Abstract
Introduction
Healthcare professionals’ beliefs and attitudes towards low back pain management play a significant role during treatment. This is a crucial aspect of primary care physicians working as a first point of contact for people seeking healthcare for low back pain.
Aim
To identify the beliefs and behaviors of frontline healthcare professionals (primary care physicians) working in the Riyadh region with regard to low back pain management.
Methods
A cross-sectional design was implemented, in which the Pain Attitude and Beliefs Scale (PABS) questionnaire was used along with a low back pain clinical vignette with some questions. The PABS assesses healthcare provider orientations toward low back pain with two subscales: biomedical and behavioral. In total, 400 primary care physicians working in the Riyadh region of Saudi Arabia were invited to participate.
Results
The responding primary care physicians (n = 72, response rate = 18%) provided an average score on the behavioral subscale (mean = 31.5±7.1) that was lower than that on the biomedical subscale (36.5±7.8) of the PABS. The lower scores in the biomedical subscale are associated with the using of clinical guidelines for low back pain management (χ2 (1) = 4.7, p = 0.03). Moreover, providing guideline-based advices regarding activity and work was more likely to come from those scoring above the mean in the behavioral subscale.
Conclusion
The results of this study show that Saudi Arabian primary care physicians manage their patients within a biomedical framework; there is some compliance to the current low back pain clinical guidelines among these physicians, with under/post-graduate education being needed for these professionals to adopt a more biopsychosocial framework during low back pain management.
Introduction
Low back pain is a significant musculoskeletal burden,Citation1 with a prevalence of 12% across the global population.Citation1 It is associated with sizeable socioeconomic losses and imposes a significant burden on society.Citation2 A random-sample study, completed in Saudi Arabia (n=25.372), shows that chronic low back pain (LBP) is the most common pain complaint at a rate of 46.4%.Citation3
There is a consensus in most international clinical guidelines of LBP management that it should be treated at a primary care setting, with referral to a higher level only being advised when there is a suspected serious pathology (known as a “red flag”).Citation4 The prevalence of LBP patients with serious pathologies in primary care has been reported as low. This means the prevalence of serious pathology will vary depending on where the clinician contacts the person in the clinical pathway. For example, spinal surgeons likely see more cases of serious pathology than general practitioners. Nevertheless, not diagnosing these cases at the primary care level can have life-changing consequences for those patients.Citation5 Conversely, a lack of knowledge about these red flag signs and symptoms could result in referring a large volume of patients to higher centers of care;Citation6,Citation7 therefore, leading to unnecessarily high levels of utilization of medical services, like imaging and consultation, which is associated with a higher impact in terms of the cost of care.Citation8,Citation9
Although these red flags are based on physician’s suspicions,Citation4 a recent framework has identified specific signs and symptoms that often raise the concerns of healthcare professionals (HCP) about serious spinal pathologies.Citation5,Citation19
Incorporating the biopsychosocial framework is a cornerstone in LBP management.Citation4,Citation10,Citation20,Citation26 LBP-associated disabilities are highly correlated with various psychosocial factors;Citation10 therefore, screening for these specific factors is encouraged when treating this condition.Citation11,Citation12 One study highlighted the significant correlation between disability and psychosocial factors in Saudi Arabian LBP patients.Citation14
Notably, the attitudes and beliefs of HCP have been associated with certain features of their chosen clinical management techniques.Citation13,Citation18,Citation19,Citation23–Citation26 Not adopting a biopsychosocial model of care could put more emphasis on structural and pathological explanations for LBP, which then require an objective explanation (radiological) and referrals to higher levels of care.Citation15,Citation19 However, the biopsychosocial model in LBP allows for interaction between a person’s behavior, beliefs, coping techniques, and social environment, and physical dysfunction.Citation21,Citation22 Therefore, several tools have been developed to assess the attitudes and beliefs of HCP.Citation26 Of which the Pain Attitudes and Beliefs Scale (PABS) was commonly used across various disciplines, eg, physiotherapists and general practitioners. Further, it has undergone the most thorough psychometric testing to date.Citation26
In Saudi Arabia, there are limited studies highlighting the current practice in primary care settings of LBP management. Moreover, the utilization of primary care centers is suggested to be inadequate in managing chronic pain conditions;Citation16 as a result, there is a high number of unurgent LBP patients accessing emergency departments.Citation17 This highlights the importance of recognizing current HCP beliefs and attitudes towards low back pain management in Saudi Arabia.
