Abstract
This case study aims to report an unresolved abdominal mass in an adult with cryptorchid testis and provide a review of related literature. We investigated a 54-year-old man who had cryptorchidism with a history of left orchiectomy 18 years prior. He was diagnosed with an intra-abdominal testicular mass after referring to the emergency ward with pelvic pain. The incidence of testicular cancer in undescended testicles is 40 times greater in the general population. In developed countries, the existence of undescended testicles in adult population is rare, which could be due to systematic practice of elective orchidopexy before the second year of life as well as orchiectomy in post-adolescent patients with undescended testicles. Despite these preventive measures, there are still some isolated cases of intra-abdominal testicular tumors in adults.
Introduction
During fetal development, the testes develop in the abdomen and later descend into the scrotal sac in the third trimester, usually between weeks 28 to 32. During the descent, it may be arrested anywhere along its tract (cryptorchidism) or may migrate into an abnormal position (ectopic testis). The most common sites of undescended testis are high scrotal, canalicular, abdominal, and bilateral.Citation1 Cryptorchidism, the most common congenital anomaly of the genitourinary tract in males, is encountered in 1% of boys.Citation2
In cryptorchid testicles, the incidence of testicular cancer is considered to be 3 to 48 times greater than in the general population. Testicular cancer is developed in 10% of the cases with undescendent testicles.Citation3 Various tumor markers are available in the form of alpha fetoprotein (α-FP), beta human chorionic gonadotrophin (β-HCG), lactate dehydrogenase (LDH), and placenta-like alkaline phosphotase (PLAP). They are helpful not only in making the diagnosis but also in formulating a management plan. Their sensitivity and specificity vary according to the type of testicular tumor.Citation4
Due to measures of prevention in force, it is uncommon to find cases of tumors in intra-abdominal testicles. This case report presents a new case of an adult patient with an intra-abdominal testicular tumor.
Case report
A 54-year-old patient, the father of three children, was referred to our hospital (Babol Clinic Hospital, in the North of Iran). He had been suffering from lower abdominal pain for 1 month. The pain was colicky in nature, mild in severity. It radiated to his left groin and was associated with occasional urinary frequency. He had normal bowel habits with no history of weight loss or change in appetite.
He had a history of herniorrhaphy and left orchiectomy about 18 years before. On initial examination in the emergency ward, his temperature was 38°C, heart rate 74/min, respiratory rate 18/min, and blood pressure 118/80 mmHg. On physical examination, his head and neck exam were within normal limits, and there was no lymph node enlargement. His chest was clear to auscultation, and no cardiac murmur was audible. Abdominal examination showed a pelviabdominal mass that was hard in consistency and mobile; there was, however, no hepatosplenomegally, no inguinal hernias, and no lymph node enlargement.
Scrotal examinations revealed a normal right testis and scrotum, whereas the left testis was neither palpable in the scrotum nor in the inguinal region. Clinical laboratory studies revealed a white blood count of 16,200 cell/mm3, with 92% neutrophils, 4% lymphocytes, 2% monocytes, and 2% eosinophil; hemoglobin of 14.6 g/dL; and a platelet count of 188,000/mm3. The aspartate aminotransferase was 30 IU/L, and the alanine aminotransferase was 28 IU/L. The erythrocyte sedimentation rate was 17 mm/h and C-reactive protein was ++. Kidney function tests were within normal limits. Tumor markers (β-HCG and α-FP) were normal too.
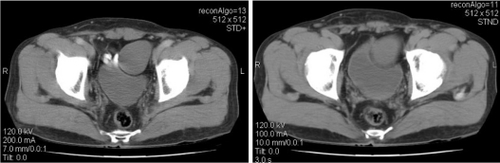
In ultrasonographic scanning, the suprapubic mass was demonstrated to be a large complex soft tissue mass (5.4 cm × 4.6 cm) with a hypoechoic area at the center. It is complemented with a CT scan observing an ovoid cystic mass with heterogeneous enhancement left anterolateral to bladder with 55 × 43 × 48 mm dimensions. There was negative evidence of the presence of adhesion between the mass and bladder but there was compressive effect on the bladder. Chest X-ray was normal.
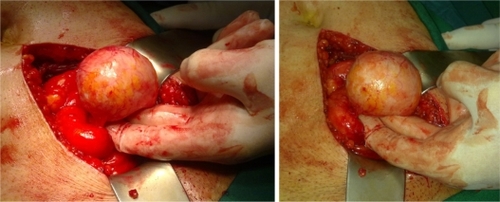
Laparotomy was done through lower midline incision and the total excision of the tumor was carried out. The resection was performed without complications, and the postoperative period was uneventful.
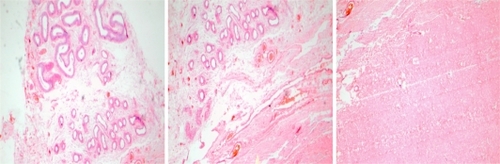
The pathological report revealed a massive complete fibrohyalinosis of testicular parenchyma with focal dystrophic calcification, but there was no evidence of malignancy (–).
