Abstract
Objective
To observe the relationship between the extrapancreatic necrosis volume and outcomes in patients with severe acute pancreatitis (SAP).
Methods
We retrospectively analyzed 125 patients with SAP admitted to Severe Acute Pancreatitis Treatment Center of Guizhou Province from August 2013 to August 2018. All patients had extrapancreatic necrosis. The general clinical data of patients, C-reactive protein (CRP) value within 72 hours of onset, Ranson score, organ failure within 3 days after onset, complications, outcomes, CT severity index (CTSI), extrapancreatic necrosis volume and other information were collected. The correlation between extrapancreatic necrosis volume and hospitalization time, ICU stay, hospitalization cost, and CRP value was analyzed. The incidence of complications was obtained from the electronic medical record system.
Results
The mean extrapancreatic necrosis volume was 680 ± 473 mL. The median length of hospital stay was 18.2 (3–76) days, and the ICU stay was 13.5 (3–66) days. The extrapancreatic necrosis volume was positively correlated with hospitalization time, ICU stay time, cost of hospitalization and CRP (P < 0.05). The extrapancreatic necrosis volume in organ failure group was significantly higher than that in non-organ failure group (P < 0.05). The extrapancreatic necrosis volume in patients with death was also higher than that in survival (P < 0.05). With the increase of extrapancreatic necrosis volume, the incidence of complications increased significantly. On the basis of extrapancreatic necrosis volume, the ROC curves yielded an AUC of 0.92 (95% CI: 0.83, 0.99) in predicting the mortality, which was higher than Ranson score (0.90, 95% CI 0.82–0.96) and CTSI (0.85, 0 95% CI 0.77–0.91).
Conclusion
With the increase of extrapancreatic necrosis volume, the incidence of complications increased significantly. The extrapancreatic necrosis volume has the potential to be used as a valuable tool to predict the poor outcome of acute pancreatitis.
Introduction
Acute pancreatitis (AP) is a common acute abdominal disease, with high mortality in severe acute pancreatitis (SAP). The implications of SAP not only embarrass the surgical and medical setting but also increase the health cost in the world.Citation1 The necrotizing pancreatitis is usually complicated by local and systemic complications, such as infection of pancreatic necrosis, which is associated with high morbidity and mortality rates.Citation2 Identifying the clinical course and outcome is fundamental for SAP prognosis.
In the past decade, some laboratory, clinical and radiological scoring systems have been created to predict the severity and outcome of SAP.Citation3 Currently, the most scoring systems are Ranson Criteria, Acute Physiology and Chronic Health Disease Classification System II (APACHE II) score, Bedside Index of Severity in Acute Pancreatitis (BISAP), and Atlanta and Balthazar classifications. C-reactive protein (CRP) is the most frequently studied in acute stage but is not practical since it produces meaningful results in 72 h.Citation4 Computed tomography (CT) or magnetic resonance imaging (MRI) also could not provide sufficient information to determine the severity since necrosis does not develop in the early stage.Citation4 Therefore, these scores have shortcomings in clinical applications.Citation5 Acute necrotic collection is the accumulation of liquid necrotic substances in and around the pancreas caused by abnormal activation and release of pancreatic enzymes in the early stage of SAP. A previous study showed that extrapancreatic fluid collection was an indicator for SAP and the extent of extrapancreatic fluid collections was significantly correlated with a severe outcome.Citation6 However, the study did not strictly distinguish the severity of acute pancreatitis, which may affect the prognosis of patients. Whether the volume of extrapancreatitis necrosis is closely related to the prognosis of SAP patients remains uncertain. The purpose of this study was to assess the extrapancreatic necrosis volume in predicting the outcome of SAP.
Materials and Methods
This study was performed with the approval of the Ethics Committee of Affiliated Hospital of Zunyi Medical University.
Patients
We performed a retrospective review of all patients admitted to the affiliated hospital of Zunyi Medical University between 2013 and 2018 with a confirmed diagnosis of AP and an early CT study. The diagnosis of SAP was based on the previous report.Citation7 Patients transferred from other hospitals to our hospital without abdominal CT were excluded from this study. General information, etiology, outcome parameters, CTSI and C-reactive protein (CRP) of patients were collected.