Aim of the Study
This study examined the beliefs and attitudes toward LBP management of primary care physicians (PCP) in the Riyadh region of Saudi Arabia.
Methods
In total, 400 primary HCP in Riyadh were sent an invitation by email to partake in this study. Upon receiving their acceptance to participate in this study, participants clicked a link to an online survey with three sections. The first section collected demographic information (gender, age, work experience etc.). The second section was a vignette of a chronic non-specific LBP case, with questions about advice regarding returning to work, activities, and imaging recommendations included (Appendix 1). In the last section, participants completed the PABS to assess their treatment orientations. The PABS is a 19-item self-administered questionnaire examining the strength of two treatment orientations toward LBP: biomedical (10 items) and behavioral (9 items).Citation23 Each item includes a 6-point Likert scale (“Totally disagree” = 1 to “Totally agree” = 6), with a total possible score ranging from 9 to 54 for the behavioral scale and from 10 to 60 for the biomedical one.Citation23
The Institutional Review Board of the Ministry of Health approved this study (IRB:2019-0060E).
Data Analysis
Data analyses were conducted using the Statistical Package for the Social Sciences (SPSS, Version 25). The level of significance was set at p<0.05 (2-sided). For the descriptive statistics, the absolute and relative frequencies were used for the categorical variables. Continuous data with a normal distribution were presented using the mean and standard deviation, or median and interquartile range when it did not follow the normal distribution. Normality of the data (for continuous variables) was examined using the Shapiro–Wilk test. A Student’s t-test and a one-way ANOVA were then used to compare the continuous data. Chi-square and Likelihood Ratio tests were used to analyze the categorical data. Univariate analysis (Pearson’s or Spearman correlations) and multivariate analysis (logistic regression) were also used to examine the association between the treatment preferences (dependent variable) on the PABS biomedical and behavioral subscales (independent variables).
Results
The final response rate was 18%. Seventy-two primary care physicians participated in this study, with any missing data being deleted pairwise. The demographic data of participants are presented in . Out of all the participants, 46% were female. Only 4% had a special interest in musculoskeletal disorders. None of the participants had received any specialized training in back pain management. However, 1 of the 72 respondents did report receiving some specialized training in managing knee disorders.
Table 1 Participants’ Demographic Data
When asked about the use of clinical guidelines for LBP management, only 35% reported using them. Additionally, 53% reported personal experiences with LBP.
Vignette
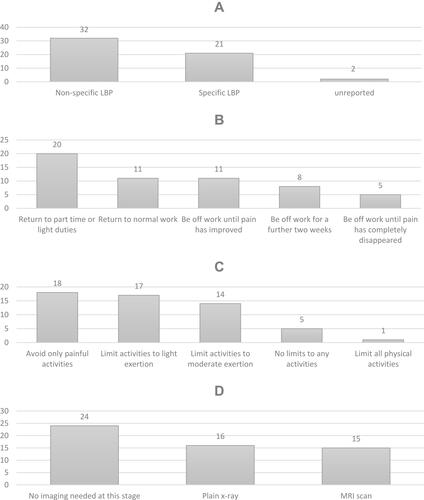
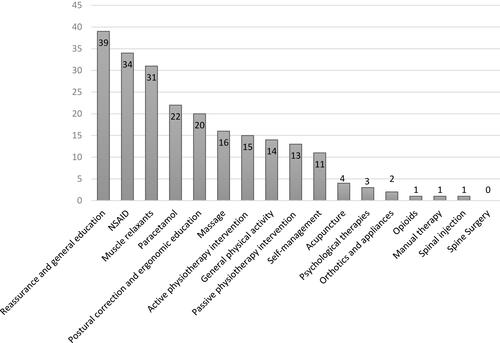
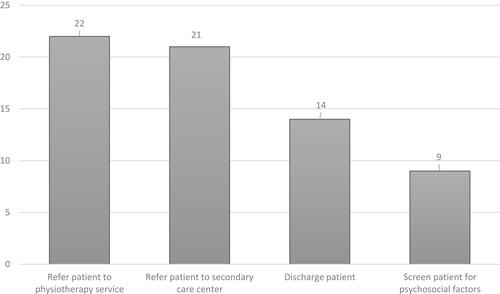
Fifty-five (76%) of the responding primary care physicians completed the questions concerning the case vignette. There was no association found between completing the vignette questions and the demographic data, except for age. Physicians who were older than 41 years were more likely to complete the vignette’s question section (χ2 (5) = 13.8, p = 0.017). The physicians’ responses to the vignette questions, their treatment preferences, and their management suggestions for the case are presented in –.
