 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
Anticaries agents must interfere with the adhesion of Streptococcus mutans and its proliferation in dental biofilm, without causing host toxicity and bacterial resistance. Natural substances, including cationic antimicrobial peptides (CAMPs) and their fragments, such as β-defensin-3 peptide fragment (D1–23), have been widely studied. However, the chemical and physical stability of CAMPs may be compromised by external factors, such as temperature and pH, reducing the period of antimicrobial activity.
Methods
To overcome the aforementioned disadvantage, this study developed and character-ized a drug delivery system and evaluated the cytotoxicity and effect against S. mutans biofilm of a D1–23-loaded bioadhesive liquid crystalline system (LCS). LCS was composed of oleic acid, polyoxypropylene-(5)-polyoxyethylene-(20)-cetyl alcohol, Carbopol® 974P and Carbopol® 971P. LCS was analyzed by polarized light microscopy (PLM), rheology (viscoelasticity and flow properties) and in vitro bioadhesion. The viability of epithelial cells was evaluated. Minimal inhibitory concentration (MIC) and minimal bactericidal concentration (MBC) against S. mutans were determined for D1–23 for further evaluation of the effect against S. mutans biofilm after 4 and 24 h of exposure to treatments.
Results
PLM, rheology, and in vitro bioadhesion tests showed that both viscosity and bioadhesion of LCS increased after it was diluted with artificial saliva. D1–23-loaded LCS system presented better activity against S. mutans biofilm after 24 h when compared to 4 h of treatment, showing a cumulative effect. Neither LCS nor D1–23-loaded LCS presented toxicity on human epithelial cells.
Conclusion
D1–23-loaded LCS is a promising drug delivery system for the prevention of dental caries.
Introduction
Dental caries is the most common oral disease worldwide. The three main factors related to caries development had already been identified almost 100 years ago: diet, microbiota and susceptible tooth, influenced by sociocultural aspects and local risk factors such as salivary flow, teeth anatomy and oral hygiene.Citation1 Nowadays, the caries ecology theory has hypothesized how the caries process occurs based on the succession of microorganisms in the dental biofilm determined by the frequency of sugar intake. Under severe and prolonged acidic conditions promoted by sugar metabolism, mutans streptococci and lactobacilli become dominant (aciduric stage) reducing drastically pH and leading to net mineral loss.Citation2 Streptococcus mutans has been considered as the primary etiological agent of dental caries, due to its ability to metabolize a wide variety of carbohydrates and produce large amounts of acid, while also tolerating extreme concentrations of sugars and acids.Citation3 Although dental biofilm is composed of multiple bacterial species, antimicrobial agents, which could interfere with the adhesion of S. mutans and its proliferation in dental biofilm, would be useful for controlling dental caries.Citation4
Natural substances with antimicrobial properties have been studied as topical agents for oral cavity to reduce pathogens without causing bacterial resistance.Citation4 Cationic antimicrobial peptides (CAMPs), such as β-defensins, have been introduced as future antimicrobial agents due to their rapid onset killing and broad-spectrum activity against Gram-positive and Gram-negative bacteria, fungi and viruses, allied with potentially low levels of induced resistance.Citation5
Human b-defensins (hBDs) are produced by epithelial cells in various organs, such as the eyes, skin, lungs, kidneys, pancreas and nasal and oral mucosa. In addition to their antimicrobial activity, β-defensins have an immunomodulatory function by modifying cell migration and maturation, inducing cytokines such as monocyte chemotactic protein-1, macrophage inflammatory protein-3α (MIP-3α) and interferon-γ inducible protein-10 (IP-10), enhancing chemotactic capacity and releasing histamine and prostaglandin A2.Citation6–Citation8 hBD-3 has shown action against the important primary and secondary colonizers of caries-related biofilm, such as S. mutans and Lactobacillus casei, with minimal inhibitory doses ranging from 1.25 to 200 µg/mL.Citation9 However, the large amino acid sequence (45 residues) and the presence of cysteine linkages on the structure make the synthesis of hBD-3 very expensive. In addition, native peptides tend to be easily degraded by external factors, such as temperature and pH, with a reduced activity in the presence of salt, serum and proteinases.Citation10 Therefore, modifications on the sequence or structure of natural peptides could generate a new synthetic CAMP that would have the same or superior broad-spectrum action against bacterial pathogens, low toxicity to the host and a minimal molecular size for low-cost production.Citation11
Recently, fragments or analogs of CAMP have been synthesized, and their immunological and microbiological functions have been studied. Reynolds et alCitation12 evaluated the bactericidal activity of peptide fragments of a β-defensin-3 derivative and found that the 23-amino acid N-terminal half (D1–23) of Defb14-1Cv (mouse ortholog of human β-defensin-3) is a potent antimicrobial, while the C-terminal half is not. To maintain chemical and physical stability and provide controlled release, drug delivery systems could be an attractive strategy for the administration of peptides.Citation13
Several studies have evaluated the incorporation of peptides in drug delivery systems in the treatment of cardiovascular diseases,Citation14 AIDSCitation15 and diabetes.Citation16 Liquid crystalline systems (LCSs) are a drug delivery system that can be used for incorporating peptides.Citation17,Citation18 LCS can promote controlled release of drugs and protect active ingredients from thermal degradation and photodegradation, while improving the effectiveness of these peptides.Citation19 The bioadhesive property of these systems can maintain a high concentration of the peptide at the site of action for a long period, while also protecting it from environmental degradation. Therefore, the objective of this study was to characterize a liquid crystalline precursor bioadhesive system and evaluate the cytotoxicity and effect against S. mutans biofilm when incorporating D1–23 (β-defensin-3 peptide fragment) in LCS.
