 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
Buccal delivery of insulin is still a challenging issue for the researchers due to the presence of permeability barrier (buccal mucosa) in the buccal cavity. The main objective of this study was to investigate the safety, effectiveness, and potential of various liposomes containing different bile salts to improve the permeation of insulin across in vitro TR146 buccal cell layers.
Methods
Elastic bilosomes containing soy lecithin and bile salt edge activators (sodium cholate [SC], sodium taurocholate [STC], sodium glycocholate [SGC], sodium deoxyglycocholate [SDGC], or sodium deoxytaurocholate [SDTC]) were fabricated by thin-film hydration method. The prepared liposomes were characterized, and in vitro permeation studies were performed. The fluorescein isothiocyanate-insulin-loaded elastic bilosomes were used to evaluate the quantitative and qualitative cellular uptake studies.
Results
The prepared elastic bilosomes had a particle size and an entrapment efficiency of ~140–150 nm and 66%–78%, respectively. SDGC-lipo (SDGC-incorporated liposome) was observed to be the most superior with an enhancement ratio (ER) of 5.24 (P<0.001). The SC-incorporated liposome (SC-lipo) and SDTC-incorporated liposome (SDTC-lipo) also led to a significant enhancement with ERs of 3.20 and 3.10 (P<0.05), respectively, compared with insulin solution. These results were further supported by quantitative and qualitative cellular uptake studies performed employing fluorescence-activated cell sorting analysis and confocal microscopy, respectively. The relative median fluorescence intensity values of elastic bilosomes were counted in the order of SDGC-lipo > SC-lipo > SDTC-lipo > SGC-incorporated liposome > STC-incorporated liposome, and similarity in the permeability profile of the employed elastic bilosomes was noted.
Conclusion
This study presents the employment of various derivatives of cholic acid-loaded elastic bilosomes as a promising strategy to enhance the permeation of insulin through buccal route.
Introduction
As per the statistics released by the International Diabetes Federation, 425 million people were affected by diabetes worldwide in 2017. The prevalence is expected to increase to 629 million by 2045, rendering diabetes as a serious health concern in the world.Citation1 It is reported that diabetes is a major cause for several chronic diseases such as heart attacks, kidney failure, blindness, stroke, and lower limb amputation.Citation2 Insulin is the promising and most common medication used for the treatment of diabetes. It is administered to patients through a subcutaneous route with multiple daily injections, creating physical and mental burden on patients, and it reduces patient compliances and desired therapeutic outcome.Citation3–Citation5 Despite the advancements in innovative therapeutic approaches in pharmaceutical field, the noninvasive buccal delivery of biopharmaceuticals, particularly insulin, is still a major challenge.Citation6 However, the presence of well-vascularized tissues, blood vessels draining directly into the jugular vein, and less proteolytic enzymes and bypassing the first-pass effects in the buccal mucosa as compared to gastrointestinal tract project the transbuccal delivery as a desired site for the delivery of biopharmaceuticals.Citation7,Citation8 Further, based on the ease of administration, short cellular turnover time of 4–14 days, and high patient compliances, transbuccal delivery has recently garnered an increasing attention worldwide.Citation9
After multiple attempts, various pharmaceuticals have been registered for buccal drug delivery and commercialized in the market. For instances, Breakyl®, Setofilm®, Chloraseptic®, Donepezil Hexal®, Risperidone Hexal®, Triaminic®, and Theraflu® have been commercialized.Citation10 In addition, several buccal products are on clinical trials such as buccal prochlorperazine (Phase III), buccal misoprostol (Phase IV), buccal midazolam (Phase IV), and Generex’s Oral-lyn™ insulin spray (Phase III).Citation11 Oral-lyn™ insulin spray, a mixed micelles liquid formulation with sodium caprate and bile salts as an enhancer, has already been approved for marketing in Ecuador and Lebanon.Citation12,Citation13 The growing interest in the area of transbuccal delivery over the last two decades prompted us toward the initiation of study on buccal delivery of biopharmaceuticals. In our previous studies, we have demonstrated the successful delivery of salmon calcitonin along with chemical enhancers or in combination with iontophoresis across the buccal mucosa both in vitro and in vivo in rabbits.Citation5,Citation14
Various nanovesicular systems have been greatly investigated to evade the absorption barriers as well as to enhance the bioavailability of protein/peptide drugs.Citation15,Citation16 Among these systems, liposomes have already demonstrated their efficiency in increasing the bioavailability of various drugs in several studies.Citation17–Citation23 Since bile salts stabilize the vesicles and increase the fluidity of biomembrane as well as internalization of vesicles, their uses in liposomes-based delivery are on a constant rise.Citation24 The tissue damages caused by bile salts are reversible; thus, they have been used abundantly to enhance the permeation of various pharmaceuticals across the buccal mucosa.Citation25 In general, it has been reported that the bile salts enhance the absorption of drugs by the extraction of the membrane protein or lipids, membrane fluidization, forming reverse micelles in the membrane, and inducing aqueous channels.Citation26,Citation27 Bilosomes are a novel colloidal delivery system formed by the incorporation of bile salts into liposomes.Citation17 Bilosomes are more elastic, flexible, and ultra-deformable than conventional liposomes.Citation28 Recently, several studies using bilosomes have shown promising potential in the delivery of insulin across different alternative routes such as oral, transdermal, and buccal.Citation29 In different studies, Niu et al incorporated three different bile salts in liposomes and revealed that sodium glycocholate (SGC)-incorporated liposomes (SGC-lipo) exhibited high potency for the oral delivery of insulin than sodium taurocholate (STC), sodium deoxycholate (SDC), or conventional liposomes.Citation30,Citation31 It has also been reported that SGC-lipo was the most superior in protecting gastrointestinal tract against enzymatic degradation, and this property was the main mechanism in enhancing the oral bioavailability of insulin.Citation32,Citation33 Furthermore, the enhanced oral bioavailability of insulin,Citation34,Citation35 cyclosporine A,Citation18 and itraconazoleCitation36 has been demonstrated by employing liposomes containing bile salts. Similarly, bilosomes incorporating various drugs have shown their efficient applicability toward a transdermal route such as insulin,Citation37 methotrexate,Citation28 and tenoxicam.Citation38 Additionally tacrolimus-loaded bilosomes have been successfully designed to function as an ocular delivery system.Citation39 Moreover Yang et al revealed that the SDC-incorporated liposomes (SDC-lipo) had a promising approach on the buccal delivery of insulin than conventional liposomes.Citation29 To the best of our knowledge, this is the first report on the buccal delivery of insulin-loaded bilosomes. Accordingly, it is hypothesized that our study might be another milestone in demonstrating the delivery of insulin employing different bile salt-loaded liposomes through a buccal route.
