoprotein and triglycerides, no significant correlation emerges. showed correlation beetwen CIMT and plasma VEGF and showed sonographic examination in one patient.
Figure 1 Curve of linear correlation between CIMT and plasma VEGF.
Abbreviation: CIMT, carotid intima-media thickness.
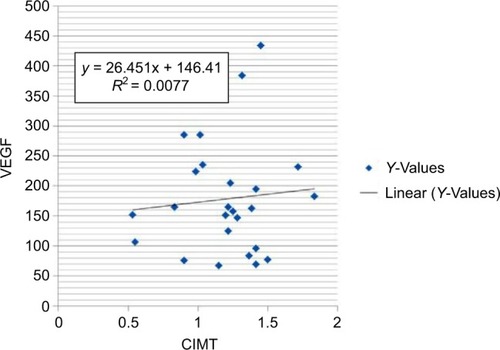
Figure 2 Sonographic examination of carotid arteries in one patient, from this figure we can see intima-media thickness measurement, carotid bulb measurement, and spectral Doppler.
Abbreviations: IMT, intima-media thickness; ICA, internal carotid artery; CCA, common carotid artery.
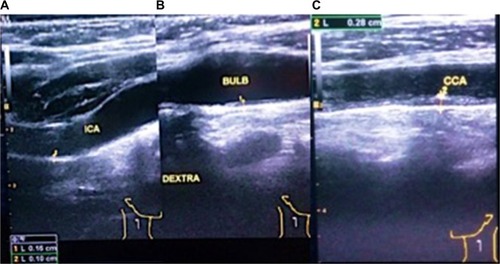
Table 5 Correlation between CIMT and lipid profile
Discussion
In this study, from a total of 25 patients, CIMT thickening was diagnosed in 22 patients (88%). CIMT thickening is not directly related to the incidence of stroke. Instead, it is associated with the increased risk of stroke. The measurement illustrates what happens to blood vessels per individual. Similarly, the rate of change in CIMT in a certain period of time illustrates how the development of atherosclerosis changes at all times.Citation10
Based on the results of Pearson correlation test, there was no significant correlation between plasma VEGF levels and the means of CIMT measurements obtained from six locations: right and left common carotid arteries, right and left bulbs, and right and left internal carotid arteries. This can be explained by a number of possibilities. The increased plasma VEGF was stimulated by nonspecific processes of tissue ischemia. VEGF synthesis is stimulated when cells undergo oxygen or glucose deficiency, or in inflammatory reactions.Citation11 In thrombotic stroke, both ischemia in blood vessels and ischemia in brain tissues occur and provoke VEGF expressions. Research by Yulinda et al examined a correlation between IMT thickness and VEGF in a mouse model in which aortic IMT was examined under microscopes, and VEGF levels were examined with immunohistochemical methods resulting in more specific description of VEGF levels in blood vessels.Citation12 This study did not allow the examination of VEGF by immunohistochemistry. Yet, another study by Hiyama et al used subject patients with endarterectomy in order that VEGF could be examined immunohistochemically and a correlation between the characteristics of the plaque with VEGF expression could be acquired.Citation13
In terms of statistical analysis, all research samples showed elevated levels of plasma VEGF and most had CIMT thickening. Differences in the values among abnormal levels were not regarded as significant. If an x, y scatter graph was made to illustrate the linearity of the relationship between CIMT with plasma VEGF levels, an R2-value of 0.007 would be obtained accordingly. That means only 0.7% of the relationships can be explained using these variables, while the remaining 99.3% of the relationships must be explained through other variables that were not examined in the present research.