Materials and methods
Preparation of the liquid crystal precursor bioadhesive system
First, 2.5% (w/w) Carbopol® 974P (C974) and 2.5% (w/w) Carbopol® 971P (C971; Lubrizol, Wickliffe, OH, USA) were dispersed in water and homogenized at 2,000 rpm in a mechanical stirrer until complete dissolution, at room temperature (25°C±0.5°C). The pH of the binary polymeric dispersion was adjusted to 6.0 with triethanolamine (Synth; Diadema, Sao Paulo, Brazil) and manual agitation.Citation20
Then, LCS (or F from formulation) was prepared weighing and mixing 40% (w/w) polyoxypropylene-(5)-polyoxyethylene-(20)-cetyl alcohol as the surfactant, 50% (w/w) oleic acid as the oil phase and 10% (w/w) binary polymeric dispersion containing 2.5% C974 and 2.5% C971 as the aqueous phase at room temperature (25°C±0.5°C). Thus, the final polymeric concentration in the F was 0.25% (w/w) for each polymer.
To evaluate the in situ lyotropic behavior, F was diluted with artificial saliva in a 1:10 (w/w) ratio to generate F10, a 1:30 (w/w) ratio to generate F30, a 1:50 ratio to generate F50 and a 1:100 ratio to generate F100. A volume of 1 L of artificial saliva was prepared by mixing 8.0 g of NaCl, 0.19 g of KH2PO4 and 2.38 g of Na2HPO4. After complete mixing, the pH was measured as 6.8.Citation20
Polarized light microscopy (PLM)
A 10 µL drop of F, F10, F30, F50 and F100 was applied on a glass slide and covered with a coverslip. Polarized light microscope (Jenamed; Carl Zeiss Meditec AG, Jena, Germany) at a magnification of 20× and at room temperature was used to analyze the glass slides to assess the presence of anisotropy or isotropy of the dispersion.Citation21
Rheological analysis
A controlled-stress AR2000 rheometer (TA Instruments, New Castle, DE, USA) was used to analyze the rheological behavior of formulations in triplicate at 37°C±0.1°C. A parallel-plate geometry (40 mm diameter) and a sample gap of 200 µm were used for F100, and a cone-plate geometry (40 mm diameter) and a sample gap of 52 µm were used for F. The formulations (500 mg) were applied to the lower plate and maintained for 3 min prior to analysis.Citation22 The same bath of formulations was used for each test.
Determination of flow properties
The determination of flow properties of formulations was performed using a controlled shear rate procedure ranging from 0.01 to 100 s−1 and back. Each stage lasted 120 s with an interval of 10 s between the curves. The quantitative analysis of flow behavior was determined using the following formula:
Oscillatory analyses
Viscoelastic region of the formulations was determined by means of a stress sweep in a constant frequency of 1 Hz over a stress range of 0.1–10 Pa. A constant shear stress of 1 Pa was selected to perform the frequency sweep over a range of 0.1–10 Hz. Thus, the storage (G′) and loss (G″) modules were recorded using the following equation:
In vitro bioadhesion strength
This study protocol was performed according to the International Guideline Principles for Biomedical Research involving animals (Council for International Organization of Medical Sciences [CIOMS]/International Council for Laboratory Animal Science, 2012) and approved by The Animal Research Ethics Committee of the Araçatuba School of Dentistry, São Paulo State University (UNESP; protocol 2014/00618). Enamel blocks from sound bovine permanent incisors were cut transversally from the middle third of the buccal surface using a water-cooled, double-faced diamond disk (KG Sorensen, Barueri, Brazil). The specimens were then rounded using a high-speed, water-cooled cylindrical diamond bur (1095; KG Sorensen) and polished with wet 200-grit silicon carbide paper (T469-SF-Norton; Saint-Gobain Abrasivos Ltda., Jundiaí, Brazil) to normalize the surface until it reaches the diameter of 1 cm.Citation18
The bioadhesive force between the bovine tooth block moistened with saliva, and the formulations were assessed using a TA-XTplus texture analyzer (Stable Micro Systems, Godalming, UK) in adhesion test mode (hold until time [HUT] mode). About 500 mg of each formulation was packed in a small glass container with the flat surface. The teeth model was fastened to the upper movable probe, and the formulation sample was located on the lower platform. Before the test, the tooth was immersed in artificial saliva. The probe was lowered until it made contact with the sample, and it was kept in contact without any force for 60 s. The probe was then raised at 0.5 mm/s, and the force needed for detachment was registered. Seven replicates of the same batch of formulations were analyzed at 37°C±0.5°C.Citation18,Citation22 The same enamel block was also used for all the tests to minimize the differences on the tooth surface’s roughness. There were not enough remaining formulations on the tooth surface to be quantified.
Antimicrobial agents
Preparation of peptide and chlorhexidine diacetate (CHX)
D1–23-Defb14-1Cv (D1–23) (sequence of amino acids from the peptide D1–23: FLPKTLRKFFARIRGGRAAVLNA)Citation12 (molecular weight [MW]: 2603.88) was synthesized at the Institute of Chemistry (UNESP, Araraquara, Brazil). Solid-phase peptide synthesis was performed manually using Fmoc (9-fluorenylmethyloxycarbonyl) protocols on the Fmoc-Ala-Wang resin.Citation23,Citation24 The molecular masses of the peptides were determined using mass spectrometry, with a positive ion mode electrospray ionization apparatus (Bruker Optik GmbH, Ettlingen, Germany) in agreement with the corresponding calculated values.Citation12 Purification of synthesized peptides was performed in a semi-preparative high performance liquid chromatography Beckman System Gold on a reverse phase C18 column (2.1 × 25 cm). Final purity levels of peptides were determined at least 95% on a Shimadzu chromatography equipped with an analytical C18 reverse-phase column (0.46 × 25 cm).Citation25 The positive control group was CHX, purchased from Sigma-Aldrich Co. (St Louis, MO, USA). A stock solution of 2% CHX was used for microbiological and cytotoxicity assays.