Due to variation in the thickness of individual’s buccal mucosae of porcine, cell model was selected.Citation4 TR146 cell culture model was used as an in vitro model, as the TR146 cells form a multilayered squamous epithelium resembling human buccal epithelium.Citation40,Citation41 In the present study, different derivatives of cholic acids were used to prepare different elastic bilosomes. summarizes the chemical structures and molecular weights of different derivatives of cholic acids used in this experiment. The main aim of this study was to investigate the safety, effectiveness, and potential of various liposomes containing different bile salts to improve the permeation of insulin across in vitro TR146 buccal cell layers.
Table 1 Properties of different derivatives of cholic acids used in the experiment
Materials and methods
Materials
Human insulin was purchased from ProSpec-Tany Techno-Gene Ltd. (Ness-Ziona, Israel). Soy lecithin (Solec 2F-UB) was purchased from Bunge North America, Inc. (Chesterfield, MO, USA). Sodium cholate (SC) and STC were purchased from Alfa Aesar (Heysham, UK). SGC and sodium deoxytaurocholate (SDTC) were purchased from Acros Organics (Morris Plains, NJ, USA). Fluorescein isothiocyanate-labeled insulin (FITC-insulin) and sodium deoxyglycocholate (SDGC) were purchased from Sigma-Aldrich (St Louis, MO, USA). TR146 cell line was purchased from Public Health England (London, UK). Hank’s balanced salt solution (HBSS), fetal bovine serum (FBS), Ham’s F-12 nutrient, and trypsin–ethylenediaminetetraacetic acid (EDTA; 0.25%) were purchased from WELGENE Inc. (Gyeongsan, Republic of Korea). All other chemicals were of reagent-grade and used without further purification.
Fabrication of elastic bilosomes
Elastic bilosomes were fabricated using a previously published thin-film hydration method with a slight modification.Citation42 Briefly, soy lecithin and bile salt edge activators (SC, STC, SGC, SDGC, and SDTC; 85:15 w/w%) were dissolved in chloroform and methanol (3:1) in a round-bottom flask. The organic solvent was removed by rotary vacuum evaporation above the lipid transition temperature. The remaining traces of dry film were removed under nitrogen gas. Subsequently, the dry lipid film was hydrated with insulin solution (1.82 mg/mL) for 30–40 minutes under water bath at 35°C. Thus, prepared multilamellar liposome was extruded five times through a 200-nm polycarbonate membrane filter for homogeneous size distribution and efficient entrapment.
Particle characterization
The mean particle size, polydispersity index (PDI), and ζ potential were determined using dynamic light scattering (DLS) with a NanoBrook ZetaPALS (Version 5.69; Brookhaven Instruments Corp., Holtsville, NY, USA). Elastic bilosomes were diluted to 1:50 with distilled water, and the light scattering property was measured promptly. All measurements were performed under ambient conditions and in triplicate.
Entrapment efficiency (EE) and loading capacity (LC)
The efficiency of insulin entrapment in various elastic bilosomes was calculated by determining the free and total amount of insulin initially added in the formulations. Briefly, 1 mL of insulin-loaded liposome was placed in a centrifuge bottle (Beckman Coulter Inc., Carlsbad, CA, USA) and diluted with 9 mL of PBS of pH 7.4. Then, it was centrifuged at 200,000× g for 2 hours at 4°C (Beckman Optima™ LE-80K Ultracentrifuge). Insulin concentration in each sample was determined by Quantikine® enzyme-linked immunosorbent assay (ELISA; DINS00; R&D Systems Inc., Minneapolis, MN, USA). Finally, the drug EE and LC were calculated based on the following equations, respectively:
Deformability of elastic bilosomes
The comparative measurement of deformability of different elastic bilosomes was carried out against the standard liposomes (control) preparation using single syringe infusion pump (KDS 100 series; KD Scientific Inc., Holliston, MA, USA).Citation43 One end of the syringe pump was fixed on the wall, and another end was adjusted by the home-built device so that it can withstand the pressure generated by the extruder. The vesicles were extruded through 50-nm polycarbonate membranes at a constant flow rate of 15.55 mL/h. The size of vesicles was measured by DLS with a NanoBrook ZetaPALS (Version 5.69). The deformability index (D) of elastic bilosomes was obtained as follows:
Cell lines and cell culture conditions
Human TR146 (passages #11–20) cells were used for in vitro cellular studies. The cells were cultured in Ham’s F-12 supplemented with 10% FBS, 2 mM glutamine, penicillin (10,000 units/mL), and streptomycin (10,000 µg/mL) and incubated at 37°C under 5% CO2 and 95% air. The media were replaced every 2–3 days. At 70%–80% confluency, cells were split using 0.25% trypsin–EDTA.
Cell viability studies
The in vitro cell cultures of TR146 cells were subjected to a 2,3-bis-(2-methoxy 4-nitro-5-sulfophenyl)–2H-tetrazolium-5-carboxanilide salt (XTT) containing N-methyl dibenzopyrazine methyl sulfate (PMS) Cell Proliferation Assay Kit (PanReac AppliChem Co., Barcelona, Spain) in order to quantify viability. The cells were seeded in 96-well plates at a density of 2×104 cells per well and incubated for 24 hours at 37°C. After 24 hours, the media were removed, and 150 µL of solution, containing various blank liposomes of different bile acids, with different concentrations was added to each well. Subsequently, the cells were incubated for 8 hours (the duration of permeability experiments). Then, 50 µL of reaction mixture (XTT and PMS reagent) was added to each well and incubated for further 4 hours at 37°C. Absorbance was read at 450 nm (reference absorbance at 690 nm) using a microplate reader.