CT Technique
All CT examinations were performed by using a 16–detector row CT scanner (Sensation 16; Siemens, Erlangen, Germany). The method and parameter setting of CT scanning are consistent with a previous report.Citation7 All patients included in this study received early CT scan within 7 days after symptom onset. In our hospital, an abdomen CT scan is routinely performed in all patients with a confirmed diagnosis of AP, regardless of its severity. Patients who had been transferred from another hospital without an early CT study were not be included.
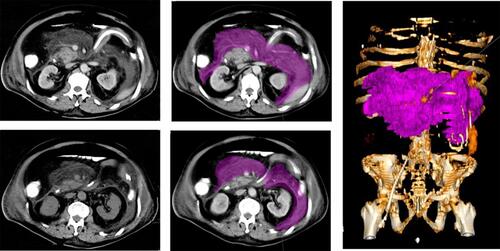
Measurement of Extrapancreatic Necrosis Volume
CT images were retrospectively reviewed on a system workstation (Syngo.via Workplace), and CTSI were calculated for each patient. Pancreatic necrosis was defined as an area of diminished or no enhancement of the pancreatic parenchyma after intravenous administration of contrast medium.Citation7 Based on CTSI, the severity was classified as mild (0–3 points), moderate (4–6 points) and severe (7–10 points). The volume of extrapancreatic necrosis was calculated with manual segmentation (Syngo.via Workplace, Siemens, Erlangen, Germany). Extrapancreatic necrosis included peripancreatic necrosis and contiguous retroperitoneal fat necrosis.Citation7 Necrotic tissues with peripancreatic or associated retroperitoneal fat tissue inflammation and liquid and solid components were considered as extrapancreatic necrotic tissue. Ascites are not included. The volume of extrapancreatic necrosis was expressed in milliliters. The patients’ CT images were used to record the intensity of pancreatic necrosis, and to calculate the CTSI scores. The pancreatic necrosis was defined as an area of diminished or no enhancement of the pancreatic parenchyma on CT. All abdominal CT images were reviewed by an experienced radiologist who had, at least, 6 years of experience. The radiologist was blinded to clinical data and the outcome parameters.
CRP levels at 48–72 hours after the onset were obtained from the medical records. Ranson’s score was evaluated within first 48 hours after symptom onset.
Statistical Analysis
All data were expressed as mean ± SD or 95% CI. Spearman rank correlation coefficient was used to analyze the correlation between the volume of extrapancreatic necrosis and other indexes. The volume of extrapancreatic necrosis between different groups was compared by non-paired t-test, P < 0.05 was statistically significant. Statistical analysis and mapping were performed by GraphPad prism 5.0.
Results
A total of 125 patients were included in this study, including 72 male and 53 female. The demographic and clinical characteristics are showed in . The average ICU stay was 13.5 days. CRP levels were obtained for all patients, and the mean value of CRP was 161 mg/L (). The mean extrapancreatic necrosis volume was 680 mL (range, 0–1650 mL, ).
Table 1 Baseline Demographic and Clinical Characteristics of 125 Patients
The Correlation Between Extrapancreatic Necrosis Volume and Hospital Stay, ICU Stay, Expense and CRP
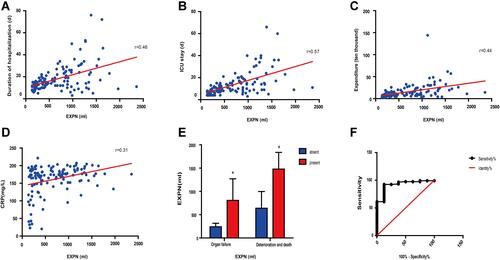
The mean hospital stay was 18.2 days, and the mean length of stay in ICU was 13.5 days. The volume of extrapancreatic necrosis was positively correlated with the length of hospital stay, r = 0.46, P < 0.05, . The volume of extrapancreatic necrosis was also positively correlated with the length of stay in ICU, r = 0.57, P < 0.05, . The extrapancreatic necrosis volume was positively correlated with hospitalization expenses, r = 0.44, P < 0.05, . The extrapancreatic necrosis volume was also positively correlated with CRP level, r = 0.44, P < 0.05, .