Incorporation of antimicrobial agents into LCS
Peptide fragment D1–23 and CHX were incorporated into the aqueous phase of formulation (F) at the concentration of 1 mg/mL based on a previous study showing that about 4% of peptide is released from LCS.Citation26 CHX is frequently used as an antimicrobial agent for oral application at 0.12% or ~1 mg/mL. Then, the groups of the study were D1–23 and CHX solutions, LCS (F), LCS containing D1–23 (F+D1–23) and LCS containing CHX (F+CHX). LCS was diluted 10-fold before incorporating CHX and D1–23 to reduce the viscosity for biofilm assays.Citation27
Microbiological evaluation
Determination of minimal inhibitory concentration (MIC) and minimal bactericidal concentration (MBC)
MIC and MBC of D1–23 and CHX solutions were determined using the microdilution broth method, in 96-well microtiter plates, following the criteria previously described by Clinical and Laboratory Standard Institute (CLSI).Citation28 Cell suspensions of S. mutans (UA159 – from University of Alabama, or ATCC 700610) at the mid-log phase (OD550=0.5) were harvested by centrifugation (Hanil Combi centrifuge, 514R) for 10 min, at 3,000×g; the supernatant was discarded, and the pellet was resuspended in 2× concentrated Mueller–Hinton broth (Difco Laboratories, Detroit, MI, USA) and diluted 1,000× in Mueller–Hinton broth. The final concentration of the suspension of S. mutans in the wells was 5–10×105 colony forming units/mL. Initially, the antimicrobial solution (peptide and CHX) was serially diluted in sterile distilled water to obtain the concentrations ranging from 0.003 to 2 mg/mL and after 50 µL microbial suspensions (correctly adjusted for the concentrations described earlier) were inoculated in each well. The plates were incubated at 37°C for 24 h in a 5% CO2 atmosphere. Afterward, 15 µL of 0.01% resazurin (Sigma-Aldrich Co.) was applied in each well and incubated for 4 h to promote an oxidation–reduction reaction and to determine cell viability by visually detecting any color change. The wells corresponding to MIC (the last blue well) and at least three previous wells were then homogenized, serially diluted and plated on Mueller–Hinton agar to determine the MBC. The plates were incubated at 37°C for 24 h in a 5% CO2 atmosphere. The colonies were counted, and the number of viable bacteria was determined in colony forming units/mL. The MBC was considered when the peptide fragments killed (99%) the tested microbial culture. CHX was used as a positive control. The negative control was the bacterial cultures without antimicrobial agents in Mueller–Hinton broth. All experiments were performed in duplicate in three independent days (n=6).
Biomass biofilm assays
Briefly, 200 µL of 5–10×105 cells of S. mutans (UA 159) in Brain Heart Infusion (Difco Laboratories) added 1% sucrose was distributed per well in 96-well microtiter plates in triplicate and incubated at 37°C for 48 h. After incubation, the wells were washed by immersion in 0.9% saline. Then, 150 µL of each treatment (at 1 mg/mL): D1–23 and CHX solutions, LCS (F), LCS containing D1–23 (F+D1–23) and LCS containing CHX (F+CHX), was added and incubated for 4 and 24 h at 37°C and 5% CO2. Negative controls were LCS without antimicrobial agents (F) and 0.9% NaCl solution. After incubation, the plates were washed by immersion in distilled water three times to remove non-adhered cells. After a brief drying, 150 µL of aqueous 1% crystalline violet was added to each well, and the plates were incubated at room temperature for 30 min. Next, the crystalline violet solution was removed, and the plates were washed again three times. The plates were inverted on paper towels and remained for 2 h at room temperature to dry. The crystalline violet dye (stained biofilm) was then solubilized by incubation with 200 µL of ethanol per well for 30 min. Then, 100 µL of the dye in ethanol was transferred to wells of a new microplate and submitted to reading in a spectrophotometer at 500 nm (Eon Microplates, Biotek Instruments, Winooski, VT, USA) to quantify the biomass of the biofilm.Citation29 For the anti-biofilm assay, the mean absorbance values obtained from the control group (bacterial growth without antimicrobial agents) were calculated and considered as 100% of cell viability, and the percentage values of biofilm biomass reduction for the tested groups were calculated based on these criteria.
Cytotoxicity assays
These assays were conducted based on the methodology described by Bedran et alCitation30 in duplicate, in three independent experiments (n=6). Human epithelial cells forming the HaCat cell line (spontaneous immortalized non-tumorigenic human keratinocyte cell line – code 341; Banco de Células do Rio de Janeiro, Rio de Janeiro, Brazil) were grown in Dulbecco’s Modified Eagle’s Medium (DMEM; Thermo Fisher Scientific, Waltham, MA, USA) plus 10% fetal calf serum and 100 µg/mL of penicillin G/streptomycin until reaching a subconfluent density at 37°C in 5% CO2 atmosphere. After that, the cells were treated with trypsin for 5 min (TrypLE™ Express; Thermo Fisher Scientific) at 37°C, followed by the inactivation of proteases by adding 0.3 mg/mL of trypsin inhibitor. Cells were centrifuged (500×g for 5 min), resuspended in DMEM and incubated in a 96-well microplate (200 µL/well, 1×106 cells/mL) overnight at 37°C in a 5% CO2 atmosphere. After that, they were then stimulated with D1–23 and CHX solutions at concentrations of 0.001–1 mg/mL and 10 µL of LCS containing or not containing D1–23 and CHX at 1 mg/mL (F, F+D1–23, F+CHX) for 24 h at 37°C in a 5% CO2 atmosphere. Cell viability was determined by using a colorimetric 3-(4,5-diethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide (MTT) cell viability assay (Sigma-Aldrich Co.) as the substrate at 5 mg/mL. After 4 h of incubation, the culture medium with the MTT solution was replaced with 100 µL of acidified isopropanol solution (0.04 NHCl), an aliquot of each well was transferred to 96-well plates (Costar Corp., Cambridge, MA, USA) and the cell viability was measured using spectrophotometer (model 3550-UV; Bio-Rad Laboratories Inc., Hercules, CA, USA) at 570 nm wavelength. The mean was calculated and transformed into percentages, considering that negative control (DMEM) was defined as having 100% cell metabolism.