Cell viability was calculated as follows:
Transepithelial electrical resistance (TEER)
In order to evaluate the integrity of the TR146 cell layers, before and after each transport during permeability studies, TEER was monitored. It was calculated by measuring resistance (R in Ω) using a Millicell® ERS-2 (Electrical Resistance System; EMD Millipore Corporation, Billerica, MA, USA) according to the manufacturer’s instruction. The TEER value was obtained as follows:
In vitro cell permeation studies
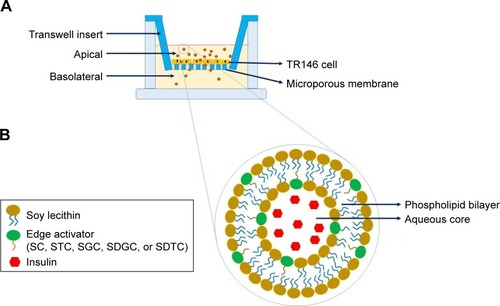
The permeability studies were performed as described by Iyire et al with a slight modification ().Citation3 The studies were done across TR146 cell layers from apical (0.5 mL) to baso-lateral direction (1.5 mL) in HBSS–hydroxyethylpiperazine ethane sulfonic acid (HEPES) buffer (pH 7.4). The cells were seeded across 12-well Transwell® inserts (Corning Inc., Corning, NY, USA) at a density of 5×104 cells/cm2, and the medium was replaced every subsequent day until the formation of the monolayer (26–30 days). Typically, 500 µL of 1.25 mg/mL insulin-loaded liposomes (SC-incorporated liposomes [SC-lipo], STC-incorporated liposomes [STC-lipo], SGC-lipo, SDGC-incorporated liposomes [SDGC-lipo], or SDTC-incorporated liposomes [SDTC-lipo]) was added to the apical chamber of the Tran-swell and kept at 37°C. At different time points (0.5, 1, 2, 4, 6, and 8 hours), 500 µL of sample was withdrawn from the basolateral chamber and replaced by the same volume of HBSS–HEPES buffer (pH 7.4) to retain the constant volume of the medium. The amount of permeated insulin across TR146 cell layers was determined by a Quantikine® ELISA (DINS00, R&D systems).
Figure 1 Schematic illustration of the delivery of insulin across TR146 cell layers on a Transwell (A) and elastic bilosomes (B).
Abbreviations: SC, sodium cholate; SDGC, sodium deoxyglycocholate; SDTC, sodium deoxytaurocholate; SGC, sodium glycocholate; STC, sodium taurocholate.
The steady state flux (Js), permeability coefficient (Kp), and enhancement ratio (ER) were calculated from the linear part of the permeation curve as described by Oh et al.Citation5
Js was obtained from EquationEquation 6(6) , where Qr is the total permeated insulin (ng), A is the cross-sectional diffusion area (cm2), and t is the time of exposure (hour).
Kp was calculated using EquationEquation 7(7) , where Js is the flux from the steady state (ng·cm−2·h−1), and Cd is the initial concentration in the donor chamber (ng·cm−3). Finally, ER was obtained by dividing the Kp value of each formulation with that of the control.
Cellular uptake studies
Fluorescence-activated cell sorting analysis (FACS) was used to study the cellular uptake characteristics of TR146 cells. The cells were seeded at a density of 3×105 cells per well in a 12-well plate and incubated for 24 hours in a humidified incubator under 5% CO2 atmosphere at 37°C. Then, the cells were treated with FITC-insulin-loaded liposomes and incubated for 8 hours. Subsequently, the cells were washed twice with HBSS–HEPES buffer (pH 7.4) to remove the traces of liposomal vesicles left in the wells, harvested, and suspended in 0.5 mL of ice-cold FACS buffer (10% FBS and 2% sodium azide in PBS, pH 7.4). The dispersed cells were introduced immediately to FACS analysis using BD FAC suit software (BD Biosciences, San Jose, CA, USA). For the quantification of median fluorescence intensity (MFI) values, 5×103 designated cells were collected per histogram.
Interaction of various elastic bilosomes with TR146 cells
The cell–particle interactions were analyzed using FITC-insulin with confocal laser scanning microscopy (CLSM; Leica Microsystems, Wetzlar, Germany). For CLSM, TR146 cells were seeded at a density of 5×104 cells per well in an 8-chamber cell culture slide (SPL Life Sciences Co., Ltd., Pocheon, South Korea) and incubated for 24 hours. Then, the cells were treated with FITC-insulin-loaded liposomes and further incubated for 2 hours. Following incubation in a humidified incubator under 50% CO2 atmosphere at 37°C for an appropriate time, the cells were washed thrice with HBSS–HEPES buffer (pH 7.4), and plasma membrane was stained by adding 150 µL of Cell Mask™ Deep Red for 20 minutes. Subsequently, the cells were rinsed four times with HBSS–HEPES buffer (pH 7.4), and 150 µL of 4′,6-diamidino-2-phenylindole (DAPI) was added in order to stain the nuclei of cells and further incubated for 10 minutes at 37°C. Next, the cells were washed thrice with HBSS–HEPES buffer (pH 7.4) to remove the excess staining solution and fixed with 4% paraformaldehyde solution for 10 minutes in the dark as well as fixed by coverslips using the mounting medium (Dako North America, Inc., Carpinteria, CA, USA) and observed by CLSM.
Statistical analysis
The results are expressed as the mean ± SD. The one-way analysis of variance (ANOVA) followed by Tukey’s multiple comparison test was used to determine the level of statistical significance between the groups. For all data, a single, double, or triple asterisk was used if the P-value was <0.05, <0.01, or <0.001 level of significance, respectively.
Result and discussion
Preparation and characterization of elastic bilosomes
Various amphiphilic molecules are used as edge activators to provide deformability to vesicles. These vesicles are capable of squeezing through the intercellular regions of biomembrane.Citation45,Citation46 Hydrophilic surfactants such as bile salts and TWEEN® 80 possess more deformability than lipophilic surfactant due to the formation of transient holes in lipid bilayers by enhancing the biomembrane fluidity.Citation43,Citation47 Lipid vesicles fabricated using phospholipid and edge activators at a ratio of 85:15 (w/w%) induced highest deformability.Citation28,Citation43,Citation44,Citation46 Different derivatives of cholic acid were chosen as edge activators for comparison and study their effects on the deformability and permeation enhancement. Elastic bilosomes containing bile salts such as SC, STC, SGC, SDGC, or SDTC at a ratio of 85:15 w/w% were successfully prepared by thin-film hydration method. These liposomal formulations were evaluated with respect to vesicular size, PDI, ζ potential, EE, and LC as shown in . On average, the vesicular size was ~140–150 nm that is considered as an ideal size to achieve permeation across biomembrane.Citation48 It is well known that PDI parameter is used to determine the level of homogeneity. PDI values <0.1 are considered as monodispersion of liposomal vesicles and >0.1 is considered as polydispersion of liposomal vesicles.Citation49 All the prepared liposomes belonged to monodispersion category, ie, particles were supposed to be of same size, more narrow, and homogeneously distributed. All elastic bilosomes were negatively charged, and the ζ values were much higher, leading to the formation of a physically stable system, due to the presence of negatively charged bile salts. Our results were in accordance with many published types of research, and a similar trend was observed with regard to higher ζ potential values of liposomes prepared using STC and SGC.Citation17,Citation18,Citation36,Citation39 The EE and LC werê66%–78% and ~0.11%–0.14%, respectively. These results indicate that the prepared elastic bilosomes successfully encapsulated higher amount of insulin.
