Abstract
Individuals presenting with sudden and focal neurological findings are usually suspected to have stroke. However, there are other conditions that can simulate stroke, which are often referred to as stroke mimics. Awareness and understanding these stroke-like disorders are of extreme importance as the treatment of each of them might be variable. We hereby briefly discuss these stroke mimics, common differentials, and key features to differentiate amongst the various causes of acute neurological event. Stroke is one of the neurological emergencies that needs urgent intervention to prevent significant mortality and morbidity. At the same time, it is important to realize the importance of other conditions which may mimic to stroke. In this letter, we aim to discuss a few key features that could probably help to distinguish stroke from mimickers thereby helping emergency doctors, neurologists, and hospitalists in streamlining the correct treatment at the earliest.
Keywords:
Prevalence of Stroke Mimics (Community vs Health Care Settings)
Stroke mimics accounts for approximately 25% of probable stroke admissions. Marot et al have reported 368 clinical episodes of presumed stroke, among which 50% were actual vascular episodes.Citation1 In another retrospective study published in 2019, Garg et al reported 27.3% of stroke mimics.Citation2 Interestingly, in another prospective study, Matuja et al recruited 1403 patients; among those, 30.6% were presumed to have a stroke. Only 6.6% of these were identified to have stroke mimics.Citation3
Hospital-based studies could have higher reported numbers of stroke mimics as compared to community-based study probably due to
Selection bias of having sicker patients with more vascular risk factors.Citation4
Observation and reporting bias in having higher reporting of stroke-like episodes, including change in cognition, dropping of the eyelid, and limb weakness while being closely monitored.Citation1,Citation5,Citation6
Meanwhile, community-based studies would report a lesser number of stroke episodes because of possible loss of continuous recruitment of patients and decreased health-seeking behavior. While the actual rates of stroke mimics continue to be diverse, it is irrefutable that stroke mimics continue to be a significant challenge to the treating clinician.Citation7,Citation8
Calling a Stroke “Stroke”
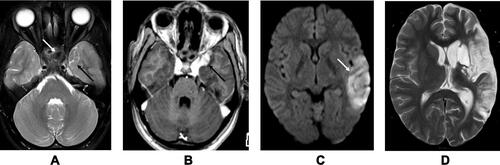
Computed tomography of the brain is routinely used in the assessment of stroke, as it facilitates the decision regarding the administration of thrombolytic agents. In the Marot et al’s study, only 2 of the stroke mimics received IV rt-PA.Citation1 In the study by Garg et al, all 33 patients with stroke mimics received rt-PA as per the treatment protocol.Citation2 With the significant mortality benefit offered by rt-PA, the harm of not administering the same to a patient is higher. However, the modality of imaging could influence the unnecessary administration of thrombolytic agent to patients at low risk in terms of clinical presentation and vascular risk profile. Magnetic Resonance Imaging (MRI) can not only show diffusion restriction but also identify granulomas, dilated Virchow robin spaces, cysts better, and differentiate them from a vascular event. Image 1 shows the MRI brain’s findings of a 20-year-old female with headache and acute onset of aphasia who had an initial non-diagnostic CT but later diagnosed to be angioinvasive aspergillosis with the contributory clue from MRI (). In a recent study by Matujia et al, improved rate of detection of mimics was secondary to better identification and differentiation of vascular events by MRI. In the absence of MRI, we agree that a detailed clinical history and examination would significantly influence the diagnosis of stroke in low-risk patients.
Figure 1 Angioinvasive aspergillosis in a 20-year-old female with headache and acute onset aphasia. (A) T2W axial section shows inflammatory changes in the sphenoid sinus (white arrow) with altered signal intensity in the adjacent medial aspect of the left temporal lobe (black arrow). (B) Post contrast T1W axial section shows enhancing area in the region of left temporal lobe signal abnormality. (C) Diffusion study shows an acute infarct in the left temporal lobe related to infective vasculitis of left middle cerebral artery (white arrow). (D) Follow up T2W axial section after 15 months shows chronic infarcts in the left MCA territory.
In high-risk patients, the role of administration of rt-PA in stroke mimics has been studied as well. Ahmed et al studied 72,582 patients from 485 US hospitals with suspected ischemic stroke who received alteplase.Citation9 Among all the recruited patients, only 3.5% of stroke mimics received alteplase. Intracranial hemorrhage and in-hospital mortality were 0.4%, and 0.8% in the mimics compared to 3.5% and 6.2% of patients with ischemic stroke.Citation9,Citation10
Identifying the Stroke Mimics and the Uncommon Causes of Stroke
In Marot et al’s study, 48.4% of stroke mimics did not get a definitive clinical diagnosis. This pattern was reported in the study by Ahmed et al as well.Citation9 A total of 61.3% of stroke mimics in their study had an uncertain diagnosis and missing details. Gomez et al included 4570 presumed stroke cases, among which 404 were diagnosed with stroke mimics. They used a broader differential diagnosis and identified an etiology in around 90% of patients.Citation11 Across studies identifying all the causes of stroke, mimics continue to be a challenge.Citation6 shows the multiple stroke mimics that have been reported in the literature.Citation12–Citation14,Citation15,Citation16 Future studies should incorporate broader differential and detailed workup.
