Abstract
Background
Drug rash with eosinophilia and systemic symptoms (DRESS) syndrome is characterized by cutaneous drug eruption, eosinophilia, and systemic symptoms. The syndrome is difficult to diagnose due to its clinical heterogeneity and long latency period (2–6 weeks).
Case report
This paper describes a 73-year-old man who presented with a rash that started 1 week prior to his presentation. The rash was associated with fever, dyspnea, and cough. He was admitted for pneumonia and started on intravenous antibiotics. After 3 days, he became confused and developed multiorgan dysfunction. Work-up for possible hematologic disorders, autoimmune diseases, and pneumonia was negative. One month prior to the onset of the rash, allopurinol had been prescribed for asymptomatic hyperuricemia. The allopurinol was stopped and corticosteroids were started; 2 days later, the patient became afebrile and the dyspnea resolved. He was diagnosed with DRESS syndrome, which is associated with high mortality.
Conclusion
The recent introduction of a drug followed by a rash, multiorgan dysfunction, and eosinophilia should raise the suspicion of DRESS syndrome. Early cessation of the introduced drug is key to survival. Clinicians should be aware of this potential adverse reaction when prescribing any new drug, including allopurinol.
Introduction
Drug rash with eosinophilia and systemic symptoms (DRESS) syndrome is characterized by cutaneous drug eruption, eosinophilia, and systemic symptoms (lymphadenopathy, hepatitis, interstitial nephritis, interstitial pneumonitis, and/or carditis).Citation1 This paper describes a patient with DRESS syndrome caused by allopurinol, the clinical presentation of which mimicked community-acquired pneumonia.
Case report
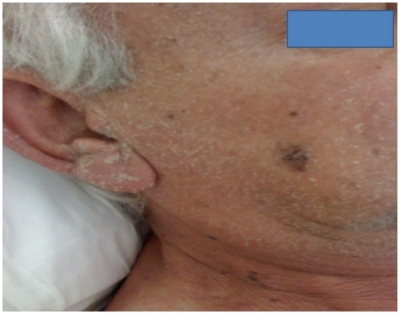
A 73-year-old man presented with a 1-week history of rash, which first appeared on the trunk and then spread to the face and upper extremities ( and ). Two days later, the rash symmetrically involved the lower extremities () and fever and chills began. He complained of shortness of breath with mild, nonproductive cough. He was anxious and dyspneic upon presentation. He denied any weight loss, night sweats, headache, abdominal pain, chest pain, or urinary symptoms. He had a history of hypertension, coronary artery syndrome, dyslipidemia, and had received coronary artery bypass surgery 3 years before. The patient was a heavy smoker (50 pack-years), drank alcohol socially, and had no history of illicit drug use. His medications included aspirin 75 mg per day, atenolol 50 mg per day, simvastatin 40 mg per day, and bezafibrate (a fibric-acid derivative available in Europe) 200 mg three times per day, which had been started 5 years prior. Allopurinol for hyperuricemia at 300 mg per day was started 1 month prior to presentation.
The patient was born in the USA and had immigrated to England during childhood. On presentation, he was in the USA visiting family. He was married and in a monogamous relationship with his wife. He was retired and did not own any pets nor was he aware of any tick or flea bites. There was no history of asthma or rash, nor any known allergies.
On examination, his heart rate was 90 beats/minute, respiratory rate 20 breaths/minute, blood pressure 150/70 mmHg, temperature 38.5°C, SpO2 90% on room air and 96% on 2 L/minute nasal cannula oxygen. He had periorbital edema; a scaling, confluent erythematous rash all over his face; scleral erythema; and crusting of the lips. A macular rash covered the trunk and upper extremities, slightly involved the palms, spared the scalp, and became more confluent and purpuric over the lower extremities (sparing the soles). There were bilateral wheezing and crackles in both lower lung fields. Meningeal signs were absent. The remainder of the examination was normal. Laboratory data included white blood cell count of 8500/*109/L with 68% neutrophils and 12% eosinophils, alanine transaminase 210 U/L, aspartate aminotransferase 165 U/L, blood urea nitrogen 19 mg/dL, and creatinine 1.7 mg/dL. Chest X-ray showed bilateral interstitial infiltrates with left lower lobe atelectasis (). Urine analysis was normal.
The patient was admitted to a regular ward for pneumonia treatment and started on ceftriaxone 2 g intravenous once daily and levofloxacine 750 mg intravenous once daily. On the second day, sputum Gram stain showed squamous epithelial cells and a fungal wet preparation showed no organisms. The patient continued to be febrile for the next 2 days, and became confused with increased shortness of breath and more wheezing and crackles on chest exam. Cultures of the blood and urine were sterile. A urine test for Legionella antigen and a serum test for antibodies to Legionella pneumophilia were negative. Salmonella antigen, Brucella-blocking antibodies, viral hepatitis panel (hepatitis A, hepatitis B, hepatitis C), and Epstein–Barr virus immunoglobulin levels were all normal; Weil–Felix test for rickettsia was negative. Stool for parasites was negative. Immunoglobulin E level was also normal.
The allopurinol was stopped and he was started on methylprednisolone 60 mg intravenous every 8 hours. Two days later, the patient became afebrile, the dyspnea resolved, the rash improved significantly, and there was complete resolution of the kidney and hepatic injury. The eosinophil count also returned to a normal value after 5 days ().