Table 2 Physical characteristics of various elastic bilosomes employed in the study
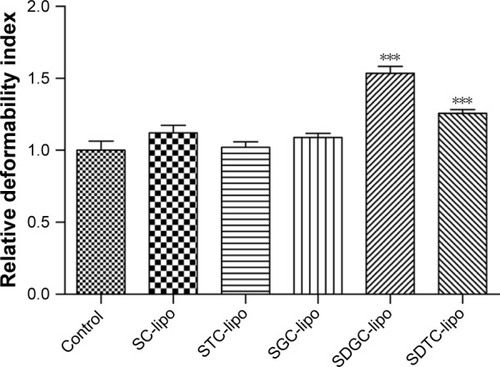
Deformability of different elastic bilosomes
Deformability is the crucial parameter of elastic bilosomes which facilitates the permeation across biomembrane pores smaller than their diameter.Citation48 It has been reported that stress-dependent adaptability and shape modification in an elastic bilosome can be expressed by deformability index (D).Citation42 In the present study, we have calculated the relative deformability as compared with the control. Since 100% soy lecithin or soy lecithin/cholesterol (85:15 w/w%) were not successfully fabricated, we preferred the minimum amount of STC (5%) to fabricate control liposome (soy lecithin/STC =95:5 w/w%). presents the relative deformability indices of several elastic bilosomes. The relative deformability indices were in the order of SDGC-lipo > SDTC-lipo > SC-lipo > SGC-lipo > STC-lipo. The significant differences in relative deformability indices were observed in SDGC-lipo (P<0.001) and SDTC-lipo (P<0.001) with respect to control. However, there were no significant differences in the relative deformability indices between each group except in the cases of SDGC-lipo and SDTC-lipo.
Figure 2 Relative deformability of different elastic bilosomes.
Notes: Error bars represent SD (n=3). ***P<0.001 vs control.
Abbreviations: SC-lipo, sodium cholate-incorporated liposomes; SDGC-lipo, sodium deoxyglycocholate-incorporated liposomes; SDTC-lipo, sodium deoxy-taurocholate-incorporated liposomes; SGC-lipo, sodium glycocholate-incorporated liposomes; STC-lipo, sodium taurocholate-incorporated liposomes.
In vitro cell viability studies
The in vitro cell viability of blank liposomes (SC-lipo, STC-lipo, SGC-lipo, SDGC-lipo, and SDTC-lipo) at different concentrations (10.00, 5.00, 2.50, and 1.25 mg/mL) was tested across TR146 cells, and presents the results. Trihydroxy bile salt-loaded liposomes (SC-lipo, SGC-lipo, and STC-lipo) at concentrations <5 mg/mL did not induce cytotoxicity. However, SC-lipo and STC-lipo induced significant cytotoxicity at a concentration of 5 mg/mL (P<0.001 and P<0.01, respectively), whereas all these three liposomes induced significant cytotoxicity at a concentration >5 mg/mL (P<0.001). Similarly, dihydroxy bile salt-loaded liposomes (SDGC-lipo and SDTC-lipo) at a concentration >1.25 mg/mL induced cytotoxicity at a concentration-dependent manner.Citation39,Citation50 These results were in accordance with the observations of some published researches. Lee and Yamamoto revealed that trihydroxy bile salts showed less toxicity than dihydroxy bile salts.Citation51 In another study by Duchateau et al, taurocholate was demonstrated as relatively safe, less toxic with no effect on ciliary arrest for 30 minutes at 30 mM concentration; whereas deoxycholate induced serious ciliotoxicity at a concentration of 5 mM for intranasal delivery of gentamicin.Citation52 Furthermore, Morimoto et al reported that SGC can be a safe and useful enhancer, even at 20 mM, for intratracheal drug delivery in rabbit tracheas.Citation53 In addition, Gordon et al demonstrated that glycine and taurine conjugates of bile salts are relatively less irritating for insulin delivery across nasal mucosa.Citation54
Figure 3 Cell viability of TR146 cells exposed to different concentrations of various elastic bilosomes.
Notes: Error bars represent SD (n=5). **P<0.01 versus control and ***P<0.001 versus control.
Abbreviations: SC-lipo, sodium cholate-incorporated liposomes; SDGC-lipo, sodium deoxyglycocholate-incorporated liposomes; SDTC-lipo, sodium deoxytaurocholate-incorporated liposomes; SGC-lipo, sodium glycocholate-incorporated liposomes; STC-lipo, sodium taurocholate-incorporated liposomes.
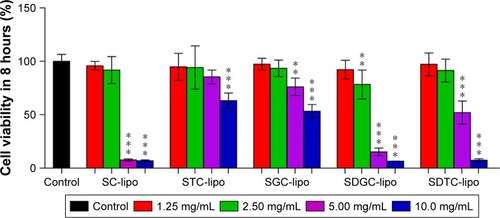
Overall, toxicity and surface activity of bile salts vary according to their structures; thus, all the formulations used in this experiment showed a concentration-dependent increase in cytotoxicity. As no significant toxic effects were observed, liposomes (SC-lipo, STC-lipo, SGC-lipo, SDGC-lipo, or SDTC-lipo) at a concentration of 1.25 mg/mL were used for permeability studies across TR146 cells.