Statistical analyses
The characterization of the LCS was presented using descriptive analysis. Mean and SD for the bioadhesion strength values were determined for each group, and differences were analyzed using analysis of variance (ANOVA) and post hoc Tukey tests. Kruskal–Wallis and Mann–Whitney tests were applied to compare the percentage of biofilm biomass reduction for the groups, at different times. Data from cytotoxicity were submitted to ANOVA and post hoc Tukey or Student’s t-tests to compare the effect of treatments on epithelial cells, considering each concentration separately. All tests were applied considering p<0.05.
Results
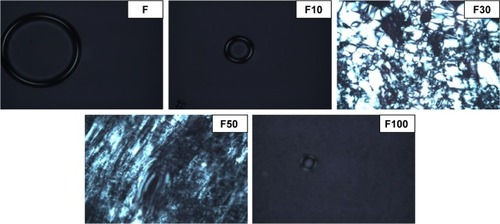
The results of photomicrographs of the formulations after adding 10%, 30%, 50% and 100% artificial saliva are shown in . These photomicrographs demonstrate that the addition of saliva caused the isotropic systems to change in anisotropic systems. The addition of 30% saliva caused the “Maltese crosses” to appear, indicating the formation of a lamellar LCS. The hexagonal LCS formation occurred after the addition of 50% saliva based on the appearance of ribbed structures. The addition of 100% saliva to the formulation caused a change in an isotropic system, however, due to its high viscosity, indicated by a cubic LCS (F).
Figure 1 Photomicrographs representing the effect of artificial saliva in the structure of F (liquid crystal system) by light polarized microscopy at 20% magnification.
Notes: F is the liquid crystal system; F10 is a 0.1:1 (wt/wt) dilution of F containing 10% artificial saliva; F30 is a 0.3:1 (wt/wt) dilution of F containing 30% artificial saliva; F50 is a 0.5:1 (wt/wt) dilution of F containing 50% artificial saliva; and F100 is a 1:1 (wt/wt) dilution of F containing 100% artificial saliva.
The flow and oscillatory characteristics of both F and F100 are shown in and , respectively. shows that F has a low viscosity, and when 100% saliva was added, F100 exhibited a high viscosity. In addition, it is also observed that F100 is potentially a thixotropic system, since the upward curve does not overlap the downward curve, indicating that F100 is more structured, because it needs a more time to return for its initial organization.
Figure 2 Rheograms of formulations F (squares) and F100 (triangles).
Notes: Ascendant curve, filled symbols; descendent curve, empty symbols. F is the liquid crystal system; F100 is a 1:1 (wt/wt) dilution of F containing 100% artificial saliva.
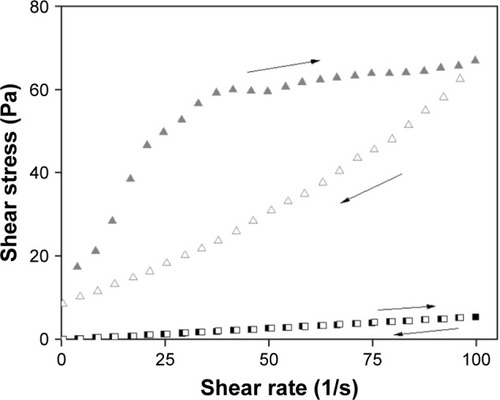
Figure 3 Variation of the storage module (G′, filled symbols) and loss module (G″, empty symbols) as a function of the frequency to F and F100.
Notes: F is the liquid crystal system; F100 is a 1:1 (wt/wt) dilution of F containing 100% artificial saliva.
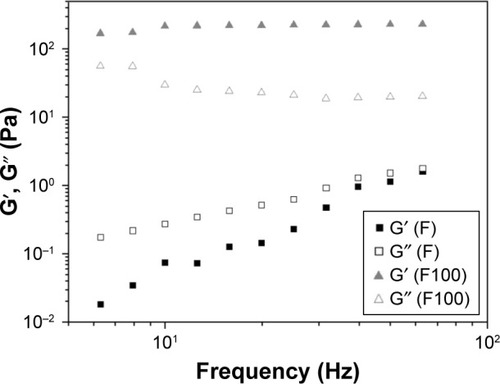
The frequency sweep test showed changes in the oscillatory properties of the formulations after adding 100% saliva, because F100 presented G′ greater than F. Moreover, G′ of F100 is much larger than G″, indicating that the incorporation of saliva increased the rigidity of F. Values of the bioadhesion test are presented in , indicating that the incorporation of 100% saliva into the F-system increased the bioadhesion strength and the work of bioadhesion on the surface of the bovine tooth five times larger than F.