International reference for VEGF preparation has not been enforced thus far. Immunoassays are preferred in clinical practices even though it may just detect VEGF epitopes with no biological activities. The emphasis is that ELISA antibody selectively detects free VEGF. Changes in the concentration of free VEGF genuinely describe the production of relative VEGF toward degradation or the change in the binding of protein carrier.Citation11 However, this study had employed VEGF levels in plasma, instead of serum, in which the release of VEGF in the platelets and other blood cells during the coagulation process occurred. More careful observations of the concentration of VEGF serum were able to provide further illustrations about the amount of blood platelet in the synthesis of peripheral tissues.Citation11
The results of this research did not indicate significant differences in the means of CIMT according to history of previous stroke(s). Still, the mean values of CIMT in patients with a history of more than one stroke were descriptively discovered to be higher (1.311 ± 0.258 mm) compared to the history of first stroke (1.190 ± 0.321 mm). This is in conformity with the Rotterdam study which involved 7,983 healthy subjects.Citation9 They used CIMT measurements followed by stroke incidence for an average follow-up period of 2.7 years, from which gradual increased risks of stroke incidence due to increased CIMT were detected. Odds ratio for stroke per 0.163 mm standard deviation increase was 1.41.Citation9 Similarly, the result of Eigenbrodt et al’s study revealed that CIMT thickening is related to the risk of stroke even after an adjustment of stroke risk factors (hazard ratio [HR]=3.7, 95% confidence interval [CI]=1.9–7.4 in males and HR=5.7, 95% CI=1.7–19 in females).Citation10 Insignificance of the statistical analysis in this study may be caused by differences in the design as the Rotterdam study was a cohort study.
Similarly, differences in the mean values of CIMT were assessed based on the history of diabetes mellitus. This study found no significant difference between the mean values of CIMT in patients with a diabetes history and in patients with no diabetes history. A study by Lee et al found an association between increased CIMT and plaque score with ischemic stroke in patients with diabetes mellitus. However, after the adjustment for risk factors for cerebrovascular disease, CIMT, and plaque no longer had a significant association with ischemic stroke.Citation14 This descriptive study found that average CIMT in patients with diabetes was higher (1.372 ± 3.88 mm) than in patients with no history of diabetes (1.151 ± 2.75 mm).
The role of VEGF and low-intensity inflammatory process in post-acute ischemic stroke patients remains controversial. A study by Berezin and Lisovaya suggested that increased circulating VEGF was associated with cumulative cardiovascular incidence within 1 year.Citation15 Research by Matsuo et al argued that higher VEGF levels in atherothrombotic stroke, therefore, were associated with better outcomes than the low levels of VEGF in post-acute thrombotic stroke. Further, the research found that high levels of VEGF in embolic stroke were associated with worse outcomes.Citation16 In this current study, evaluation of patients’ clinical conditions was not performed. Likewise, the cross-sectional research design did not lead to finding information about the relationship between VEGF and clinical outcomes of patients. The plausibility in embolic stroke is that the wider area of ischemic brain and the higher of VEGF expressions which resulted in worse clinical outcome.
In this present study, a significant difference in the average VEGF according to diabetes mellitus history was unidentified. This is in contrast with the research by Mahdy et al in which VEGF serum increased significantly in patients with diabetes mellitus with micro- and macrovascular complications.Citation17 Even so, the descriptive statistical analysis showed a trend of increased VEGF in patients with a history of diabetes mellitus (212.28 ± 101.93 pg/mL) compared to patients without a history of diabetes (167.54 ± 91.53 pg/mL). These significant differences may be due to the study design distinction in which Mahdy et al employed a case–control approach.
This study identifies significant correlations between the mean values of CIMT with total cholesterol and LDL levels in blood. This can be explained as due to the process of atherosclerosis, which started with the accumulation of oxidized LDL in the matrix below the layer of endothelial cells of blood vessels which stimulates the recruitment of monocytes.Citation18 Atherosclerotic plaques were initially seen as CIMT thickening then followed by the echogenic material coating the arterial lumen.Citation19
The result of analysis on correlation between plasma VEGF levels and LDL provides a negative yet insignificant correlation. This is consistent with the theory which suggests that VEGF expression is inhibited by LDL. The absence of significance of correlation is probably because the blood sampling for evaluation of VEGF levels and for lipid profile was taken at different times.