In vitro cell permeation profiles of insulin
The TR146 cell line is a continuous cell line that is derived from human neck node metastasis originating from buccal carcinoma. It is capable of forming stratified nonkeratinized epithelium with four to seven cell layers of flattened cells on the surface after being cultured for 3–4 weeks.Citation4,Citation55 This cellular model has been used to simulate human buccal epithelium to predict the permeations of drug across the epithelium. The TR146 cell culture model closely mimics in vivo conditions; thus, it is used as in vitro model in our experiment.Citation40 TEER is a decisive parameter to evaluate the integrity of the cell layers. In our study, the maximum TEER of confluent TR146 cell layers has reached at Day 30, and the value was 71.68±2.96 Ω·cm2 (97.39% recovery). All of these formulation-treated cells have revealed a recovery of above 96%. There were no any significant changes in the TEER before and after the permeability experiment, and presents the results. This maximum TEER value of confluent TR146 cell layer was consistent with the previous reports.Citation56 Jacobsen et al demonstrated that the maximum integrity of the TR146 cell layers has reached at around Day 30 in culture, and the maximum TEER value was 68.2±2.3 Ω·cm2.Citation56 The in vitro cell culture models that form tight junctions such as Caco-2 cells (260 or 480 Ω·cm2)Citation57,Citation58 and MDCK stain I (1,500 Ω·cm2)Citation59 have a higher magnitude of TEER compared with lacking tight junctions that could be attributed to a lower magnitude of TEER in TR146 cell layers.Citation56 Thus, this proves that the TR146 cell layers maintain the cellular morphology as well as cell monolayer integrity during the experiment.
Table 3 TEER measurements for formulations before and after permeability experiments through TR146 cell layers
The cumulative permeation profiles of insulin-loaded various elastic bilosomes across the TR146 cell layers at each point were plotted as a function of time (). The distinct differences in the cumulative amount of insulin between SDGC-lipo and SC-lipo or SDTC-lipo were observed after 2 hours. The potential of various elastic bilosomes in transporting the insulin across the TR146 cell layers over the period of 8 hours was evaluated by calculating the steady-state flux (Js), a permeability coefficient (Kp), and ER, and presents the results. Improvement in permeation parameters was observed in the order of SDGC-lipo > SC-lipo > SDTC-lipo > SGC-lipo > STC-lipo > insulin solution. The Js, Kp, and ER values of insulin were significantly increased after incorporation into the elastic bilosomes with the most prominent effect found with the SDGC-lipo with an ER of 5.24 (P<0.001). The SC-lipo and SDTC-lipo also led to a significant enhancement with ERs of 3.20 and 3.10 (P<0.05), respectively, compared with insulin solution. This result can be explained as per Lipinski’s Rule of Five, ie, the permeability will increase across the biomembrane, if the number of H-bond donors and the number of H-bond acceptors are <5 and <10, respectively.Citation60–Citation62 Apparently, it means that the lower the value of H-bond donors and H-bond acceptors, the more will be the permeability. The SDGC has lower H-bond donors and acceptors than all the cholic acid derivatives as mentioned in . Thus, the ER was improved in the order of SDGC-lipo > SC-lipo > SDTC-lipo > SGC-lipo > STC-lipo.
Table 4 Permeation parameters calculated from in vitro cell permeation studies
Figure 4 In vitro permeability profiles of insulin-loaded various elastic bilosomes across TR146 cell layers.
Notes: All experiments were conducted from the apical to the basolateral direction in HBSS–HEPES buffer (pH 7.4) at 37°C. Error bars represent SD (n=3).
Abbreviations: HBSS, Hank’s balanced salt solution; HEPES, hydroxyethylpip-erazine ethane sulfonic acid; SC-lipo, sodium cholate-incorporated liposomes; SDGC-lipo, sodium deoxyglycocholate-incorporated liposomes; SDTC-lipo, sodium deoxytaurocholate-incorporated liposomes; SGC-lipo, sodium glycocholate-incorporated liposomes; STC-lipo, sodium taurocholate-incorporated liposomes.
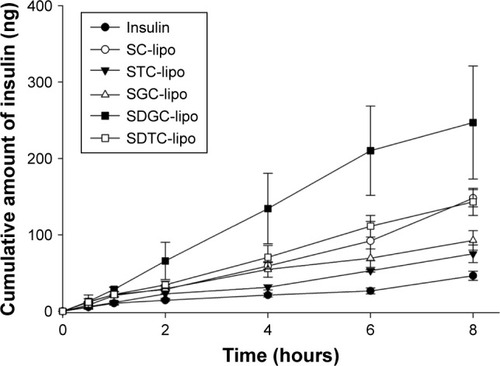
Figure 5 Effect of H-bond donor and acceptor on enhancement profiles.
Abbreviations: ER, enhancement ratio; H, hydrogen; SC-lipo, sodium cholate-incorporated liposomes; SDGC-lipo, sodium deoxyglycocholate-incorporated liposomes; SDTC-lipo, sodium deoxytaurocholate-incorporated liposomes; SGC-lipo, sodium glycocholate-incorporated liposomes; STC-lipo, sodium taurocholate-incorporated liposomes.
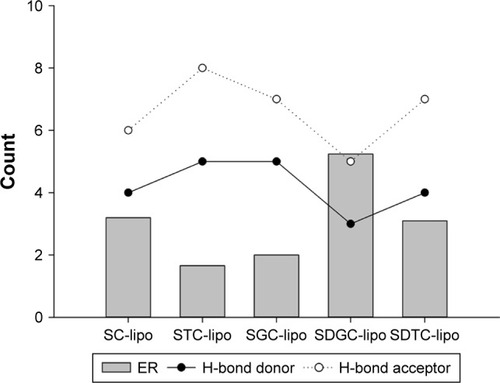
These findings were quite close with the results of relative deformability study (). The higher permeation of SDGC-lipo in comparison with insulin solution could be explained based on their ability to squeeze themselves through the cell pores. The tiny space detention by buccal pore induces a modification in the shape of elastic vesicles and enables them to deliver the entrapped drugs across the buccal mucosa.Citation28 Yang et al have already proposed alternative mechanisms for facilitating insulin transport across the buccal mucosa using SDC-lipo. One mechanism signifies the consequence of transbuccal hydration force across the buccal mucosa induced by the difference in water concentration between its surface and interior as dominant in the transdermal delivery of elastic bilosomes, thus facilitating the penetration of elastic bilosomes into the interstices across the buccal membrane.Citation29 Another mechanism involves fusion of vesicles with the buccal membrane in a manner similar to the process involved in transdermal delivery. Accordingly, vesicles can act as penetration enhancers and penetrate the membrane, modify its intercellular lipids, and increase the membrane’s fluidity and weakness. In addition, the mixing of intercellular lipid layers of membrane and liposome–phospholipid bilayers can play an important role in enhancing the permeation of elastic bilosomes.Citation43,Citation63 It is hypothesized that these factors may be the plausible reasons for the observed enhanced permeation of insulin across TR146 cell layers. In addition, in one study, it has been demonstrated that dihydroxy bile salts (SDGC and SDTC) enhanced the permeation of decitabine than trihydroxy bile salts (SGC and STC) across the porcine buccal mucosa. The enhancement flux was 38-fold higher with 10 mM of SDGC compared with control. It is hypothesized that the enhancement may be due to a complex process including solubilization and micellar entrapment of intercellular lipids, extraction and denaturation of proteins, enzyme inactivation, and swelling of tissues.Citation64 Similarly, our results also showed that permeation enhancement of dihydroxy bile salt-encapsulated liposome (SDGC-lipo, SDTC-lipo) was better compared with trihydroxy bile salt-encapsulated liposomes (SGC-lipo or STC-lipo).