PABS
Only 38 of the 72 participants (53%) completed the PABS. We compared the demographic data between those who completed the PABS and those who did not. There was no difference found except for a statistically significant association between level of work experience and completion of the PABS (χ2 (5) = 13.9, p = 0.016). Physicians with 11 to 15 years of experience were more likely to withdraw from completing the PABS. The demographic data of the physicians who completed this questionnaire are presented in .
Table 2 Demographic Data of Participants Who Completed the PABS
The normality assumption was met for the PABS behavioral subscale (p = 0.245). However, the biomedical subscale did not meet the normality assumption (p = 0.046). The descriptive data of the PABS subscales are presented in . The correlation (Spearman’s) between the two subscales was found to be significant (rs = 0.51, p < 0.001).
Table 3 Descriptive Data of the PABS Subscale
As there is no consensus on the cut-off score of the PABS (for both scales), and in order to test the association between higher or lower PABS scores for both subscales, we divided the biomedical subscale into two (above and below the median score). Likewise, we divided the behavioral subscale into two (above and below the mean score).
We found a significant association between the use of clinical guidelines and being either above or below the PABS median score for the biomedical subscale (χ2 (1) = 4.7, p = 0.03). Physicians who reportedly used the clinical guidelines for LBP management were more likely to have score below the median on the PABS biomedical subscale.
PABS and the Vignette Responses
Each response to the vignette questions was examined for an association of being either above or below the median score of the PABS biomedical subscale and with being above or below the mean score of the behavioral subscale. There was no significant association found between being above/below the median score of the PABS biomedical subscale and vignette responses (p > 0.05). However, there was a significant association found between being above/below the mean PABS behavioral subscale score and work recommendation (χ2 (4) = 15.5, p = 0.004). Physicians who recommended the patient “to return to part-time or light duties” were more likely to be below the mean score of the behavioral subscale. Conversely, physicians who recommended the patient “to return to normal work” were more likely to be above the PABS behavioral subscale’s mean score.
Similarly, there was a significant association found between being above or below the mean score of the behavioral subscale and activity recommendations (χ2 (4) = 9.6, p = 0.047). Physicians who recommended “no limits to any activities” were more likely to be above the behavioral subscale’s mean score. In contrast, physicians who recommended “limitation on activities to light exertion” were more likely to be below the mean score of the behavioral subscale.
Multiple logistic regression analyses were conducted to predict the participants’ beliefs in each treatment preference—ie, if participants would recommend it or not (dependent variable)— on both the biomedical and behavioral subscales (continuous scores as the independent variables), based on the responses of the 39 respondents. We found a significant association between believing that patients will benefit from reassurance and general education with low scores in the biomedical subscale (Odds-Ratio [OR]: 1.27; 95% Confidence Interval [CI], 1.06–1.52; p = 0.01), as well as a significant association between having a high score in the behavioral subscale with the belief that patients will benefit from reassurance and general education (OR: 0.79; 95% CI, 0.64–0.96; p = 0.02). We also found a significant association between high scores on the behavioral subscale and holding the belief that patients will benefit from a massage (OR: 0.85; 95% CI, 0.73–0.99; p = 0.03).
Discussion
Main Findings
This study aimed to explore the current PCP beliefs and attitudes toward LBP management. To our knowledge, this is the first exploratory survey of LBP related attitudes and beliefs among a group of Saudi Arabian PCPs.