Table 1 Various Stroke Mimics Described in the Literature
In conclusion, stroke mimics are reported all over the world. They continue to be a diagnostic challenge to the treating emergency physician, neurologist, and clinician. A detailed history, neurological examination, appropriate neuroimaging, laboratory findings, and a multidisciplinary approach would facilitate understanding of these mimics and optimal care of these patients.
Disclosure
The authors report no conflicts of interest in this work.
References
- Marot JE, Rebeiz T, Kramer C, et al. Neurological examination, rather than vascular risk factor assessment, serves to distinguish strokes from stroke mimics [published online ahead of print, 2020 Jul 17]. World Neurosurg. 2020:S1878-8750(20)31596-5. doi:10.1016/j.wneu.2020.07.075
- Garg R, Rech MA, Schneck M. Stroke mimics: an important source of bias in acute ischemic stroke research. J Stroke Cerebrovasc Dis. 2019;28(9):2475–2480. doi:10.1016/j.jstrokecerebrovasdis.2019.06.019
- Matuja SS, Khanbhai K, Mahawish KM, Munseri P. Stroke mimics in patients clinically diagnosed with stroke at a tertiary teaching hospital in Tanzania: a prospective cohort study. BMC Neurol. 2020;20(1):270. doi:10.1186/s12883-020-01853-7
- Sahu KK, Mishra AK, Lal A, Kranis M. An interesting case of expressive aphasia: enterococcus faecalis-related infective endocarditis complicating as septic emboli. QJM. 2020;113(2):146–147. doi:10.1093/qjmed/hcz169
- Vanjare HA, Mannam P, Mishra AK, et al. Brain imaging in cases with positive serology for dengue with neurologic symptoms: a clinicoradiologic correlation. AJNR Am J Neuroradiol. 2018;39(4):699–703. doi:10.3174/ajnr.A5544
- Mishra A, Binu A, Abraham G, Vanjare H, George T, Iyadurai R. Cerebrovascular injury following scorpion sting and snake envenomation: a case series. Can J Neurol Sci. 2018;45(6):669–674. doi:10.1017/cjn.2018.328
- Thomas VV, George T, Mishra AK, Mannam P, Ramya I. Lateral medullary syndrome after a scorpion sting. J Family Med Prim Care. 2017;6(1):155–157. doi:10.4103/2249-4863.214988
- Mishra AK, Sahu KK, George AA, Sargent J, Lal A. Cerebrovascular events in COVID-19 patients. Monaldi Arch Chest Dis. 2020;90(2). doi:10.4081/monaldi.2020.1341
- Ali-Ahmed F, Federspiel JJ, Liang L, et al. Intravenous tissue plasminogen activator in stroke mimics. Circ Cardiovasc Qual Outcomes. 2019;12(8):e005609. doi:10.1161/CIRCOUTCOMES.119.005609
- Mishra AK, Iyadurai R. Prehospital and hospital delays for stroke patients treated with thrombolysis: access to health care facility - still a bottle neck in stroke care in developing nation. Australas Emerg Care. 2019;22(4):227–228. doi:10.1016/j.auec.2019.07.003
- Avellaneda-Gómez C, Rodríguez Campello A, Giralt Steinhauer E, et al. Estudio descriptivo de los stroke mimics después de un estudio neurovascular completo [Description of stroke mimics after complete neurovascular assessment]. Neurologia. 2019;34(1):7–13. doi:10.1016/j.nrl.2016.10.006
- Mishra AK, Vanjare HA, Raj PM. Cryptococcal meningitis presenting as acute onset bilateral cerebellar infarct. J Neurosci Rural Pract. 2017;8(1):159–160. doi:10.4103/0976-3147.193537
- Mishra AK, Aaron S, Abhilash K, et al. Simple telephone call a feasible, useful and acceptable method of following up patients with cerebrovascular accidents: prospective Cohort study in South India. Int J Stroke. 2016;11(8):NP87–NP88. doi:10.1177/1747493016654486
- Ifergan H, Amelot A, Ismail M, Gaudron M, Cottier J-P, Narata AP. stroke-mimics in stroke-units. evaluation after changes imposed by randomized trials. Arq Neuropsiquiatr. 2020;78(2):88–95. doi:10.1590/0004-282x20190154
- Meng D, AlSaeed M, Randhawa J, Chen T. Retrosplenial stroke mimicking transient global amnesia. Can J Neurol Sci. 2021;12:1–7. doi:10.1590/0004-282x20190154
- Lim EYT, Swaminathan SK. Cerebral contrast staining mimicking parenchymal haemorrhage in a stroke patient. BMJ Case Rep. 2020;13(12):e236400.