FITC-insulin uptake study in TR146 cell layers
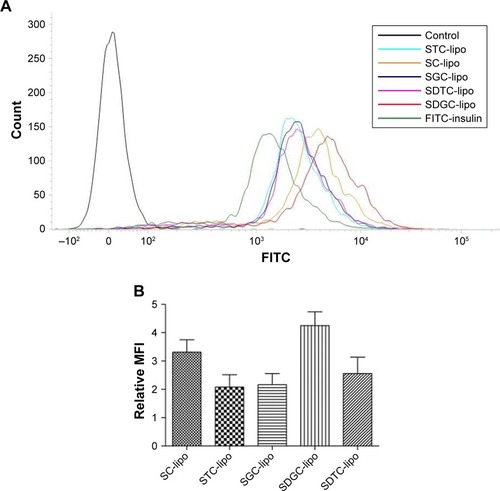
FITC-insulin-loaded liposomes were prepared in order to evaluate the quantitative cellular uptake studies across TR146 cells. FACS analysis was performed for studying the cellular uptake of FITC-insulin-loaded liposomes. presents the representative fluorescence intensity of FITC-insulin-loaded various elastic bilosomes. The graph clearly distinguishes the greater shift in the fluorescence intensity of FITC-insulin after incorporation into various elastic bilosomes. However, there was a little shift in fluorescence intensity after treatment with FITC-insulin alone. In order to compare the obtained fluorescence intensity with the fluorescence intensity of FITC-insulin, the relative MFI values in different treatments were calculated and shown in . The results revealed that SDGC-lipo exhibited a 4.25-fold increase in the cellular uptake of FITC-insulin compared with FITC-insulin alone. A possible explanation for this could be the presence of less number of H-bond donors and acceptors and the nature of dihydroxy bile salt, which contributed toward higher lipophilicity of the system. Similarly, SC-lipo and SDTC-lipo revealed 3.30- and 2.56-fold increases in the cellular uptake of FITC-insulin, respectively. The relative MFI values of elastic bilosomes were counted in the order of SDGC-lipo > SC-lipo > SDTC-lipo > SGC-lipo > STC-lipo, which is in accordance with the results obtained from the drug permeability studies.
Figure 6 Representative fluorescence intensity (A), relative MFI values of FITC-insulin-loaded various elastic bilosomes compared with the relative MFI values of FITC-insulin alone (B).
Note: Error bars represent SD (n=3).
Abbreviations: FITC, fluorescein isothiocyanate; FITC-insulin, FITC-insulin solution; MFI, median fluorescence intensity; SC-lipo, sodium cholate-incorporated liposomes; SDGC-lipo, sodium deoxyglycocholate-incorporated liposomes; SDTC-lipo, sodium deoxytaurocholate-incorporated liposomes; SGC-lipo, sodium glycocholate-incorporated liposomes; STC-lipo, sodium taurocholate-incorporated liposomes.
Interaction of various elastic bilosomes with TR146 cells
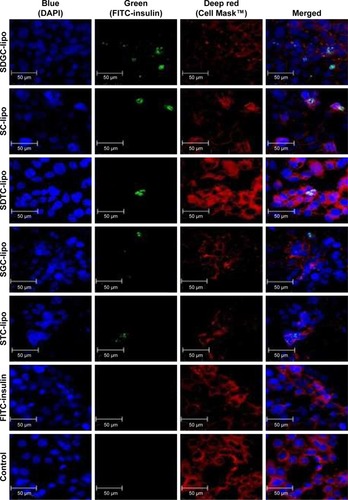
Qualitative cellular uptake was assessed employing confocal microscopy as presented in . The blue fluorescence, green fluorescence, and red fluorescence represent the DAPI that labels the nuclei of cells, the FITC-insulin that indicates FITC-insulin-loaded liposomes, and the Cell Mask™ that labels the cell membranes, respectively. These results demonstrate minimal or no interactions between the cells and various FITC-insulin-loaded elastic bilosomes. In agreement with the FACS results, the cellular uptake of FITC-insulin-loaded SDGC-lipo was potentiated in TR146 cell layers, as presented by the enhancement of green fluorescence emitted by FITC-insulin. The results also showed that FITC-insulin was within or close to the nucleus. Thus, these findings reveal that some amount of insulin was permeated through the transcellular route.Citation3
Figure 7 Confocal images of TR146 cell layers treated with different elastic bilosomes loaded with FITC-insulin after 2 hours of incubation at 37°C.
Notes: Blue: nuclei stained with DAPI; red: cell membrane stained with Cell Mask™; and green: FITC-insulin.
Abbreviations: DAPI, 4′,6-diamidino-2-phenylindole; FITC, fluorescein isothiocyanate; FITC-insulin, FITC-insulin solution; SC-lipo, sodium cholate-incorporated liposomes; SDGC-lipo, sodium deoxyglycocholate-incorporated liposomes; SDTC-lipo, sodium deoxytaurocholate-incorporated liposomes; SGC-lipo, sodium glycocholate-incorporated liposomes; STC-lipo, sodium taurocholate-incorporated liposomes.