This study’s results indicate that scores on the PABS behavioral subscale are lower than those on the biomedical one. When compared to previous studies, the average biomedical subscale score in this research (mean = 36.5) was lower compared to an Irish sample (mean = 38.8), but was higher when compared to samples from Asia and the United Kingdom (means = 34.8 and 30.9, respectively).Citation23,Citation24,Citation35,Citation27 Further, the average behavioral subscale score was lower (mean = 31.5) among the PCPs in this study compared to those of other researches (means = 35.6 and 33.7) who assessed the same domains with the same questionnaire items.Citation23,Citation24 This result suggests that beliefs and treatment orientations of PCPs practicing in Saudi Arabia are mostly biomedical. Further, this study’s results revealed that only 35% of PCPs practicing in Saudi Arabia reported using the clinical guidelines supporting the conceptualization of LBP as a biopsychosocial health condition.Citation32 This is problematic because LBP is an established biopsychosocial health problem,Citation1,Citation26 with disability related to this pain being shown to be a multifactorial condition among the Saudi Arabian population with chronic LBP.Citation13,Citation28
A robust body of evidence has shown that PCPs’ beliefs about LBP are associated with both their management choices and recommendations, as well as with the beliefs and attitudes of their patients.Citation20 It has been reported that PCPs with a more behavioral orientation are more likely to follow the clinical guideline recommendations and advise their patients “to return to normal work”.Citation12 Conversely, physicians with a mainly biomedical attitude towards LBP were less likely to follow the clinical guidelines for its management and may perceive the continuation of daily activities as more harmful.Citation20,Citation26,Citation35 Consequently, they are more prone to recommend that their patients limit their daily physical activity levels.Citation13 This is consistent with the results of this study which found that its participating physicians who recommended patients “to return to part-time or light work duties” or “limitation on activities to light exertion” were more likely to be below the mean score on the PABS behavioral subscale. These reported beliefs and practice behaviors might reflect fear and are inconsistent with more recent recommendations for LBP treatment that encourage providing clear information about continuing activities, even if there is some pain.Citation36,Citation37 This is a concern given the recognized negative influences of fear of daily activities on LBP-related disabilities and on the overall experience with this condition.Citation1,Citation31,Citation32
Further, the results of our regression analysis, in terms of a significant association between scoring high on the behavioral subscale and holding the belief that patients will benefit from reassurance and general education, is consistent with both clinical guidelines and the broader literature. Specifically, the clinical guidelines recommend both structured education and reassurance for LBP patients to ensure a more favorable prognosis.Citation31 For instance, giving reassuring information to patients is known to improve their coping with the pain, resulting in significant decreases in the overall negative consequences of LBP (eg, increasing their work participation and overall activity continuation).Citation30,Citation33 Compared with the results from similar regression analyses in previous studies, those with lower biomedical subscale scores have been found to follow the clinical guidelines (p < 0.05).Citation25,Citation35 Conversely, a higher biomedical subscale score was associated with increased disagreements with recommendations to return to usual activities or work.Citation39 Further, participants who were male and less experienced were more likely to follow a biomedical approach during the treatment of patients with LBP among physiotherapists.Citation38 Moreover, our findings are in line with a recently published studyCitation40 involving physiotherapists and PCPs from Saudi Arabia, that showed treatment recommendations may not correspond with contemporary clinical guidelines and that will reflect in overutilization of secondary and tertiary healthcare services.Citation41 To sum up, adopting a more behavioral orientation towards LBP may contribute to reductions in the uncertainty of participating in physical activities and will thus establish a more positive continuation of movement and reductions in the fear-avoidance behaviors and overall burdens associated with LBP.Citation30,Citation32,Citation29
Limitations
This study has several limitations. First, the low response rate to the survey (18%) may lead to sampling bias and potentially limit these results’ generalizability. Second, there may have been a selection bias in that HCPs in the Riyadh region were the only participants in this survey; as such, HCPs treatment orientation might be different in other country regions. Although the study sample was from one area in Saudi Arabia, participants were from more than five countries, enhancing the international transferability of the current fining. Third, this study did not investigate the actual prescription of treatment or the subsequent behaviors of patients. Finally, as this was a cross-sectional study, we made statistical comparisons, and some associations may have occurred by chance. Future studies should, therefore, adopt a more longitudinal design and include participants from various Saudi Arabian regions for greater generalizability and to build upon this research’s findings.
Conclusion and Clinical Implications
This study’s results show that many PCPs practicing in Saudi Arabia continue to manage their patients within a biomedical basis. These results also show that there is some compliance to the current LBP clinical practice guidelines. As such, this study’s findings are novel, indicating that PCP’s training and treatment orientations may need improvements, which highlights the pressing need to implement relevant educational programs to ensure that undergraduate Saudi Arabian PCPs are able to adopt a biopsychosocial model of pain to manage conditions like LBP.
Ethical Approval and Consent Statement
The Institutional Review Board of the Ministry of Health approved this study (IRB:2019-0060E) and all participants gave informed consent to participate.
Disclosure
No conflict of interest.