Table 1 Results of in vitro bioadhesion strength in F and F100
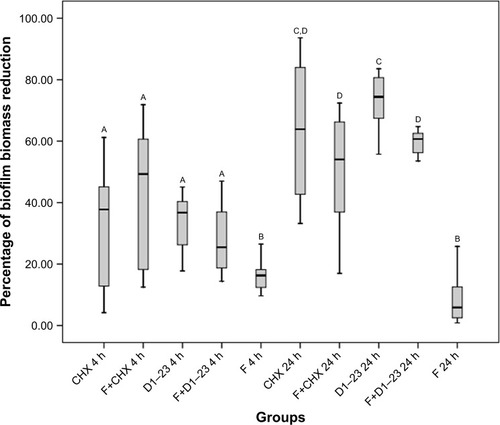
presents the values of MIC and MBC for the antimicrobial agent in solution, demonstrating that CHX was more effective in solution when compared to D1–23. Considering the biofilm assays, the percentage of S. mutans reduction in the biofilm after 4 and 24 h with the appropriated treatments is shown in . After 4 h of exposure, there was no statistical difference in the biofilm reduction comparing CHX and D1–23 incorporated in F and both agents in solution. After 24 h, no difference was observed comparing CHX in solution or incorporated into F, but higher biofilm reduction was noted for D1–23 in solution compared to D1–23 incorporated into F. Overall, biofilm reduction was higher in 24 h when compared to 4 h, suggesting a cumulative effect of antimicrobial agents when incorporated into F.
Table 2 MIC and MBC of D1–23 and CHX solution against planktonic S. mutans
Figure 4 Boxplot of the percentage of biofilm biomass reduction after 4 and 24 h of the treatment.
Notes: Bars indicate minimum and maximum values. Boxes indicate lower and upper quartiles. Line in the middle of boxes is median. A–DDifferent letters show statistical difference among the groups, according to Kruskal–Wallis/Mann–Whitney tests (p<0.05). F, liquid crystalline formulation; D1–23, peptide D1–23; F+D1–23, formulation+peptide D1–23; F+CHX, formulation+CHX.
Abbreviation: CHX, chlorhexidine diacetate.
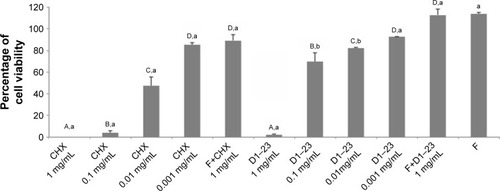
shows the cytotoxicity effects of the antimicrobial agents on epithelial cells. CHX and D1–23 solutions at 1 mg/mL were very cytotoxic, but when these agents were incorporated in F at 1 mg/mL concentration, cytotoxicity was not observed.
Figure 5 Mean (SD) of the percentage of epithelial cell viability after 24 h of the treatment.
Notes: A–DDifferent uppercase letters show statistical difference among the concentrations of the same agent, according to ANOVA/Tukey tests (p,0.05). a,bDifferent lowercase letters show statistical difference among CHX and D1–23 or F+CHX and F+D1–23, according to Student’s t-test (p<0.05). F, liquid crystalline formulation.
Abbreviations: ANOVA, analysis of variance; CHX, chlorhexidine diacetate.
Discussion
This is the first in vitro study investigating the applicability of LCS containing an AMP fragment on tooth surfaces aimed to prevent dental caries. All these characterization results indicated that, in contact with the saliva, F (LCS) presents a more structured system, with greater viscosity and better bioadhesive power on the tooth surface, which may increase the action of the peptide and improve the performance of the treatment.
Formulations composed of surfactant, an aqueous phase and an oil phase in different proportions can generate microemulsions, emulsions, liquid crystals or phase separation.Citation31 The identification of the liquid crystalline phase is fundamental in the development of drug delivery systems, because the mesophase structure may influence drug release. This study observed that the addition of saliva, ie, the increase in the concentration of aqueous phase of system, caused isotropic systems to convert to anisotropic systems. The structures observed in the anisotropic field, such as streaks and Maltese crosses, are referred to as hexagonal and lamellar, respectively, whereas the microemulsions and cubic mesophases are isotropic and visualized as dark field.Citation32 Maltese crosses starting to appear from the addition of 30% saliva indicate the formation of a lamellar LCS. The hexagonal LCS formation occurred after the addition of 50% saliva with the appearance of ribbed structures. The addition of 100% saliva in formulation caused a change to an isotropic system, indicated by a cubic LCS. The rigidity and high viscosity of the cubic phase retards diffusion and can provide a slow sustained release of the incorporated drug.Citation33
The continuous rheological analysis is a widely used method for characterizing delivery systems, because it evaluates the facility that the material flows from a bottle, pumping a product in an industrial process, the spreading of a cream or lotion on skin and passage of product through the hole of a syringe.Citation34 In the ascending curve, the flow behavior is classified into two types: Newtonian or non-Newtonian. The non-Newtonian flow can be further classified as pseudoplastic, dilatant or plastic. In the descending curve, the materials are classified as thixotropic or reopetic. Flow is classified as Newtonian when the shear stress and rate are constant, or its viscosity is constant.Citation35 The pseudoplastic flow occurs in materials that undergo a decrease in viscosity when the shear rate goes from low levels to higher levels. The increase in the shear rate guides rigid particles in the flow direction, creating shear thinning.Citation36 F was determined to have a Newtonian flow and low viscosity. When 100% saliva was added to F, F100 exhibited a non-Newtonian pseudoplastic behavior (n<1) and high viscosity. In addition, F100 was observed to have a thixotropic system, because the descending curve did not overlap the ascending curve, indicating that the system is more structured for F100 when compared to F.