Table 1 Patient’s laboratory data
Discussion
One outstanding feature of this case is eosinophilia. Eosinophilia occurs in hematologic, allergic, autoimmune, and infectious diseases.Citation2 The eosinophilia in this case was associated with a cutaneous rash, hepatitis, kidney dysfunction, mental status changes, and interstitial pneumonitis. In this clinical context (eosinophilia with multiorgan involvement), the differential diagnoses would be: Churg–Strauss syndrome (CSS), idiopathic hypereosinophilic syndrome, eosinophilic leukemia, or drug-induced eosinophilia. The actual presentation of an “asthma-like” exacerbation with eosinphilia is consistent with CSS, but does not fulfill the criteria for this diagnosis. Furthermore, the patient had no history of asthma or sinus abnormality and skin lesions in CSS usually appear as subcutaneous nodules on the extensor surfaces.Citation3 Migratory or transient pulmonary opacities detected radiographically, along with evidence of a peripheral neuropathy, are required for the diagnosis of CSS. The absence of immature eosinophils in the peripheral blood smear makes the diagnosis of eosinophilic leukemia unlikely. Hypereosinophilic syndrome is a diagnosis of exclusion when no apparent cause of eosinophilia is diagnosed, which was not the case in this patient.Citation4 The recent introduction of allopurinol raised the suspicion of DRESS syndrome.
DRESS syndrome, previously known as drug-induced hypersensitivity, is characterized by fever, cutaneous eruption, and involvement of several internal organs – most commonly the liver and, to a lesser extent, the kidneys, lungs, and brain. The cutaneous reaction usually begins 2–6 weeks after the drug is started and is due to a delayed-type hypersensitivity reaction.Citation5 The rash presents as a widespread erythematous eruption on the face, upper trunk, and upper extremities and is accompanied by fever, facial and periorbital edema, and/or exfoliative dermatitis. Eruption may become purpuric on the legs and rarely involves the palms and soles, and virtually never involves the scalp.Citation5 Scaling and/or desquamation may occur with healing. The most common drug class implicated is anticonvulsants, including phenytoin, lamotrigine, and carbamazepine; other drugs known to cause this syndrome include allopurinol, minocycline, dapsone, and sulfonamides. Citation6 Although the pathophysiology is still unknown, different factors have been postulated in DRESS syndrome’s etiology – mainly immunologic and genetic factors and metabolite accumulation. Drugs with reactive metabolites can modify cellular proteins and trigger an autoimmune response against the skin or liver cells.Citation7 The metabolism of allopurinol and consequent accumulation of oxypurinol, especially in patients with renal insufficiency or those on thiazides diuretics, may predispose the patient to an immunologic reaction.Citation8 A recent study in the Han Chinese population found that HLA-B*5801 is a genetic marker for the DRESS syndrome caused by allopurinol.Citation9 Also, allopurinol’s inhibition of the enzyme purine nucleoside phosphorylase, which results in defective T-cell-mediated immunity, is due to a genetic predisposition. One study suggests a role for the human herpes virus 6 in the pathogenesis of DRESS syndrome.Citation7 Early cessation of the drug implicated in the development of DRESS syndrome will result in a better outcome. Corticosteroids have been used for treatment of DRESS syndrome, but their role remains controversial. Unfortunately, a review of the literature found that 80% of patients with allopurinol-induced DRESS syndrome were treated for asymptomatic hyperuricemia.Citation10 Currently, the only indications for allopurinol include symptomatic hyperuricemia, such as nephrolithiasis and gout, and prophylaxis for urate nephropathy with chemotherapy in neoplastic diseases.
Conclusion
A drug allergy should always be suspected in a patient presenting with a whole-body rash and eosinophilia, especially if a new medication was recently started. Allopurinol-induced DRESS syndrome is associated with significant mortality (10%). The use of allopurinol for accepted indications and dose adjustment for renal dysfunction are the only ways to decrease the incidence of the potentially fatal toxic effects of this medication.
Disclosure
Written informed consent was obtained from the patient discussed for publication of this case report and accompanying image. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
The authors declare that they have no competing interests in this work.
References
- WolfRDavidoviciBMatzHMahlabKOrionESthoegerZMDrug Rash with eosinophilia and systemic symptoms versus Stevens-Johnson syndrome – a case that indicates a stumbling block in the current classificationInt Arch Allergy Immunol200614130831016940741
- TefferiABlood eosinophilia: a new paradigm in disease classification, diagnosis, and treatmentMayo Clin Proc200580758315667033
- SchwartzRAChurgJChurg-Strauss syndromeBr J Dermatol19921271992041390162
- RoufosseFCoganEGoldmanMThe hypereosinophilic syndrome revisitedAnnu Rev Med20035416918412525672
- EshkiMAllanoreLMusettePTwelve-year analysis of severe cases of drug reaction with eosinophilia and systemic symptoms: a cause of unpredictable multiorgan failureArch Dermatol2009145677219153346
- JeungYJLeeJYOhMJChoiDCLeeBJComparison of the causes and clinical features of drug rash with eosinophilia and systemic symptoms and stevens-johnson syndromeAllergy Asthma Immunol Res2010212312620358026
- IchicheMKieschNDe BelsDDRESS syndrome associated with HHV-6 reactivationEur J Intern Med20031449850014962704
- SullivanJRShearNHThe drug hypersensitivity syndrome: what is the pathogenesis?Arch Dermatol200113735736411255340
- HungSIChungWHLiouLBHLA-B*5801 allele as a genetic marker for severe cutaneous adverse reactions caused by allopurinolProc Natl Acad Sci U S A20051024134413915743917
- ArellanoFSacristánJAAllopurinol hypersensitivity syndrome: a reviewAnn Pharmacother1993273373438453174