Additional information
Funding
References
- Hoy D, March L, Brooks P, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(6):968–974. doi:10.1136/annrheumdis-2013-204428
- Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8(1):8–20. doi:10.1016/j.spinee.2007.10.005
- Almalki MT, BinBaz SS, Alamri SS, et al. Prevalence of chronic pain and high-impact chronic pain in Saudi Arabia. Saudi Med J. 2019;40(12):1256. doi:10.15537/smj.2019.12.24690
- O’Connell N, Cook C, Wand B, et al. Clinical guidelines for low back pain: a critical review of consensus and inconsistencies across three major guidelines. Best Pract Res Clin Rheumatol. 2016;30(6):968–980. doi:10.1016/j.berh.2017.05.001
- Finucane L, Downie A, Mercer C, et al. International framework for red flags for potential serious spinal pathologies. J Orthop Sports Phys Ther. 2020;50:1–23. doi:10.2519/jospt.2020.9971
- Williams C, Maher C, Hancock M, et al. Low back pain and best practice care: a survey of general practice physicians. Arch Intern Med. 2010;170(3):271–277. doi:10.1001/archinternmed.2009.507
- Schers H, Braspenning J, Drijver R, et al. Low back pain in general practice: reported management and reasons for not adhering to the guidelines in The Netherlands. Br J Gen Pract. 2000;50(457):640–644.
- Cutler R, Fernandez-Llimos F, Frommer M, et al. Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open. 2018;8(1):e016982. doi:10.1136/bmjopen-2017-016982
- Graves J, Fulton-Kehoe D, Jarvik J, et al. Impact of an advanced imaging utilization review program on downstream health care utilization and costs for low back pain. Med Care. 2018;56(6):520–528. doi:10.1097/MLR.0000000000000917
- Foster N, Thomas E, Bishop A, et al. Distinctiveness of psychological obstacles to recovery in low back pain patients in primary care. Pain. 2010;148(3):398–406. doi:10.1016/j.pain.2009.11.002
- National Institute for Health and Care Excellence (NICE). Low back pain and sciatica in over 16s: assessment and management. NICE guideline [NG59]. London, UK: NICE; 2016.
- Qaseem A, Wilt TJ, McLean RM, et al. Clinical Guidelines Committee of the American College of Physicians. Non-invasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Int Med. 2017;166:514–530. doi:10.7326/M16-2367
- Darlow B, Fullen B, Dean S, et al. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: a systematic review. Eur J Pain. 2012;16(1):3–17. doi:10.1016/j.ejpain.2011.06.006
- Alamam D, Moloney N, Leaver A, et al. Pain intensity and fear avoidance explain disability related to chronic low back pain in a Saudi Arabian population. Spine. 2019;44(15):E889–E898. doi:10.1097/BRS.0000000000003002
- Crawford C, Ryan K, Shipton E. Exploring general practitioner identification and management of psychosocial Yellow Flags in acute low back pain. N Z Med J. 2007;120:U2536.
- Alfaqeeh GA. Access and Utilisation of Primary Health Care Services in Riyadh Province, Kingdom of Saudi Arabia [PhD thesis]. University of Bedfordshire; 2015.
- Alyasin A, Douglas C. Reasons for non-urgent presentations to the emergency department in Saudi Arabia. Int Emerg Nurs. 2014;22(4):220–225. doi:10.1016/j.ienj.2014.03.001
- Corbett M, Foster N, Ong BN. GP attitudes and self-reported behaviour in primary care consultations for low back pain. Fam Pract. 2005;26(5):359–364. doi:10.1093/fampra/cmp042
- Schers H, Wensing M, Huijsmans Z, et al. Implementation barriers for general practice guidelines on low back pain: a qualitative study. Spine. 2001;26(15):E348–E353. doi:10.1097/00007632-200108010-00013
- Darlow B. Beliefs about back pain: the confluence of client, clinician and community. Int J Osteopath Med. 2016;20:53–61. doi:10.1016/j.ijosm.2016.01.005
- Pincus T, Kent P, Bronfort G, et al. Twenty-five years with the biopsychosocial model of low back pain—is it time to celebrate? A report from the twelfth international forum for primary care research on low back pain. Spine. 2013;38(24):2118–2123. doi:10.1097/BRS.0b013e3182a8c5d6
