Abstract
Acute intramural hematoma of the colon is a rarely encountered clinical condition with diverse precipitating factors. Different acute and chronic complications emerge following hematoma formation, mandating high clinical suspicion for early diagnosis and optimum management. CECT represents the cornerstone for the proper demonstration of colonic hematomas and possible detection of complications as well as the underlying etiology. There are multiple strategies for management of intramural hematoma and treatment should be tailored according to the etiology and the clinical condition of the patient, reserving surgical intervention for unstable or complicated cases. Endoscopic management of colonic hematomas offers a promising minimally invasive modality with potential safety and efficacy.
Introduction
Intramural hematoma may occur at any site from the esophagus to the rectum, with the duodenum being the most common site for it.Citation1 On the other hand, intramural hematoma of the colon is a rare entity with only few cases reported where sigmoid colon is the typical site.Citation2 Spontaneous colonic hematoma is an uncommon disease and it is usually diagnosed at a late stage.Citation3 It has been most commonly associated with blunt trauma. However, other risk factors including bleeding diathesis, malignancies, chemotherapy, vasculitis, collagen diseases, H. Pylori infection and colonic diverticular disease can be incriminated.Citation1,Citation4 Additionally, a case report of a huge submucosal hematoma complicating an angiodysplastic lesion in the sigmoid colon was reported in the literature.Citation5 Rarely did it occur as an iatrogenic sequale, or as a rare complication of anticoagulant therapy or vaginal delivery.Citation2 According to Zhu et al and Yavari et al, despite the rarity of bowel hematoma incidence, it should be considered as an adverse drug reaction of low molecular weight heparin or warfarin therapy, especially among cases presenting with gastrointestinal symptoms with or without prolonged INR.Citation6,Citation7 Gastrointestinal hematomas are estimated to occur in only 1 in every 250,000 anti-coagulated patients; with small intestinal hematoma reported in 1/2500 anticoagulated patients per year and far fewer reported colonic hematoma cases.Citation8,Citation9 Colonic trauma can occur in only 0.5–5% of those exposed to blunt abdominal injuries,Citation10 with a very uncommon incidence of colonic intramural hematoma. It is suggested that the taenia coli plays a major protective role in cases of blunt trauma resulting in rupture of intramural vessels as it prevents the extravasation of blood into the bowel wall, which explains the rare incidence of hematoma in the colon.Citation1
Diagnosis is majorly accomplished radiologically with contrast-enhanced computed tomography (CECT) scan or magnetic resonance imaging. Surgical management used to be the standard treatment for traumatic acute colonic intramural hematoma in most of the reported cases. On the other hand, conservative management was reserved for very few cases where no local or systemic signs of hemodynamic instability were detected.
Pathophysiology
Traumatic acute intramural hematoma is thought to originate from blood reaching the bowel wall from mesentery as a result of crushing forces inducing shearing of bowel layers and rupture of terminal blood vessels.Citation11 Another postulated mechanism leading to bowel intramural hematoma might be the rapid decompression of splanchnic circulation due to decreased abdominal pressure, causing the bowel to rupture and bleed in cases on therapeutic anticoagulation therapy.Citation6 The most involved bowel segments with traumatic acute hematoma are those residing between retroperitoneally free and fixed structures; with duodenum being the most commonly affected region followed by ascending colon or caecum.Citation12
Diagnosis and Complications
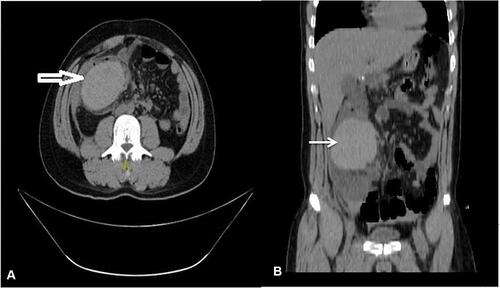
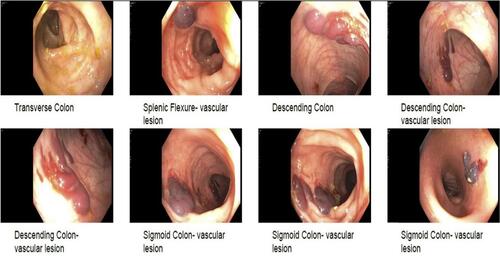
The clinical symptoms of colonic hematoma are usually nonspecific and can vary from mild, crampy abdominal pain to hemorrhagic shock. Nausea and vomiting are detected in 50% of cases and are related to intestinal obstruction.Citation6 Physical examination might reveal rebound tenderness, abdominal guarding, hematochezia, or signs of bowel obstruction.Citation2 Early and late complications can arise as a result of intramural hematoma. At the acute phase, it might lead to blood loss by free rupture of hematoma into the peritoneum causing hemodynamic instability, bowel gangrene, intestinal obstruction, and intussusception.Citation12 On the other hand, late complications can be in the form of stenotic lesion causing luminal obstruction due to