Figure 2 The correlation between extrapancreatic Necrosis Volume (EXPN) and hospital stay (A), ICU stay (B), expenditure (C) and CRP (D). Comparison of necrotic volume in patients with different outcome (E). ROC curves of the EXPN predictors in predicting mortality (F). *P<0.05, compared to absent group.
Comparison of Necrotic Volume in Patients with Different Outcome
Of the 125 patients, 97 patients had organ failure within 3 days of onset, and 28 patients had no organ failure. The volume of extrapancreatic necrosis in organ failure group was significantly higher than that in non-organ failure group (807.6 ± 462.5 vs 240.0 ± 75.4, P < 0.05). Of the 125 patients, 24 died. The extrapancreatic necrosis volume in death group was also higher than that in the survival group (1479.03 ± 58.9 vs 639.3 ± 355.2, P < 0.05), .
Relationship Between Extrapancreatic Necrosis Volume and Complications
According to the different extrapancreatic necrosis volume, these patients were divided into three groups: group A (n = 36) <300 mL; group B (n = 41) 300–800 mL; group C (n = 48) >800 mL. With the increase of extrapancreatic necrosis volume, the incidence of complications increased significantly ().
Table 2 Incidence of Complications in Different Groups
Extrapancreatic Necrosis Volume Used to Predict the Mortality
CTSI, Ranson score and extrapancreatic necrosis volume for the prediction of death in AP patients were evaluated by AUC analyses. The extrapancreatic necrosis volume had the highest AUC value in predicting the development of death (AUC 0.92, 95% CI 0.83–1.009, P<0.05, ), which was followed by Ranson score (AUC 0.90, 95% CI 0.82–0.96) and CTSI (AUC 0.85, 0 95% CI 0.77–0.91). The cutoff value of extrapancreatic necrosis volume in predicting the mortality was 1314 mL, which sensitivity was 92.44%, specificity was 87.50% () CTS.
Discussion
The patients included in this study were all patients treated in ICU. The mean patient age was 48.8 (16–83) years old, which is consistent with a previous report in China.Citation8 The most frequent aetiology was biliary in 58 patients (46.4%), which is nearly to a previous report.Citation9 The incidence rate of hyperlipidemic pancreatitis (26.4%) in the study is higher than that in a recent study in China (14.37%).Citation8 The high incidence rate of hyperlipidemic pancreatitis may be related to local eating habits (high-fat diet).
Alfonso et al had found that CRP had a significant association in predicting the severity of pancreatitis.Citation10 Cardoso et alCitation11 and Wilson et al confirmed that a CRP value of 150 mg/L could be taken as a cut off for predicting pancreatic fluid collection and necrosis.Citation12 In the study, the mean level of CRP was 161 mg/L, which is above 150 mg/L. Our results also showed that the extrapancreatic necrosis volume was also positively correlated with CRP level.
Previous studies suggest that the incidence of peripancreatic necrosis approximates to that of pancreatic necrosis.Citation13 A recent study suggested that extrapancreatic necrosis volume was found to be particularly better at predicting organ failure and infection.Citation6 In our study, the volume of extrapancreatic necrosis in organ failure group was also significantly higher than that in non-organ failure group. The extrapancreatic necrosis volume in death group was also higher than that in the survival group. However, this study did not use the volume of extrapancreatic necrosis to predict organ failure. In our study, the mean extrapancreatic necrosis volume was 680 mL, which is significantly higher than that in a recent report (246.42 mL).Citation6 The patients included in this study were all treated in ICU, and the severity of the disease may be more severe than those included in Çakar et al reported.Citation6
Bakker et al reported that the complications such as organ failure, developing infected necrosis, percutaneous/surgical intervention, and death were less frequent in the extrapancreatic necrosis group (P < 0.001).Citation13 In a similar study, Koutroumpakis et alCitation14 also had similar findings to the results of Bakker et al in terms of the need for intervention, development of infected necrosis, and duration of hospitalization. In our study, with the increase of extrapancreatic necrosis volume, the incidence of complications increased significantly, such as bleeding and AKI.
