Abstract
Objectives
Little is known about the factors that influence survival following in-hospital resuscitation, but previous investigations have suggested that in-hospital resuscitations outside of regular working hours are associated with worse survival rates.
Material and methods
In-hospital cardiac arrest teams at our hospital were instructed to complete a questionnaire following every emergency call between July 2011 and June 2013. Data on all resuscitation attempts were collected and analyzed.
Results
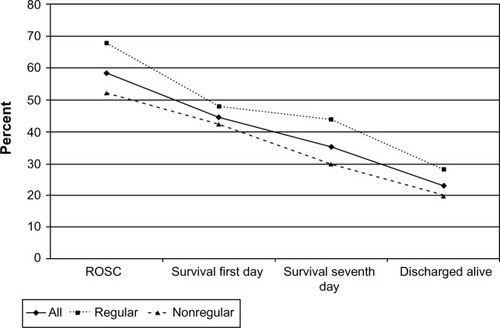
A total of 65 in-hospital resuscitations were recorded in 42 males (64.6%) and 23 females (35.4%) (mean age 72.0±14.3 years). A total of 54 (83.1%) cardiac arrests were witnessed; seven (10.8%) showed a shockable rhythm at the time of the first ECG. Resuscitation attempts lasted 29.3±41.3 minutes, and 4.1±3.1 mg epinephrine was given. Return of spontaneous circulation could be achieved in 38 patients (58.5%); 29 (44.6%) survived the first day, 23 (35.4%) the seventh day, and 15 patients (23.1%) were discharged alive. Significantly more in-hospital resuscitations were obtained for those performed during non-regular working hours (P<0.001), with higher neuron-specific enolase levels at 72 hours after resuscitation during nonregular working hours (P=0.04). Patients who were discharged alive were significantly younger (P=0.01), presented more often with an initial shockable rhythm (P=0.04), and had a shorter duration of resuscitation (P<0.001) with the need of a lower dose of epinephrine (P<0.001).
Discussion
Survival rates following in-hospital resuscitation were poor at any time, but appear to depend less on time-dependent effects of the quality of resuscitation and more on time-dependent effects of recognition of cardiac arrests.
Objectives
Previous studies have estimated that a large number of in-hospital cardiac arrests occur; for example, more than 200,000 in-hospital cardiac arrests occur annually in the United States.Citation1 Despite this substantial number of patients, only a few studies have focused on this theme. Factors that have been described as being relevant for surviving an in-hospital cardiac arrest include an initial shockable rhythm, younger age, shorter duration of arrest, and time of arrest.Citation2 Time-dependent effects were also reported in another large investigation that described lower survival rates of in-hospital cardiac arrest during nights and weekends.Citation3
Since the implementation of in-hospital cardiac arrest teams during the past few years, we are of the opinion that the time of an arrest can no longer automatically be associated with differences in the quality of resuscitation and the outcome following an in-hospital cardiac arrest. For this reason, we initiated this study to test our hypothesis that, due to specialized emergency teams being available 24 hours a day, there are no time-dependent differences in survival of in-hospital cardiac arrest in a good neurological state.
Material and methods
In-hospital cardiac arrest team
In clinically unstable inpatients, early intervention by a medical emergency team significantly reduces the incidence of and mortality from unexpected in-hospital cardiac arrest.Citation4 Consequently, in our hospital, a central in-hospital cardiac arrest team was implemented a few years ago. This team comprises one emergency physician and an experienced intensive care nurse who are available 24 hours a day by emergency call and can reach every in-hospital emergency within 4 minutes.
Data collection
In our hospital, all in-hospital emergency calls initially reach the coordination center, who then alert the emergency physician and the intensive care nurse. All emergency calls, therefore, can be registered in a central database, and our in-hospital cardiac arrest teams could be instructed to fill out a questionnaire following every emergency call due to a cardiac arrest between July 2011 and June 2013. The questionnaires contained data regarding sex, age, place of emergency, initial rhythm, and duration of resuscitation, as well as the number of defibrillations and applied medication.
Regular working hours were defined as the time between 8 am and 5 pm Monday through Friday, except for holidays. This threshold was chosen in accordance with the regular working hours of the physicians in our hospital.
The cardiac arrest was classified as “in-hospital” if it occurred in a hospitalized patient who had a pulse at the time of admission. Resuscitation attempts following in-hospital cardiac arrests were recorded and stored on a central database. Data were completed by additional review of the patient records. The primary endpoint of our study was survival following in-hospital cardiac arrest. The secondary endpoint was survival in a good neurological state (cerebral performance category [CPC] 1 or 2). Statistical analyses were performed using Student’s t-tests and Pearson’s chi-squared tests with the Statistical Package for the Social Sciences (SPSS 22.0; IBM, Armonk, NY, USA).