Discussion
In humans, testes develop in the abdomen and normally descend into the lower portion of the scrotum during the third trimester. During the descent, it may be arrested anywhere along its tract (cryptorchidism) or may migrate into an abnormal position (ectopic testis). The most common sites of undescended testis are high scrotal (50%), canalicular (20%), and abdominal (10%), bilateral (10%).Citation1 The cancer risk of an ectopic testis is 40 times higher in a normal testis. Furthermore, an abdominal testis is four times more likely to undergo malignant degeneration than an inguinal testis.Citation2 The cancer of undescended testes usually peaks in the third or fourth decade of life.Citation2
Tumor in an abdominal testis is more likely to be seminoma, but tumors in testes previously corrected by orchipexy are more likely to be nonseminomas.Citation5
In ultrasonographic scanning, most GCTs (giant cell tumors) are solid, hypoechoic tumors. Cystic degeneration may be seen as representing necrosis and hemorrhage. CT and MRI show heterogenous soft tissue mass and retroperitoneal lymphadenopathy. CT shows calcifications better and MRI is superior in terms of detecting hemorrhage. Imaging and laboratory studies (α-FP and B-HCG) are quite useful in suggesting the diagnosis. Exploratory laparotomy and subsequent pathological examination are diagnostic too.Citation5
Undescended testes with intra-abdominal testes are more likely to be seminomas. Seminoma is a germ cell neoplasm of the testis. For this reason, testicular cancer should be considered as the differential diagnosis of an abdominal mass in patients with a nonpalpable testis.
Two hypotheses have been proposed to explain this association. The first one posits that local temperature elevation of an ectopic testis is, somehow, procarcinogenic. If this hypothesis is true, then orchidopexy (testis descend and fixation in the scrotum) could protect against cancer if the procedure is performed before precancerous cells differentiate to a critical point such as that of puberty. The second hypothesis posits that an underlying hormonal condition predisposes to both cryptorchidism and testicular cancer. If so, orchidopexy would not prevent the testicular cancer; and orchidectomy would be required.Citation2
A high intra-abdominal temperature has been incriminated as the cause of carcinogenesis in the testis. There may be a decrease in the spermatogenesis, Leidig cell abnormality, and delay in the development of the Sertoli cells in the testis, leading to infertility.Citation6 In our case, there was no evidence of sterility due to the testicular malfunction and the patient had three children. Painless enlargement of the testis, or abdominal mass, is the common mode of manifestation in a cryptorchid testis. Rarely, an abdominal testicular tumor can cause an acute abdomen, a massive abdominal mass, pain, and hematuria because of adjacent visceral infiltration.Citation6 Our patient had no such complications.
Various imaging modalities are available to diagnose and stage the condition. Classically, scrotal ultrasonography shows hypoechoic intratesticular mass in seminoma and at times with some calcification and cystic changes though mainly in nonseminomas. CT scanning of the abdomen and the pelvis is a very sensitive tool for the metastatic evaluation, which definitely helps plan the management. CT scan of the chest can usually be omitted unless there is an abnormal CXR finding.Citation7
In developed countries, the existence of undescended testicles in the adult population is rare, which is due to systematic practice of elective orchidopexy before the second year of life to prevent cancer and infertility. Orchidopexy does not eliminate cancer risk but allows an early diagnosis by making testicles accessible to exploration.Citation3
In conclusion, despite the elevated risk of testicular cancer in patients with intra-abdominal testicles, we consider it a low incidence disease. This could be due to standard practice of orchidopexy in pre-adolescent patients and orchiectomy in post-adolescents ones with cryptorchidism. Nevertheless, there are still some cases of intra-abdominal testicle tumors, which could presumably be avoided with the adoption of adequate prevention strategies.
Disclosure
The authors report no conflicts of interest in this work.
References
- DahnertWTesticular tumorRadiology review manual5th edWilliams and Wilkins2003925
- AlshyarbaMHA giant intra-abdominal testicular seminomaBiomed Res2010213227229
- Cristián PalmaCCristóbalBMaccioniRSeminoma in an adult cryptorchid testis (intra-abdominal): a case reportActas Urol Esp200731216016317645097
- ShresthaBBaidyaJLUnresolved abdominal massKathmandu Univer Med J20097258285
- ChandrasekharanLVAbdl GhaffarTVenkatramanaMRathSA case of teratocarcinoma In: Abdominal testis: a case reportInternet J Radiol200541 Available from: http://www.ispub.com/journal/the_internet_journal_of_radiology/volume_4_number_1_46/article/a_case_of_teratocarcinoma_in_abdominal_testis_a_case_report.html. Accessed 16 Nov, 2010
- HaqueMMSiddiqueABRabbaniABMGQuasemMARahmanAKMGRahmanMMSeminoma in undescended intra abdominal testis: a case reportTAJ: Journal of Teachers Association2005182131133
- JosephCPrestiJRGenital tumoursTanaghoEAMcAninchJWSmith’s general urology17th edNew York, NYLange Medical Books/McGraw-Hill, Medical Publishing Division2008375382