In most cases of AP, it is difficult to assess the severity clinically alone. In our study, the volume of extrapancreatic necrosis in organ failure group was significantly higher than that in non-organ failure group. The extrapancreatic necrosis volume in death group was also higher than that in the survival group. Therefore, extrapancreatic necrosis volume may be considered as an assessment tool to determine the severity of acute pancreatitis in the early phase. In addition, the necrotic volume was correlated with the length of hospital stay, ICU stay and hospital costs. Çakar et al also found that a moderate positive correlation between the extrapancreatic necrosis volume and the duration of hospitalization (r = 0.479 P = 0.0001).Citation6 Meyrignac et al found a strong positive correlation (r = 0.75, p = 0.0001).Citation7 Our findings suggest that the extrapancreatic necrosis volume may provide a higher positive likelihood and diagnostic odds ratio.
In this study, the mortality of SAP patients was 19.2%, which is higher than a previous study (14.6%). There are two possible reasons for the high mortality of SAP patients in this study. Some of the patients included in this study were patients transferred from primary hospitals, and these patients were already in serious condition when they were transferred to our hospital. In addition, the patients included in this study had extrapancreatic necrosis. AP is a heterogeneous and poorly understood disease, ranging from a mild clinical course to severe life-threatening complications.Citation15 Early evaluation of the severity of AP is essential to allow the clinician to predict patient outcome, estimate prognosis, and determine the need for ICU care. Therefore, the factors that predict mortality should be further explored to provide timely treatment for AP.
We further compared the AUC of Ranson score, CTSI score and extrapancreatic necrosis volume to predict the mortality. Yang et al found that in the assessment of mortality, the AUC of mCTSI was 0.839 (95% CI 0.721–0.957) in hyperlipidemic acute pancreatitis, which is similar to our results (0.85, 95% CI 0.82–0.96).Citation16 CTSI performed poorly compared to Ranson scoring systems in predicting the mortality in our study. In predicting the mortality, the AUC of extrapancreatic necrosis volume was higher than Ranson scoring and CTSI. Currently, it is difficult to predict the mortality of AP in the early stage. Hence, the extrapancreatic necrosis volume has the potential to be used as a valuable tool to predict the poor outcome of acute pancreatitis.
The study has several limitations. First, it was a single-center and retrospective study. Only 125 patients were included, and there is a need for a multi-center prospective study with a larger sample size to validate the predictive performance of extrapancreatic necrosis volume. Second, the relationship between the volume of peripancreatic necrosis and the degree of pancreatic necrosis was not observed in this study. The relationship between pancreatic necrosis and peripancreatic necrosis remains to be further clarified. Finally, Ranson’s score was evaluated within first 48 hours after admission in our study, while the CT scan was performed within 7 days after symptom onset. Although some radiologic scoring systemsCitation17 and extrapancreatitis necrosis volume are more accurate than Ranson score in predicting the severity of acute pancreatitis, there are also some defects in imaging evaluation. However, there is a lag in the imaging changes of pancreas or extrapancreatic tissues. In addition, the convenience of radiology scoring system is not as good as Ranson score because CT is not necessary for the diagnosis of AP. Hence, Ranson score is still a valuable tool for early prediction of the severity of AP.Citation18
Conclusions
The volume of extrapancreatic necrosis was positively correlated with the incidence of complications of SAP. The extrapancreatic necrosis volume has the potential to be used as a valuable tool to predict the poor outcome of acute pancreatitis.
Data Sharing Statement
The datasets used in the present study are available from the corresponding author (Xiaoyun Fu) on reasonable request.