fibrosis. Contrast-enhanced CT (CECT) along with colonoscopy is the modality of choice for diagnosis of colonic intramural hematoma.Citation13 It has been suggested that non-contrast CT should be performed for oral and intravenous contrast medium application, as contrast-enhanced CT alone may mask the presence of intramural hemorrhage.Citation6 Computed tomography diagnostic criteria of colonic hematomas include eccentric or circumferential wall thickening, intramural hyper-density, narrowing of the lumen and intestinal obstruction, as shown in .Citation14 In addition to defining hemorrhagic areas, CT can also detect possible complications as well as the underlying etiology leading to hematoma formation. Two additional signs can be detected in intramural hematoma: “coiled spring” and “pseudokidney” signs.Citation15 Ultrasonography and CT show 71.4% and 80–100% sensitivity, respectively, for detecting such findings.Citation16 Rigid proctoscopy is considered a precious adjunctive diagnostic modality which demonstrates colonic intramural hematomas as round-shaped, dark-reddish submucosal masses or lesions often causing luminal obstruction of the lumen.Citation17 On the other hand, colonoscopy could reveal a localized, submucosal mass with variable mucosal manifestations, as shown in , which demonstrates a case of colonoscopy-induced intramural hematomas in a 16-year-old patient most likely secondary to looping of colonoscope and loop reduction maneuvers.Citation2,Citation18 Different signs can be illustrated by barium studies denoting the presence of intramural hematoma, including coiled spring or picket fence sign or stacked coin sign.Citation11 Repeated abdominal ultrasonography can assist in follow up of patients.
Management
The diagnosis of intramural hematoma poses a challenge, particularly in the absence of clinical suspicion. An early recognition is mandatory for a positive outcome.Citation19 The optimum treatment should be tailored according to the underlying cause in addition to the patient’s clinical condition.Citation2 Conservative management can be considered in case of clinically and hemodynamically stable cases without signs of peritoneal affection.Citation20 It consists of anticoagulation cessation with reversal of coagulation if the patient was anticoagulated, total parenteral nutrition and intravenous hydration for resuscitation.Citation2,Citation6 Nevertheless, the patient should be under close observation for alarming manifestations including acute anemia, evidence of expanding hematoma, and abdominal tenderness, guarding or rigidity. Usually, a minority of cases of colonic hematomas stabilize under conservative management alone. It should be noted that identification of patients with self-limiting intramural hematoma from those with more severe pathology represents a serious clinical challenge as routine clinical examination is insufficient to identify serious life-threatening cases and even a simple hematoma may also present with hyperthermia, leukocytosis and peritoneal signs.Citation17
Indications of surgical intervention are variable and include evidence of ongoing arterial bleeding into hematoma detected in CECT arterial phase, evolving signs of peritonitis or a failure of stabilization despite conservative management.Citation21 In patients undergoing laparotomy, a diversion stoma is one treatment option.Citation3 It should be mentioned that diverting colostomies were required in about 80% of cases with distal colonic hematomas, as demonstrated in many case series.Citation22
It is of utmost importance to manage a hematoma in an early stage as this prevents intestinal obstruction and obviates the need for surgery and bowel resection.Citation16 Alternative treatment modalities have been described in case reports and series including endoscopic drainage; however, it requires colonic wall viability and it can cause relief of the “tamponade effect” of the hematoma.Citation23 Another valuable line of treatment includes selective mesenteric embolization in patients with active bleeding into the colonic wall, with an 85% success rate, and an overall 20% of complications as a result of the procedure. A recent review of the literature demonstrates a shift in the management of colonic hematomas over the past 50 years where surgical management was the treatment of choice;Citation24 however, since 2010 there has been a recent trend towards more conservative management.Citation6,Citation7,Citation16
Endoscopic Management
Endoscopic procedures can be incriminated in many cases of acute intramural hematomas of the gastrointestinal tract, especially in those receiving anticoagulant therapy or those with concomitant hematological disorders.Citation25 Although an intramural hematoma can be primarily associated with an invasive endoscopic procedure, including biopsy or therapeutic procedures, an incidence of spontaneous intramural hematomas during a diagnostic colonoscopy has been reported in a few cases.Citation13