The oscillatory analysis determined the viscoelastic properties of the formulations, providing information on the structural nature of the system, leading directly to the performance of the formulation. This information is obtained through the analysis of the elastic module (G′) and viscous module (G‴) obtained in this assay. The elastic module, G′, is termed as the storage module, representing both the energy stored during deformation when the tension increases and the energy released when the tension is relaxed. The G″ viscous module is the viscous element that cannot store energy because the applied tension is dissipated in the form of irreversible deformation.Citation37 In this current study, changes were observed in the oscillatory properties of the formulations after the addition of 100% saliva by using the frequency sweep test. plots the G′ storage module and the G″ loss module versus frequency. The F organization degree increases when 100% saliva was incorporated, the F100 value G′ module was higher than the F value G′ module. Furthermore, the F100 G′ storage module was greater than the G″ loss module, while the F value G′ module was less than the G″ module, indicating that the saliva incorporation increased the rigidity of the system.
The addition of bioadhesive system in drug delivery was able to prolong the time of action of the drug, reducing the frequency of application of the product and thus increasing patient compliance to treatment.Citation38 In our study, we observed that when 100% saliva was added, the formulation exhibited the best bioadhesive properties (). This characteristic obtained from the formulation is due to the use of Carbopol as a bioadhesive agent. Carbopol is a bioadhesive polymer derived from the polyacrylic acid commonly used in bioadhesive pharmaceutical hydrogels, owing to their hydrophilic nature and reticulated structure, which makes them interesting for controlling drug release.Citation22
The current study investigated the toxicity in epithelial cells and anti-biofilm activity against S. mutans of a CAMP fragment (D1–23) incorporated into a controlled drug delivery system, LCS (LCS or F in this study). AMP production is a major component of the innate immunity against infection that provides protection against bacteria, fungi, yeast and viruses.Citation39 These molecules have been shown to be promising agents in controlling microbial growth due to their low concentration and selective antimicrobial activity, as well as low rates of antimicrobial resistance induction.Citation40 S. mutans has been considered to be associated with dental cariesCitation41–Citation43 based on their acid production and acid tolerance.Citation3,Citation44
The peptide fragment (D1–23) was chosen based on a prior studyCitation45 testing the antimicrobial activity of various peptide fragments, including defensins and cathelicidins. The D1–23 fragment showed the best results against S. mutans when compared to the other peptide fragments. In the current study, we determined MIC and MBC values for this peptide fragment, showing that this peptide has an antimicrobial activity against S. mutans with low values of MIC/MBC. Several studies have demonstrated the antimicrobial activity of defensins against S. mutans.Citation46–Citation48 Maisetta et alCitation46 observed an S. mutans reduction of at least 3 log 10 after 1.5 h of incubation with 2 µg/mL hBD-3. Joly et alCitation47 determined MIC values ranging from 3.4 to 5 µg/mL of hBD-3 against S. mutans strains. Nishimura et alCitation48 found MBC<10 µg/mL of hBD-2 for several oral streptococci, including S. mutans. The mechanism of action of defensins against bacteria is through cell rupture and inhibition of lipopolysaccharide production.Citation40 Lower MIC/MBC values were also observed for CHX in this current study. The cationic molecule of CHX is attracted toward negatively charged bacterial cell wall. This interaction is able to modify the integrity of cell membrane and allows CHX binding to phospholipids in the inner membrane, which leads to increased permeability and entrance of ions such as potassium and a progressive damage to the membrane by increasing the concentration of CHX.Citation49
Despite all the advantages that AMPs have demonstrated, including activity at low concentrations and activity across a wide spectrum, there are some limitations to their therapeutic application. One limitation is related to the high cationic activity of peptides. The inhibitory action of AMPs seems to be significantly reduced in biological fluids such as plasma, serum or saliva,Citation40 while their chemical and physical stability may be compromised by external factors, requiring special attention to their efficacy and security.Citation50 Therefore, LCS has been used to load peptides. LCS has been studied more intensively as a carrier of bioactive molecules in medicine,Citation51 including applications for pulmonary drug delivery,Citation52 diabetes treatmentCitation16 and even AIDS treatment.Citation15 There are some reports in dentistry of using the drug delivery systems as the carrier of oral substances, with the majority of them being studied as an alternative for periodontal treatment.Citation33,Citation53 However, a few studies analyzed this specific system for oral application. Souza et alCitation54 evaluated an LCS as a carrier for an antiseptic poly(hexamethylene biguanide) hydrochloride (PHMB). They observed that this system improved residence time and modulated drug release, indicating the use of this drug delivery system for PHMB.
With regard to cytotoxicity, the D1–23 and CHX solutions at 1 mg/mL were toxic for epithelial cells; however, both agents did not affect cell metabolism at low concentrations. D1–23 showed toxicity against two epithelial cell lines at concentrations >0.2 mM.Citation45 In this study, even at high concentrations, when both antimicrobial agents were incorporated into LCS, they did not have a cytotoxic effect on epithelial cells. This occurs because LCS was not cytotoxic, and low concentrations of peptide and CHX are released from LCS. Any cytotoxic effect was observed when these LCSs were applied on macrophage cultures.Citation55
Our main objective was to evaluate whether the LCS would work as a carrier, and if it could slowly release the antimicrobial agent and consequently have a cumulative effect. The current results indicate that the peptide fragment D1–23 in solution and in LCS reduced the S. mutans biofilm growth in both times of exposures (after 4 and 24 h); however, we should emphasize that the concentration selected for the D1–23 and CHX solutions was 1 mg/mL, regardless of the MBC. MIC/MBC assays of the tested agents showed that CHX had greater effect at lower concentrations when compared to D1–23. This means that the bactericidal concentration of CHX used in the biofilm assays was much higher than for D1–23. Even so, D1–23 presented similar results to CHX in both times of exposure. The concentration of both agents incorporated into LCS was also 1 mg/mL. Data from literature report that the release of agents from this LCS is around 4% at 24 h.Citation26 Although data from the release of antimicrobial agents were not available in this current study, the peptide and CHX release from LCS was probably >4%, since the formulation was diluted before incorporation of antimicrobial agents for biofilm assays to reduce viscosity. Even so, D1–23 at 1 mg/mL into LCS presented similar antibiofilm activity to D1–23 in solution after 4 h. D1–23 into LCS increased the residence time of the antimicrobial agent but did not potentiate the antimicrobial effect. We believe that the antimicrobial agents interact with the LCS promoting a cumulative effect of D1–23.