Conclusion
There were no significant correlations between CIMT and plasma VEGF levels in patients with post-acute thrombotic stroke. However, there was CIMT thickening in most (88%) patients and plasma VEGF levels increased in all patients with thrombotic stroke. CIMT measurement is a promising noninvasive modality to assess the vascular condition of patients with stroke and diabetes, while plasma VEGF cannot specifically assess vascular condition as it can be triggered by ischemic conditions in tissues of the whole body.
Disclosure
This work was supported by grants from Ministry of Health, Indonesia. The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
- XingCAraiKLoEHHommelMPathophysiologic cascades in ischemic strokeInt J Stroke20127537838522712739
- YueniwatiYYurinaVIndraMRThicker carotid intima media thickness in children with monocyte chemoattractant protein-1: A-2138T and A-2464G mutationNeurol Res Int2014201417653524860665
- YueniwatiYYurinaVSobahNRahayuEGenetic variations in the osteopontin promoters T-443C and G-156GG increase carotid intima-media thicknessInt J Gen Med2016911712227274305
- Yayasan stroke indonesia. sekilas tentang stroke2012 Availlabel from: http://www.yastroki.or.id/read.php?id=361Accessed October 3, 2016
- CaplanLRDiagnosis and the clinical encounterCaplan’s Stroke: A Clinical ApproachElsevier Inc20096486
- WolfPAKannelWBEpidemiology of strokeStroke5th ed.Elsevier2006198218
- XuJLuXShiGVasa vasorum in atherosclerosis and clinical significanceInt J Mol Sci2015165115741160826006236
- AidoudiSBikfalviAInteraction of PF4 (CXCL4) with the vasculature: a role in atherosclerosis and angiogenesisThromb Haemost2010104594194820806113
- BotsMLHoesAWKoudstaalPJHofmanAGrobbeeDECommon carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam StudyCirculation1997965143214379315528
- EigenbrodtMLEvansGWRoseKMBilateral common carotid artery ultrasound for prediction of incident strokes using intima-media thickness and external diameter: an observational studyCardiovasc Ultrasound2013112223768019
- JelkmannWPitfalls in the measurement of circulating vascular endothelial growth factorClin Chem200147461762311274009
- YulindaDYueniwatiYNursetaTVigna unguiculata reduces aortic intima-media thickness and increases aortic diameter and angiogenesis in ovariectomized ratsJournal of Experimental and Integrative Medicine2014428588
- HiyamaTTanakaTEndoSKomineKKudoTKobayashiHShiokawaYAngiogenesis in atherosclerotic plaque obtained from carotid endarterectomy: association between symptomatology and plaque morphologyNeurol Med Chir (Tokyo)201050121056106121206178
- LeeEJKimHJBaeJMRelevance of common carotid intima-media thickness and carotid plaque as risk factors for ischemic stroke in patients with type 2 diabetes mellitusAJNR Am J Neuroradiol200728591691917494669
- BerezinAELisovayaOAPredicted value of serial measurements of circulating vascular endothelial growth factor-1 in arterial hypertension patients after acute ischaemic strokeIntern Med20141711420
- MatsuoRAgoTKamouchiMClinical significance of plasma VEGF value in ischemic stroke – research for biomarkers in ischemic stroke (REBIOS) studyBMC Neurol2013133223566234
- MahdyRANadaWMHadhoudKMEl-TarhonySAThe role of vascular endothelial growth factor in the progression of diabetic vascular complicationsEye (Lond)201024101576158420508651
- MooreKJTabasIReview macrophages in the pathogenesis of atherosclerosisCell2011145334135521529710
- BluthEI8 – Ultrasound assessment of carotid plaquePelleritoJPolakJFIntroduction to Vascular UltrasonographyLondonElsevier Health Sciences2011147157