Conclusion
Liposomes containing bile salt edge activator (SC, STC, SGC, SDGC, or SDTC) were successfully fabricated using thin-film hydration method and revealed similar particle size and EE. The present study demonstrates that various derivatives of cholic acid-loaded elastic bilosomes can be advantageous for the buccal delivery of insulin. SDGC-lipo was found to be the most superior for the transport of insulin across TR146 cell layers. SC-lipo, SDTC-lipo, SGC-lipo, and STC-lipo were also good candidates for enhancing the insulin permeability across TR146 cells. However, further detailed studies are necessitated to explore the mechanism for the transport of insulin across TR146 cell layers. To conclude, the presented findings present elastic bilosomes as a potential approach for facilitating the buccal delivery of protein/peptide drugs. Another study on in vitro and in vivo application of these elastic bilosomes to porcine buccal tissues and diabetic rabbit models, respectively, is currently under investigation.
Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Sciences, ICT and Future Planning (NRF-2016R1D1A1B01015369).
Disclosure
The authors report no conflicts of interest in this work.
References
- Idf.org [homepage on the Internet]International Diabetes Federation Available from: https://www.idf.org/aboutdiabetes/what-is-diabetes/facts-figures.htmlAccessed January 11, 2018
- Who.int [homepage on the Internet]World Health Organization Available from: http://www.who.int/news-room/fact-sheets/detail/diabetesAccessed January 11, 2018
- IyireAAlaayediMMohammedARPre-formulation and systematic evaluation of amino acid assisted permeability of insulin across in vitro buccal cell layersSci Rep201663249827581177
- XueXYZhouYChenYYPromoting effects of chemical permeation enhancers on insulin permeation across TR146 cell model of buccal epithelium in vitroDrug Chem Toxicol201235219920721848502
- OhDHChunKHJeonSOKangJWLeeSEnhanced transbuccal salmon calcitonin (sCT) delivery: effect of chemical enhancers and electrical assistance on in vitro sCT buccal permeationEur J Pharm Biopharm201179235736321683790
- ShresthaNShahbaziMAAraújoFChitosan-modified porous silicon microparticles for enhanced permeability of insulin across intestinal cell monolayersBiomaterials201435257172717924844163
- BashyalSNohGKeumTChoiYWLeeSCell penetrating peptides as an innovative approach for drug delivery; then, present and the futureJ Pharm Investig2016463205220
- CaonTJinLSimõesCMNortonRSNicolazzoJAEnhancing the buccal mucosal delivery of peptide and protein therapeuticsPharm Res201532112125168518
- PatherSIRathboneMJŞenelSCurrent status and the future of buccal drug delivery systemsExpert Opin Drug Deliv20085553154218491980
- Montenegro-NicoliniMMoralesJOOverview and future potential of buccal mucoadhesive films as drug delivery systems for biologicsAAPS PharmSciTech201718131427084567
- MoralesJOBraydenDJBuccal delivery of small molecules and biologics: of mucoadhesive polymers, films, and nanoparticlesCurr Opin Pharmacol201736222828800417
- BernsteinGDelivery of insulin to the buccal mucosa utilizing the RapidMist systemExpert Opin Drug Deliv2008591047105518754753
- BernsteinGBuccal delivery of insulin: the time is nowDrug Dev Res2006677597599
- OhDHKimMJJeonSOStrategic approaches for enhancement of in vivo transbuccal peptide drug delivery in rabbits using iontophoresis and chemical enhancersPharm Res201532392994025231009
- ShresthaNAraújoFShahbaziMAThiolation and cell-penetrating peptide surface functionalization of porous silicon nanoparticles for oral delivery of insulinAdv Funct Mater2016262034053416
- BashyalSLeeSDelivery of biopharmaceuticals using combination of liposome and iontophoresis: a reviewJ Pharm Investig2015457611624
- CuiMWuWHovgaardLLuYChenDQiJLiposomes containing cholesterol analogues of botanical origin as drug delivery systems to enhance the oral absorption of insulinInt J Pharm20154891–227728425957702
- GuanPLuYQiJEnhanced oral bioavailability of cyclosporine A by liposomes containing a bile saltInt J Nanomedicine2011696597421720508
- LankalapalliSTennetiVSFormulation and evaluation of rifampicin liposomes for buccal drug deliveryCurr Drug Deliv20161371084109926687256
- El-SamaligyMSAfifiNNMahmoudEAIncreasing bioavailability of silymarin using a buccal liposomal delivery system: preparation and experimental design investigationInt J Pharm20063081–214014816356669
- Abd El AzimHNafeeNRamadanAKhalafallahNLiposomal buccal mucoadhesive film for improved delivery and permeation of water-soluble vitaminsInt J Pharm20154881–2788525899288
- MašekJLubasováDLukáčRMulti-layered nanofibrous mucoadhesive films for buccal and sublingual administration of drug-delivery and vaccination nanoparticles – important step towards effective mucosal vaccinesJ Control Release201724918319527469472
- SmistadGJacobsenJSandeSAMultivariate toxicity screening of liposomal formulations on a human buccal cell lineInt J Pharm20073301–2142216997516
- MoghimipourEAmeriAHandaliSAbsorption-enhancing effects of bile saltsMolecules2015208144511447326266402
- HassanNAhadAAliMAliJChemical permeation enhancers for transbuccal drug deliveryExpert Opin Drug Deliv2010719711220017661
- SohiHAhujaAAhmadFJKharRKCritical evaluation of permeation enhancers for oral mucosal drug deliveryDrug Dev Ind Pharm201036325428219663558
- NicolazzoJAReedBLFinninBCBuccal penetration enhancers–how do they really work?J Control Release20051051–211515894393
- ZebAQureshiOSKimHSChaJHKimHSKimJKImproved skin permeation of methotrexate via nanosized ultradeformable liposomesInt J Nanomedicine2016113813382427540293
- YangTZWangXTYanXYZhangQPhospholipid deformable vesicles for buccal delivery of insulinChem Pharm Bull200250674975312045327
- NiuMLuYHovgaardLHypoglycemic activity and oral bioavailability of insulin-loaded liposomes containing bile salts in rats: the effect of cholate type, particle size and administered doseEur J Pharm Biopharm201281226527222369880
- NiuMTanYGuanPEnhanced oral absorption of insulin-loaded liposomes containing bile salts: a mechanistic studyInt J Pharm20144601–211913024275447