The study adhered to all criteria of the WMA Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects.
Results
Patient data
A total of 65 in-hospital resuscitations were recorded between July 1, 2011, and June 30, 2013, in 42 males (64.6%) and 23 females (35.4%) with a mean age of 72.0±14.3 years. A total of 54 (83.1%) in-hospital resuscitations followed witnessed arrests (either directly or indirectly via ECG monitoring); seven patients (10.8%) presented with an initial shockable rhythm.
Resuscitation attempts lasted 29.3±41.3 minutes, and 4.1±3.1 mg epinephrine was given. Initial return of spontaneous circulation (ROSC) could be achieved in 38 patients (58.5%); 29 (44.6%) survived the first day, 23 (35.4%) the seventh day, and 15 patients (23.1%) were discharged alive. Among those discharged, eleven patients (16.9%) showed a good cerebral performance category (CPC 1), two patients (3.1%) had moderate disabilities (CPC 2), and two patients (3.1%) remained in a vegetative state (CPC 4).Citation5
The cause of death was cardiac-related in 36 patients (55.4%), hypoxemia in 16 patients (24.6%), and other reasons in 13 patients (20.0%). Neuron-specific enolase (NSE) level was 57.5±108.8 ng/mL at 24 hours after resuscitation, and 35.7±19.3 ng/mL at 72 hours after resuscitation.
The first electrocardiogram (ECG) after resuscitation showed heart rates of 90.2±27.6 beats per minute (bpm) and a frequency-related QT time of 462.1±42.5 ms; maximal creatinine kinase was 2197.9±1960.0 U/L.
After ROSC, the following were observed: first pH =7.25±0.15, pCO2 =48.2±26.6 mmHg, pO2 =130.3±104.8 mmHg, lactate =5.6±4.8 mmol/L, and potassium =4.2±0.8 mmol/L ().
Table 1 Patient characteristics
Resuscitation during regular and nonregular working hours
According to the classification of regular and nonregular working hours as described in the Data collection section, significantly more in-hospital resuscitations were observed during nonregular working hours (P<0.001). No differences were observed between patients resuscitated during regular working hours and those resuscitated during nonregular working hours, except for a significantly higher NSE level at 72 hours after resuscitation during nonregular working hours (P=0.04; ).
Post hoc analyses depending on patient follow-up
A comparison of patients who were discharged alive following in-hospital resuscitation and those who died during follow-up showed several significant differences (). Patients who were discharged alive were significantly younger (P=0.01), presented more often with an initial shockable rhythm (P=0.04), and had a shorter duration of resuscitation (P<0.001) with the need for a lower dose of epinephrine (P<0.001).
Table 2 Post hoc analyses depending on patient’s survival during follow-up
Patient characteristics, including first blood gas analysis and ECG criteria following ROSC, showed no significant differences.
Discussion
Duration of cardiopulmonary resuscitation, age, initial rhythm, and witnessed events are factors that have been described to influence survival of any kind of sudden cardiac arrest; ie, in-hospital cardiac arrestCitation6 as well as out-of-hospital cardiac arrest.Citation7 However, as patients of in-hospital cardiac arrest are hospitalized due to preexisting illness, they cannot be directly compared with patients of out-of-hospital cardiac arrests; for example, acute apoplectic stroke, preexisting severe sepsis, and preexisting poor CPC scores have been associated with a very poor prognosis for surviving in-hospital cardiac arrest in a good neurological state.Citation8
For this reason, further studies were demanded to specifically focus on in-hospital cardiac arrests, and we initiated our study to investigate whether the time of arrest still influences survival from in-hospital cardiac arrest despite the implementation of in-hospital cardiac arrest teams.
Unfortunately, despite the implementation of in-hospital cardiac arrest teams, survival rates following in-hospital resuscitation are poor even with acceptable rates of initial ROSC.Citation2,Citation9–Citation11 In our study, only 23.1% of all resuscitated patients were discharged alive, and only 20.0% of all resuscitated patients left the hospital in a good neurological state (CPC 1 or 2).
Effect of time on survival rates following in-hospital cardiac arrest
It has been assumed that the time of an arrest may influence survival rates following in-hospital cardiac arrest, with poorer results obtained for resuscitation performed during nonregular working hours.Citation2,Citation3,Citation10 Nevertheless, previous studies did not consider that 24/7 in-hospital resuscitation teams might cause comparable conditions for victims of in-hospital cardiac arrests independent from the time of an arrest.