Other studies are necessary to confirm the effectiveness of LCSs for oral applications, perhaps using different methodologies promoting more time of contact between the antimicrobial agent and the site of action (tooth surface).
Conclusion
The current study developed and characterized an LCS with bioadhesive properties. Fragment of hBD-3, D1–23, incorporated in this LCS did not promote cytotoxic effect on epithelial cells. In solution, D1–23 had a similar effect on S. mutans biofilm compared to CHX, however, when this peptide was incorporated into LCS, promoted a cumulative antibiofilm effect, indicating that this drug delivery system might be a promising carrier to CAMP. This delivery system could be professionally used by dentists as a tool for biofilm control in patients with high risk to develop dental caries.
Acknowledgments
This study was funded by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP; grants #2012/19235-5, #2013/12285-0, #2013/07600-3 and #2013/01565-1).
The authors would like to thank professors Robson Frederico Cunha and Sandra Maria Herondina Ávila de Aguiar for their contributions to this study.
Disclosure
The authors report no conflicts of interest in this work.
References
- FejerskovOConcepts of dental caries and their consequences for understanding the diseaseCommunity Dent Oral Epidemiol19972515129088687
- TakahashiNNyvadBThe role of bacteria in the caries process: ecological perspectivesJ Dent Res201190329430320924061
- HamadaSSladeHDBiology, immunology, and cariogenicity of Streptococcus mutansMicrobiol Rev19804423313846446023
- FreiresIARosalenPLHow natural product research has contributed to oral care products development? A critical viewPharm Res20163361311131726975359
- GorrSUAbdolhosseiniMAntimicrobial peptides and periodontal diseaseJ Clin Periodontol201138Suppl 1112614121323710
- NiyonsabaFUshioHNakanoNAntimicrobial peptides human beta-defensins stimulate epidermal keratinocyte migration, proliferation and production of proinflammatory cytokines and chemokinesJ Invest Dermatol2007127359460417068477
- MccormickTSWeinbergAEpithelial cell-derived antimicrobial peptides are multifunctional agents that bridge innate and adaptive immunityPeriodontol 2000201054119520620712640
- WiesnerJVilcinskasAAntimicrobial peptides – the ancient arm of the human immune systemVirulence20101544046421178486
- OuharaKKomatsuzawaHYamadaSSusceptibilities of periodontopathogenic and cariogenic bacteria to antibacterial peptides, {beta}-defensins and LL37, produced by human epithelial cellsJ Antimicrob Chemother200555688889615886266
- GordonYJRomanowskiEGMcDermottAMA review of antimicrobial peptides and their therapeutic potential as anti-infective drugsCurr Eye Res200530750551516020284
- ZhangLFallaTJHost defense peptides for use as potential therapeuticsCurr Opin Investig Drugs2009102164171
- ReynoldsNLDe CeccoMTaylorKPeptide fragments of a β-defensin derivative with potent bactericidal activityAntimicrob Agents Chemother20105451922192920176896
- BhardwajVKumarMNVRFundamentals and applications of controlled release drug delivery advancesSiepmannJSiegelRARathboneMJDelivery Science and TechnologyNew YorkSpringer2012493516
- LestiniBJSagnellaSMXuZSurface modification of liposomes for selective cell targeting in cardiovascular drug deliveryJ Control Release2002781–323524711772464
- AvachatAMParpaniSSFormulation and development of bicontinuous nanostructured liquid crystalline particles of efavirenzColloids Surf B Biointerfaces2015126879725543986
- OkawaraMHashimotoFTodoHEffect of liquid crystals with cyclodextrin on the bioavailability of a poorly water-soluble compound, diosgenin, after its oral administration to ratsInt J Pharm20144721–225726124954725
- BernegossiJCalixtoGMSanchesPRPeptide KSL-W-loaded mucoadhesive liquid crystalline vehicle as an alternative treatment for multispecies oral biofilmMolecules2015211E3726712726
- CalixtoGMGarciaMHCilliEMChiavacciLAChorilliMDesign and characterization of a novel p1025 peptide-loaded liquid crystalline system for the treatment of dental cariesMolecules2016212E15826828470
- GuterresSSAlvesMPPohlmannARPolymeric nanoparticles, nanospheres and nanocapsules, for cutaneous applicationDrug Target Insights2007214715721901071
- MarquesMRCLoebenbergRAlmukainziMSimulated biological fluids with possible application in dissolution testingDissolution Technologies201181528
- SalmaziRCalixtoGBernegossiJRamosMABauabTMChorilliMA curcumin-loaded liquid crystal precursor mucoadhesive system for the treatment of vaginal candidiasisInt J Nanomedicine2015104815482426257519
- CalixtoGYoshiiACRocha e SilvaHStringhetti Ferreira CuryBChorilliMPolyacrylic acid polymers hydrogels intended to topical drug delivery: preparation and characterizationPharm Dev Technol201520449049625975700
- MerrifieldRBSolid phase peptide synthesis. I. The synthesis of a tetrapeptideJ Am Chem Soc1963851421492154
- KaiserEColescottRLBossingerCDCookPIColor test for detection of free terminal amino groups in the solid phase synthesis of peptidesAnal Biochem19703425955985443684
- CruscaERezendeAAMarchettoRInfluence of N-terminus modifications on the biological activity, membrane interaction, and secondary structure of the antimicrobial peptide Hylin-a1Biopolymers2011961414820560142