- Houben RM, Ostelo RW, Vlaeyen JW, et al. Health care providers’ orientations towards common low back pain predict perceived harmfulness of physical activities and recommendations regarding return to normal activity. Eur J Pain. 2005;9(2):173–183. doi:10.1016/j.ejpain.2004.05.002
- Poitras S, Durand MJ, Côté AM, et al. Guidelines on low back pain disability: interprofessional comparison of use between general practitioners, occupational therapists, and physiotherapists. Spine. 2012;37(14):1252–1259. doi:10.1097/BRS.0b013e31824b6adf
- Bishop A. Pain attitudes and beliefs scale (PABS). J Physiother. 2010;56(4):279. doi:10.1016/S1836-9553(10)70014-X
- Sit RW, Yip BH, Chan DC, et al. Primary care physicians’ attitudes and beliefs towards chronic low back pain: an Asian study. PLoS One. 2015;10(1):e0117521. doi:10.1371/journal.pone.0117521
- Bishop A, Thomas E, Foster NE. Health care practitioners’ attitudes and beliefs about low back pain: a systematic search and critical review of available measurement tools. Pain. 2007;132(1):91–101. doi:10.1016/j.pain.2007.01.028
- Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356–2367. doi:10.1016/S0140-6736(18)30480-X
- Alamam DM, Moloney N, Leaver A, et al. Multidimensional prognostic factors for chronic low back pain-related disability: a longitudinal study in a Saudi population. Spine J. 2019;19(9):1548–1558. doi:10.1016/j.spinee.2019.05.010
- Vlaeyen JW, Kole-Snijders AM, Rotteveel AM, et al. The role of fear of movement/(re)injury in pain disability. J Occup Rehabil. 1995;5(4):235–252. doi:10.1007/BF02109988
- Frederiksen P, Indahl A, Andersen LL, et al. Can group-based reassuring information alter low back pain behavior? A cluster-randomized controlled trial. PLoS One. 2017;12(3):e0172003. doi:10.1371/journal.pone.0172003
- Oliveira CB, Maher CG, Pinto RZ, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J. 2018;27(11):2791–2803. doi:10.1007/s00586-018-5673-2
- Burton AK, Waddell G, Tillotson KM, et al. Information and advice to patients with back pain can have a positive effect. A randomized controlled trial of a novel educational booklet in primary care. Spine (Phila Pa 1976). 1999;24(23):2484–2491. doi:10.1097/00007632-199912010-00010
- Traeger AC, Huebscher M, Henschke N, et al. Effect of primary care–based education on reassurance in patients with acute low back pain: systematic review and meta-analysis. JAMA Intern Med. 2015;175(5):733–743. doi:10.1001/jamainternmed.2015.0217
- Fullen BM, Baxter GD, Doody C, et al. General practitioners’ attitudes and beliefs regarding the management of chronic low back pain in Ireland: a cross-sectional national survey. Clin J Pain. 2011;27(6):542–549. doi:10.1097/AJP.0b013e31821771e2
- Linton SJ, Vlaeyen J, Ostelo R. The back pain beliefs of health care providers: are we fear-avoidant? J Occup Rehabil. 2002;12(4):223–232. doi:10.1023/A:1020218422974
- Coudeyre E, Rannou F, Tubach F, et al. General practitioners’ fear-avoidance beliefs influence their management of patients with low back pain. Pain. 2006;124(3):330–337. doi:10.1016/j.pain.2006.05.003
- Magalhães MO, Costa LO, Cabral C, et al. Attitudes and beliefs of Brazilian physical therapists about chronic low back pain: a cross-sectional study. Braz J Phys Ther. 2012;16(3):248–253. doi:10.1590/S1413-35552012005000014
- Derghazarian T, Simmonds MJ. Management of low back pain by physical therapists in Quebec: how are we doing? Physiother Can. 2011;63(4):464–473. doi:10.3138/ptc.2010-04P
- Cherkin DC, Deyo RA, Wheeler K, et al. Physician views about treating low back pain. The results of a national survey. Spine. 1995;20:1–9. doi:10.1097/00007632-199501000-00001
- Alhowimel A, Alodaibi F, Alotaibi M, Alamam D, Fritz J. Comparison of attitudes and beliefs of physical therapists and primary care physicians regarding low back pain management: a cross-sectional study. J Back Musculoskelet Rehabil. 2021;1–7. doi:10.3233/bmr-200295
- Alhowimel AS, Alodaibi FA, Alotaibi MA, Alamam DM, Fritz J. Management of Low back pain in Saudi Arabia healthcare system. A Qualitative Study. Inquiry. 2021;58:469580211060178. doi:10.1177/00469580211060178