In our study, time-dependent effects were minimal; the only observed difference was a higher NSE level at 72 hours after in-hospital resuscitation during nonregular working hours, which affected neither the survival rates nor the neurological outcomes among survivors ( and ). We therefore doubt that the time of resuscitation has a relevant effect on the efficiency of the resuscitation procedure itself; at least in hospitals with 24/7 in-hospital cardiac arrest teams. Following this idea, we think that lower survival rates from in-hospital cardiac arrest during nights and weekends may be more a problem of a later detection of the cardiac arrest. This theory is supported by the following two findings. First, the nurse-to-bed ratio has been described as a relevant modifiable factor for survival following an in-hospital cardiac arrest.Citation12 Second, the median hospital cardiac arrest incidence rate has been described as 4.02 per 1,000 admissions,Citation12 but during our study period, approximately 35,000 admissions were observed in our hospital, which would imply that approximately 140 expected in-hospital cardiac arrests were observed during the same time. Nevertheless, only 65 resuscitation attempts were identified in our study, suggesting a significant percentage of in-hospital cardiac arrests that occurred without resuscitation attempts. Furthermore, 83.1%, of cardiac arrests were witnessed in our study, which indicates that resuscitation attempts were mainly initiated following a witnessed event. Considering these findings, we think those previously described effects of time of arrest on survival rates might be more a problem of delayed recognition rather than poor resuscitation.
Limitations
The main limitation of this study is the small number of patients. We therefore think that further studies should be performed to verify our results.
Conclusion
Survival rates following in-hospital resuscitation might depend less on time-dependent effects of the quality of resuscitation and more on on time-dependent effects of recognition. Nevertheless, our single-center results should be confirmed by further investigations and larger trials.
Disclosure
The authors report no conflicts of interest in this work.
References
- MerchantRMYangLBeckerLBAmerican Heart Association Get with the Guidelines-Resuscitation InvestigatorsIncidence of treated cardiac arrest in hospitalized patients in the United StatesCrit Care Med201139112401240621705896
- CooperSJanghorbaniMCooperGA decade of in-hospital resuscitation: outcomes and prediction of survival?Resuscitation200668223123716325314
- PeberdyMAOrnatoJPLarkinGLNational Registry of Cardiopulmonary Resuscitation InvestigatorsSurvival from in-hospital cardiac arrest during nights and weekendsJAMA2008299778579218285590
- BuistMDMooreGEBernardSAWaxmanBPAndersonJNNguyenTVEffects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary studyBMJ2002324733438739011850367
- AjamKGoldLSBeckSSDamonSPhelpsRReaTDReliability of the Cerebral Performance Category to classify neurological status among survivors of ventricular fibrillation arrest: a cohort studyScand J Trauma Resusc Emerg Med2011193821672267
- KantamineniPEmaniVSainiARaiHDuggalACardiopulmonary Resuscitation in the Hospitalized Patient: Impact of System-Based Variables on Outcomes in Cardiac ArrestAm J Med Sci Epub2014423
- McNallyBRobbRMehtaMCenters for Disease Control and PreventionOut-of-hospital cardiac arrest surveillance – Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005–December 31, 2010MMWR Surveill Summ201160811921796098
- EbellMHAfonsoAMGeocadinRGAmerican Heart Association’s Get With the Guidelines-Resuscitation (formerly National Registry of Cardiopulmonary Resuscitation) InvestigatorsPrediction of survival to discharge following cardiopulmonary resuscitation using classification and regression treesCrit Care Med201341122688269724107638
- BloomHLShukrullahICuellarJRLloydMSDudleySCZafariAMLong-term survival after successful inhospital cardiac arrest resuscitationAm Heart J2007153583183617452161
- RužmanTTotOKIvićDGulamDRužmanNBurazinJIn-hospital cardiac arrest: can we change something?Wien Klin Wochenschr201312517–1851652323928936
- KaernestedBIndridasonOSBaldurssonJArnarDOIn-hospital cardiopulmonary resuscitation at Landspitali University Hospital in ReykjavikLaeknabladid2009957–8509514 Icelandic19553709
- ChenLMNallamothuBKSpertusJALiYChanPSAmerican Heart Association’s Get With the Guidelines-Resuscitation (formerly the National Registry of Cardiopulmonary Resuscitation) InvestigatorsAssociation between a hospital’s rate of cardiac arrest incidence and cardiac arrest survivalJAMA Intern Med2013173131186119523689900