While CT offers the most sensitive diagnostic modality of intramural colonic hematoma, colonoscopy could be an adjunctive method revealing a localized submucosal lesion.Citation2 Echo-endoscopy or endoscopic ultrasound (EUS) can be a valuable diagnostic tool in cases of intramural hematoma at an accessible location of the lesion. EUS can assist in determining the wall thickness and involvement and evaluating intra-lesional structures.Citation26
By reviewing different case reports of colonic hematoma, it was illustrated that, as mentioned earlier, management options vary from conservative management in stable patients and surgical management for unstable or complicated patients.Citation3,Citation16 Nevertheless, there remain some cases where endoscopy might pose a potential role not only in diagnosis but also in offering a minimally invasive interventional modality for management of colonic hematoma. However, performing colonoscopy in the setting of an intramural hematoma might further complicate the hemorrhage as the tissue contained in hematoma can be fragile.Citation1
Kwon et al reported a case of colonic hematoma which was developed in the sigmoid colon during colonoscopy. It was supposed to be precipitated by a continuous suctioning process applied during the procedure due to poor bowel preparation. At the suspected site of bleeding, endoscopic clips were applied, which successfully led to cessation of hematoma growth, followed by a dual knife which was used to excise and evacuate the hematoma with an electrosurgical unit and Endocut I setting as a power source.Citation27
Similarly, Ulla-Rocha et al reported two cases of perigastric and perirectal hematomas, which were successfully managed endoscopically with fine needle aspiration (EUS-FNA)-guided drainage and stent placement, highlighting the safety and efficacy of endoscopic intervention in management of colonic hematoma.Citation28
Another case of intramural hematoma but in the duodenum was approached endoscopically using a similar perspective by Kwon et al. The site of the suspected hematoma was punctured and incised with an electrical needle knife. After the site was punctured, a large amount of liquefied dark red-colored material gushed out from the hematoma, relieving the luminal obstruction and stenosis.Citation23
In conclusion, intramural hematoma of the colon is a rare clinical entity which has variable precipitating factors and non-specific manifestations. High clinical suspicion is required and early recognition helps to avoid complications and abates the need for unnecessary surgical interference. Endoscopic management of intramural hematoma might offer an alternative less-invasive modality and has been reported in sporadic cases with successful and favorable outcomes.
Disclosure
The authors report no conflicts of interest in this work.
References
- Vecchio R, Cacciola E, Figuera M, et al. Idiopathic intramural hematoma of the right colon. A case report and review of the literature. Int J Surg Case Rep. 2019;60:16–20. doi:10.1016/j.ijscr.2019.05.004
- Wang J, Sun X, Shi H, Cao D. Intramural hematoma of colon: case report of 2 cases. Medicine. 2020;99(10):e19404. doi:10.1097/MD.0000000000019404
- Lobo L, Koudki R, Kishan Prasad H, Shetty B. Colon obstruction due to an anticoagulant induced intramural haematoma; a rare case report. J Clin Diagn Res. 2013;7(4):739. doi:10.7860/JCDR/2013/5283.2899
- Limmer AM, Clement Z. Extensive small bowel intramural haematoma secondary to warfarin. J Surg Case Rep. 2017;2017(3):rjx044. doi:10.1093/jscr/rjx044
- Shimizu T, Koike D, Nomura Y, Ooe K. Colonic angiodysplasia with a huge submucosal hematoma in the sigmoid colon. Case Rep Surg. 2016;2016:4. doi:10.1155/2016/3457367
- Zhu Y, Wang C, Xu C, Liu J. Case report: spontaneous intramural hematoma of the colon secondary to low molecular weight heparin therapy. Front Pharmacol. 2021;12(12):598661. doi:10.3389/fphar.2021.598661
- Yavari N, Majdi Nassab F, Tajvidi MA, Shirani S, Shirani S, Ahmadi TSH. Spontaneous descending colon hematoma due to a rare complication of warfarin therapy: a case report. Clin Case Rep. 2021;9(6):e04252. doi:10.1002/ccr3.4252
- Abdel Samie A, Theilmann L. Risk factors and management of anticoagulant-induced intramural hematoma of the gastrointestinal tract. Eur J Trauma Emerg Surg. 2013;39(2):191–194. doi:10.1007/s00068-013-0250-1
- Eek AK, Strøm BO, Bakkehøi G, Stenberg-Nilsen H. Anticoagulant-associated adverse drug reactions in 2013–15. Tidsskr nor Laegeforen. 2018;138(12):12–20.