- HuFQHongYYuanHPreparation and characterization of solid lipid nanoparticles containing peptideInt J Pharm20042731–2293515010127
- GawandePVLeungKPMadhyasthaSAntibiofilm and antimicrobial efficacy of DispersinB®-KSL-W peptide-based wound gel against chronic wound infection associated bacteriaCurr Microbiol201468563564124445333
- CLSI – Clinical and Laboratory Standard InstituteMethods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically9th edWayne, PACLSI Document2012M7M9
- Mattos-GranerRONapimogaMHFukushimaKDuncanMJSmithDJComparative analysis of Gtf isozyme production and diversity in isolates of Streptococcus mutans with different biofilm growth phenotypesJ Clin Microbiol200442104586459215472313
- BedranTBMayerMPSpolidorioDPGrenierDSynergistic anti-inflammatory activity of the antimicrobial peptides human beta- defensin-3 (hBD-3) and cathelicidin (LL-37) in a three-dimensional co-culture model of gingival epithelial cells and fibroblastsPLoS One201499e10676625187958
- LawrenceMJReesDGMicroemulsions-based as novel drug delivery systemsAdv Drug Deliv Rev20004518912111104900
- CalixtoGMFDesenvolvimento e caracterização de sistemas nano-estruturados bioadesivos contendo peptídeo análogo à adesina do Streptococcus mutans [Development and characterization of nano-structured bioadhesives containing peptide analogue to Streptococcus mutans adhesin; dissertation]Araraquara, BrazilSão Paulo State University2013 Portuguese
- ShahJCSadhaleYChilukuriDMCubic phase gels as drug delivery systemsAdv Drug Deliv Rev2001472–322925011311994
- PestanaKCMicroemulsões biocompatíveis de anfotericina b para administração oral. Estudo estrutural, liberação in vitro e farmacocinética pré-clínica [tesis]Araraquara, BrazilSao Paulo State University2009
- SchrammGReologia e Reometria. Fundamentos Teóricos e Práticos [Rheology and Rheometry. Theoretical and Practical Fundamentals]São Paulo, BrazilArtliber2006 Portuguese
- SavicSLukicMJaksicIReichlSTamburicSMüller-GoymannCAn alkyl polyglucoside-mixed emulsifier as stabilizer of emulsion systems: the influence of colloidal structure on emulsions skin hydration potentialJ Colloid Interface Sci2011358118219121421214
- PènzesTRheological analysis of the structural properties effecting the percutaneous absorption and stability in pharmaceutical organogelsRheol Acta200443457463
- SmartJDRileyRGTsibouklisJThe retention of C-labelled poly(acrylic acids) on gastric and oesophageal mucosa: an in vitro studyEur J Pharm Sci20032018990
- Pinheiro da SilvaFMachadoMCAntimicrobial peptides: clinical relevance and therapeutic implicationsPeptides201236230831422659161
- da SilvaBRde FreitasVANascimento-NetoLGAntimicrobial peptide control of pathogenic microorganisms of the oral cavity: a review of the literaturePeptides201236231532122664320
- TanzerJMLivingstonJThompsonAMThe microbiology of primary dental caries in humansJ Dent Educ200165101028103711699974
- GuptaPGuptaNPawarAPBirajdarSSNattASSinghHPRole of sugar and sugar substitutes in dental caries: a reviewISRN Dent2013201351942124490079
- NyvadBCrielaardWMiraATakahashiNBeightonDDental caries from a molecular microbiological perspectiveCaries Res20134728910223207320
- BeckerMRPasterBJLeysEJMolecular analysis of bacterial species associated with childhood cariesJ Clin Microbiol20024031001100911880430
- KrelingPFAidaKLMassunariLCytotoxicity and the effect of cationic peptide fragments against cariogenic bacteria under planktonic and biofilm conditionsBiofouling2016329995100627538256
- MaisettaGBatoniGEsinSActivity of human β-defensin 3 alone or combined with other antimicrobial agents against oral bacteriaAntimicrob Agents Chemother200347103349335114506056
- JolySMazeCMcCrayPBJrGuthmillerJMHuman β-defensin 2 and 3 demonstrate strain-selective activity against oral microorganismsJ Clin Microbiol20044231024102915004048
- NishimuraEEtoAKatoMOral streptococci exhibit diverse susceptibility to human β-defensin – 2: antimicrobial effects of hBD-2 on oral streptococciCurr Microbiol2004482858715057473
- PrasannaSGVLakshamananRCharacteristics, uses and side effect of chlorhexidine: a reviewJ Dent Med Sci20161565759
- DaileyLAWittmarMKisselTThe role of branched polyesters and their modifications in the development of modern drug delivery vehiclesJ Control Release20051011–313714915588900
- ChenYMaPGuiSCubic and hexagonal liquid crystals as drug delivery systemsBiomed Res Int2014201481598124995330
- PatilSSMahadikKRParadkarARLiquid crystalline phase as a probe for crystal engineering of lactose: carrier for pulmonary drug deliveryEur J Pharm Sci201568435025460546
- HorevBKleinMIHwangGpH-activated nanoparticles for controlled topical delivery of farnesol to disrupt oral biofilm virulenceACS Nano2015932390240425661192
- SouzaCWatanabeEBorgheti-CardosoLNde Abreu FantiniMCLaraMGMucoadhesive system formed by liquid crystals for buccal administration of poly(hexamethylene biguanide) hydrochlorideJ Pharm Sci2014103123914392325336429
- OliveiraMBCalixtoGGraminhaMCerecettoHGonzálezMChorilliMDevelopment, characterization, and in vitro biological performance of fluconazole-loaded microemulsions for the topical treatment of cutaneous leishmaniasisBiomed Res Int2015201539689425650054