Ethics Approval and Consent to Participate
This study was approved by the Ethical Committee of Affiliated Hospital of Zunyi Medical University, which waived the need for written informed consent from the participants, since the data were analysed anonymously. This study was conducted in accordance with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- Ouyang G, Pan G, Liu Q, et al. The global, regional, and national burden of pancreatitis in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. BMC Med. 2020;18:388. doi:10.1186/s12916-020-01859-5
- Whitcomb DC. Clinical practice. Acute pancreatitis. N Engl J Med. 2006;354(20):2142–2150. doi:10.1056/NEJMcp054958
- Papachristou GI, Whitcomb DC. Predictors of severity and necrosis in acute pancreatitis. Gastroenterol Clin North Am. 2004;33(4):871–890. doi:10.1016/j.gtc.2004.07.004
- Tenner S, Baillie J, DeWitt J, Vege SS. American college of gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108:1400–1415; 1416. doi:10.1038/ajg.2013.218
- Delrue LJ, De Waele JJ, Duyck PO. Acute pancreatitis: radiologic scores in predicting severity and outcome. Abdom Imaging. 2010;35(3):349–361. doi:10.1007/s00261-009-9522-y
- Cakar I, Keven A, Eseroglu E, Cubuk SM. Role of extrapancreatic necrosis volume in determining early prognosis in patients with acute pancreatitis. Abdom Radiol. 2020;45:1507–1516. doi:10.1007/s00261-019-02188-9
- Meyrignac O, Lagarde S, Bournet B, et al. Acute pancreatitis: extrapancreatic necrosis volume as early predictor of severity. Radiology. 2015;276:119–128. doi:10.1148/radiol.15141494
- Pu W, Luo G, Chen T, et al. A 5-Year Retrospective Cohort Study: epidemiology, etiology, severity, and outcomes of acute pancreatitis. Pancreas. 2020;49:1161–1167. doi:10.1097/MPA.0000000000001637
- Alberti P, Pando E, Mata R, et al. Evaluation of the modified computed tomography severity index (MCTSI) and computed tomography severity index (CTSI) in predicting severity and clinical outcomes in acute pancreatitis. J Dig Dis. 2021;22:41–48. doi:10.1111/1751-2980.12961
- Alfonso V, Gomez F, Lopez A, et al. [Value of C-reactive protein level in the detection of necrosis in acute pancreatitis]. Gastroenterol Hepatol. 2003;26:288–293. Spanish. doi:10.1016/S0210-5705(03)70358-6
- Cardoso FS, Ricardo LB, Oliveira AM, et al. C-reactive protein prognostic accuracy in acute pancreatitis: timing of measurement and cutoff points. Eur J Gastroenterol Hepatol. 2013;25:784–789. doi:10.1097/MEG.0b013e32835fd3f0
- Wilson C, Heads A, Shenkin A, Imrie CW. C-reactive protein, antiproteases and complement factors as objective markers of severity in acute pancreatitis. Br J Surg. 1989;76:177–181. doi:10.1002/bjs.1800760224
- Bakker OJ, van Santvoort H, Besselink MGH, et al. Extrapancreatic necrosis without pancreatic parenchymal necrosis: a separate entity in necrotising pancreatitis? Gut. 2013;62(10):1475–1480. doi:10.1136/gutjnl-2012-302870
- Koutroumpakis E, Dasyam AK, Furlan A, et al. Isolated peripancreatic necrosis in acute pancreatitis is infrequent and leads to severe clinical course only when extensive: a prospective study from a US tertiary center. J Clin Gastroenterol. 2016;50(7):589–595. doi:10.1097/MCG.0000000000000482
- Hori Y, Vege SS, Chari ST, et al. Classic chronic pancreatitis is associated with prior acute pancreatitis in only 50% of patients in a large single-institution study. Pancreatology. 2019;19(2):224–229. doi:10.1016/j.pan.2019.02.004
- Yang L, Liu J, Xing Y, et al. Comparison of BISAP, Ranson, MCTSI, and APACHE II in predicting severity and prognoses of hyperlipidemic acute pancreatitis in Chinese patients. Gastroenterol Res Pract. 2016;2016:1834256. doi:10.1155/2016/1834256
- Xie J, Xu L, Pan Y, Li P, Liu Y. Impact of visceral adiposity on severity of acute pancreatitis: a propensity score-matched analysis. BMC Gastroenterol. 2019;19(1):87. doi:10.1186/s12876-019-1015-z
- Ong Y, Shelat VG. Ranson score to stratify severity in acute pancreatitis remains valid - old is gold. Expert Rev Gastroenterol Hepatol. 2021;15:865–877. doi:10.1080/17474124.2021.1924058