- Carrillo EH, Somberg LB, Ceballos CE, et al. Blunt traumatic injuries to the colon and rectum. J Am Coll Surg. 1996;183(6):548–552.
- Hughes CE, Conn J Jr, Sherman JO. Intramural hematoma of the gastrointestinal tract. Am J Surg. 1977;133(3):276–279. doi:10.1016/0002-9610(77)90528-1
- Nozu T. Idiopathic spontaneous intramural hematoma of the colon: a case report and review of the literature. Clin J Gastroenterol. 2009;2(3):161–165. doi:10.1007/s12328-008-0061-9
- Katsurahara M, Horiki N, Kitade T, et al. Acute colonic intramural hematoma: a rare complication of colonoscopy. Endoscopy. 2014;46 Suppl 1 UCTN:E180–E181. doi:10.1055/s-0034-1365108
- Jebin Aaron D, Bhattarai S, Shaikh O, et al. Traumatic acute colonic intramural hematoma: a rare entity and successful expectant approach. Cureus. 2020;12(8):e9694. doi:10.7759/cureus.9694
- Kokabi N, Harmouche E, Xing M, et al. Specific radiological findings of traumatic gastrointestinal tract injuries in patients with blunt chest and abdominal trauma. Can Assoc Radiol J. 2015;66(2):158–163. doi:10.1016/j.carj.2014.11.003
- Kwon K, Cheung DY, Seo Y, et al. Supportive management resolved a colonic intramural hematoma in an anticoagulant user. Intern Med. 2014;53(14):1505–1509. doi:10.2169/internalmedicine.53.2358
- Rentea RM, Fehring CH. Rectal colonic mural hematoma following enema for constipation while on therapeutic anticoagulation. J Surg Case Rep. 2017;2017(1):rjx001. doi:10.1093/jscr/rjx001
- Chetan M, Kaliyann T, Mary L. Image: colonic hematoma complicating pediatric colonoscopy. J Pediatr Gastroenterol Nutr Rep. 2021;2(4):e128. doi:10.1097/PG9.0000000000000128
- Figueiredo J, Borges N, Pascoalinho J, Matos R. Giant intramural hematoma of the colon in acquired factor VIII inhibitor. Acta Med Port. 2019;32(9):614–617. doi:10.20344/amp.8519
- Akgul GG, Yenidogan E, Ozsoy Z, et al. Conservative management of large rectosigmoid perforation under peritoneal reflection: case report and review of the literature. Case Rep Surg. 2015;2015:4.
- Mohamed B, Mohamed AS, Philippe-Abrahim K, Robert C, Khaled K. Nontraumatic intramural hematomas in patients on anticoagulant therapy: report of three cases and overview of the literature. Afr J Emerg Med. 2014;4(4):e1–e4. doi:10.1016/j.afjem.2014.07.009
- Chaiteerakij R, Treeprasertsuk S, Mahachai V, Kullavanijaya P. Anticoagulant-induced intramural intestinal hematoma: report of three cases and literature review. J Med Assoc Thai. 2008;91(8):1285–1290.
- Kwon CI, Ko KH, Kim HY, et al. Bowel obstruction caused by an intramural duodenal hematoma: a case report of endoscopic incision and drainage. J Korean Med Sci. 2009;24(1):179–183. doi:10.3346/jkms.2009.24.1.179
- Calenoff L, Lounsbury F. Intramural hematoma of the sigmoid. Am J Roentgenol Radium Ther Nucl Med. 1969;107(1):170–174. doi:10.2214/ajr.107.1.170
- Liu Y, Yang S, Tong Q. Spontaneous intramural hematoma of colon. Clin Gastroenterol Hepatol. 2012;10:e38.
- Gravito-Soares E, Gravito-Soares M, Figueiredo P. An unusual cause of lower gastrointestinal bleeding. Gastroenterology. 2018;154(8):e12–3. doi:10.1053/j.gastro.2017.09.014
- Kwon CI, Kim DH, Hong SP. Immediate endoscopic management of an intramural hematoma developed during colonoscopy. Clin Endosc. 2017;50(5):508–509. doi:10.5946/ce.2017.037
- Ulla-Rocha JL, Vilar-Cao Z, Sardina-Ferreiro R. EUS-guided drainage and stent placement for postoperative intra-abdominal and pelvic fluid collections in oncological surgery. Therap Adv Gastroenterol. 2012;5(2):95–102. doi:10.1177/1756283X11427420