- NiuMLuYHovgaardLWuWLiposomes containing glycocholate as potential oral insulin delivery systems: preparation, in vitro characterization, and improved protection against enzymatic degradationInt J Nanomedicine201161155116621822379
- HuSNiuMHuFIntegrity and stability of oral liposomes containing bile salts studied in simulated and ex vivo gastrointestinal mediaInt J Pharm20134411–269370023089580
- MahmudFJeonOCAl-HilalTAAbsorption mechanism of a physical complex of monomeric insulin and deoxycholyl-l-lysyl-methylester in the small intestineMol Pharm20151261911192025892399
- KimSKLeeSJinSDiabetes correction in pancreatectomized canines by orally absorbable insulin-deoxycholate complexMol Pharm20107370871720361761
- LiZZhangMLiuCDevelopment of liposome containing sodium deoxycholate to enhance oral bioavailability of itraconazoleAsian J Pharm Sci2017122157164
- MalakarJSenSONayakAKSenKKFormulation, optimization and evaluation of transferosomal gel for transdermal insulin deliverySaudi Pharm J201220435536323960810
- Al-MahallawiAMAbdelbaryAAAburahmaMHInvestigating the potential of employing bilosomes as a novel vesicular carrier for trans-dermal delivery of tenoxicamInt J Pharm20154851–232934025796122
- DaiYZhouRLiuLLuYQiJWuWLiposomes containing bile salts as novel ocular delivery systems for tacrolimus (FK506): in vitro characterization and improved corneal permeationInt J Nanomedicine201381921193323690687
- SanderCNielsenHMJacobsenJBuccal delivery of metformin: TR146 cell culture model evaluating the use of bioadhesive chitosan discs for drug permeability enhancementInt J Pharm2013458225426124148665
- PorteroARemuñán-LópezCNielsenHMThe potential of chitosan in enhancing peptide and protein absorption across the TR146 cell culture model-an in vitro model of the buccal epitheliumPharm Res200219216917411883644
- KangMJEumJYJeongMSTat peptide-admixed elastic liposomal formulation of hirsutenone for the treatment of atopic dermatitis in NC/Nga miceInt J Nanomedicine201162459246722072881
- El ZaafaranyGMAwadGAHolayelSMMortadaNDRole of edge activators and surface charge in developing ultradeformable vesicles with enhanced skin deliveryInt J Pharm20103971–216417220599487
- JainSJainPUmamaheshwariRBJainNKTransfersomes – a novel vesicular carrier for enhanced transdermal delivery: development, characterization, and performance evaluationDrug Dev Ind Pharm20032991013102614606665
- El MaghrabyGMWilliamsACBarryBWOestradiol skin delivery from ultradeformable liposomes: refinement of surfactant concentrationInt J Pharm20001961637410675708
- LeeEHKimAOhYKKimCKEffect of edge activators on the formation and transfection efficiency of ultradeformable liposomesBiomaterials200526220521015207467
- CevcGGebauerDStieberJSchätzleinABlumeGUltraflexible vesicles, transfersomes, have an extremely low pore penetration resistance and transport therapeutic amounts of insulin across the intact mammalian skinBiochim Biophys Acta1998136822012159459598
- KangMJEumJYJeongMSFacilitated skin permeation of oregonin by elastic liposomal formulations and suppression of atopic dermatitis in NC/Nga miceBiol Pharm Bull201033110010620045944
- KarnPRJinSELeeBJPreparation and evaluation of cyclosporin A-containing proliposomes: a comparison of the supercritical antisolvent process with the conventional film methodInt J Nanomedicine201495079509125395846
- YangLZhangHFawcettJPMikovMTuckerIGEffect of bile salts on the transport of morphine-6-glucuronide in rat brain endothelial cellsJ Pharm Sci201110041516152424081474
- LeeVHLYamamotoAPenetration and enzymatic barriers to peptide and protein absorptionAdv Drug Deliv Rev198942171207
- DuchateauGSMJEZuidemaJMerkusFWHMBile salts and intra-nasal drug absorptionInt J Pharm1986313193199
- MorimotoKUeharaYIwanagaKInfluence of absorption enhancers (bile salts) and the preservative (benzalkonium chloride) on mucociliary function and permeation barrier function in rabbit tracheasEur J Pharm Sci1998632252309795068
- GordonGSMosesACSilverRDFlierJSCareyMCNasal absorption of insulin: enhancement by hydrophobic bile saltsProc Natl Acad Sci U S A19858221741974233903753
- ShresthaNAraújoFSarmentoBHirvonenJSantosHACell-based in vitro models for buccal permeability studiesSarmentoBrunoConcepts and Models for Drug Permeability StudiesNew YorkElsevier20153140
- JacobsenJvan DeursBPedersenMRassingMRTR146 cells grown on filters as a model for human buccal epithelium: I. Morphology, growth, barrier properties, and permeabilityInt J Pharm19951252165184
- AnderbergEKNyströmCArturssonPEpithelial transport of drugs in cell culture. VII: Effects of pharmaceutical surfactant excipients and bile acids on transepithelial permeability in monolayers of human intestinal epithelial (Caco-2) cellsJ Pharm Sci19928198798871432633
- ArturssonPEpithelial transport of drugs in cell culture. I: A model for studying the passive diffusion of drugs over intestinal absorptive (Caco-2) cellsJ Pharm Sci19907964764821975619
- ChoMJThompsonDPCramerCTVidmarTJScieszkaJFThe Madin Darby canine kidney (MDCK) epithelial cell monolayer as a model cellular transport barrierPharm Res19896171772470075
- AlexAMillanDSPerezMWakenhutFWhitlockGAIntramolecular hydrogen bonding to improve membrane permeability and absorption in beyond rule of five chemical spaceMed Chem Comm201127669674
- ChoyYBPrausnitzMRThe rule of five for non-oral routes of drug delivery: ophthalmic, inhalation and transdermalPharm Res201128594394820967491
- BhalSKKassamKPeirsonIGPearlGMThe Rule of Five revisited: applying log D in place of log P in drug-likeness filtersMol Pharm20074455656017530776
- VermaDDVermaSBlumeGFahrALiposomes increase skin penetration of entrapped and non-entrapped hydrophilic substances into human skin: a skin penetration and confocal laser scanning microscopy studyEur J Pharm Biopharm200355327127712754000
- MahalingamRRavivarapuHRedkarSLiXJastiBRTransbuccal delivery of 5-Aza-2′-deoxycytidine: effects of drug concentration, buffer solution, and bile salts on permeationAAPS PharmSciTech200783E28E33
