Abstract
This preliminary study investigated the use of poly (2-hydroxyethyl methacrylate) (pHEMA) nanoparticles for the delivery of the deoxyribonucleic acid (DNA) vaccine pCAG-HAk, which expresses the full length hemagglutinin (HA) gene of the avian influenza A/Eurasian coot/Western Australian/2727/1979 (H6N2) virus with a Kozak sequence which is in the form of a pCAGGS vector. The loaded and unloaded nanoparticles were characterized using field-emission scanning electron microscopy. Further characterizations of the nanoparticles were made using atomic force microscopy and dynamic light scattering, which was used to investigate particle size distributions. This preliminary study suggests that using 100 μg of pHEMA nanoparticles as a nanocarrier/adjuvant produced a reduction in virus shedding and improved the immune response to the DNA vaccine pCAG-HAk.
Introduction
Nanotechnology has been able to deliver a wide range of new and novel materials. These new nanomaterials are increasingly becoming the subject of many investigations in several fields, particularly those of engineering, biotechnology, and biomedical sciences.Citation1,Citation2 Nanomaterials can be made from a wide range of solid materials such as metals, ceramics, polymers, organic materials, and composites. They can come in a wide range of morphologies; namely, spheres, rods, tubes, and plates. The use of nanoparticles of biodegradable polymers is being extensively studied since they provide an attractive alternative for a number of nanomedical applications by providing a delivery platform for the sustained, controlled, and targeted release of drugs and immunogens. These immunogens, therapeutic drug agents, or in some cases imaging agents can be loaded into a biodegradable polymer matrix. Once the polymer is administered, the nanoparticles of the matrix slowly begin to degrade and release the drug or immunogen agents. In addition, the biodegradable nanoparticles can be administered through several different delivery routes, such as oral, nasal, ocular, transdermal, and intravenous routes.Citation3 Ideally these nanoparticles should be inert, biocompatible, and biodegradable. They also need to be stable in vivo, easily attached to immunogens, effectively delivered, and have little or no side effects.Citation4–Citation6
The 1918 Spanish flu is considered to be the deadliest disaster in human history. The flu killed more than 50 million people worldwide and was related to an avian flu virus H1N1.Citation7 In the late 1990s, the re-emergence of avian influenza demonstrated that this type of virus is persistent and can reach endemic levels in many south-east Asian countries if not effectively managed. Influenza still remains an important and threatening disease to both humans and animals. In contrast to measles, smallpox, and poliomyelitis, influenza is caused by viruses that undergo a continuous antigenic modification within their natural host. The natural reservoir for these viruses is aquatic, migratory birds, which usually flock in large numbers and travel great distances between countries. When these birds associate with the local terrestrial poultry they can occasionally transmit transitory infections. The diversity of diseases that can be transmitted range from mild respiratory illnesses to fatal systematic diseases. The development of new antiviral drugs and vaccines based on nanoparticles has the potential to provide an effective method in dealing with any possible future outbreaks of the influenza virus strains.
Polymer based nanoparticles have been found to improve the therapeutic efficacy and reduce the potential side effects of many therapeutic drug agents. The major challenge facing nanomedicine today in using these polymeric delivery systems is to engineer and manufacture a biodegradable nanoparticle matrix with the desired physiochemical and pharmaceutical properties. If these optimum properties are achieved, then delivering the payload should permit the controlled release of medication concentration within the effective therapeutic window and dosage.Citation3 The polymeric nanoparticle matrix used in any particular application is an important factor because it can influence parameters such as protein loading, stability, biodegradability, and bioavailability. Citation8 Thus there are a number of commercially available biodegradable polymers currently used in polymeric nanoparticle matrix formulations. For example, the most widely researched Food and Drug Administration (FDA)-approved biodegradable polymers in the literature are poly (lactide) (PLA), poly (D,L-lactide-co-glycolide) (PLGA) (a copolymer of PLA and poly (glycolide) [PGA]), and poly (ɛ-caprolactone) (PCL).Citation9
The polymers PLA, PLGA, PGA, and PCL were all originally synthesized in the 1950s for nondrug delivery functions such as surgical sutures, textile grafts, and implants. Since this time, these polymers have been also investigated for a variety of drug agent delivery platforms in a number of therapeutic applications. Unfortunately, there are a number of disadvantages in using these polymers; for example, their strong mechanical strength and slow degradation rates, which can lead to a slow drug release that does not provide the desired concentration. In addition, the bioactivity of proteins and peptides encapsulated in the polymer matrix can deteriorate since the polymers’ hydrophobic nature can produce an acidic microenvironment. This microenvironment results from water being unable to enter the matrix and the accumulation of acidic breakdown products (lactic and glycolic acid end groups). There are also issues with the hydrophobic nature of the polymeric nanoparticles interacting with hydrophilic molecular probes used for targeting, which can lead to complications in the drug preparation technology.Citation8 It is due to these disadvantages that many researchers look for other novel biodegradable polymers and copolymer delivery platform systems for immunogens and therapeutic drugs.
Many synthetic methods have been used to manufacture a variety of nanopolymeric particles with various sizes and morphologies. The latter parameters having a dominant bearing on the final properties of the nanomaterial synthesized. Some of the attractive features of using a synthetic sonochemical approach are: less complications, reduced processing time, generally more efficient, and economical.Citation10–Citation13 The sonochemical technique is based on the acoustic cavitation phenomenon, which produces the continuous formation, growth, and final implosive collapse of bubbles in the solution being sonicated. This creates numerous hot-spots in the solution, which provide sufficient energy for the formation and growth of nanoparticles. This synthetic process can be extended to polymers and composite materials.Citation14,Citation15
In this article, the development of biocompatible and biodegradable nanosized poly (2-hydroxyethyl methacrylate) (pHEMA) particles that are used as deoxyribonucleic acid (DNA) vaccine carriers is described. DNA vaccination is an effective procedure for inducing protective immunity against a number of infectious and noninfectious diseases in a variety of animals.Citation16 However, several factors can influence their performance; for example, the delivery technique will dictate the DNA dosage level that is required to solicit an effective immune response. In addition, the rapid degradation and low cellular uptake of plasmid DNA can also have a dramatic effect on the efficiency of the exposed plasmid DNA vaccines.Citation17 To remediate these problems, plasmid DNA vaccines have been combined with particles, via adsorption, or encapsulation, or by co-formulation to stabilize the plasmid DNA delivery. Combining plasmid DNA with particles significantly reduces the degradation process and also stabilizes the vaccine. It also has the advantage of providing particular materials that are effectively taken up by the antigen presenting cells, thus providing an adjuvant (synergistic) effect. Historically, adjuvants have been successfully used in the development of vaccines.Citation18 Conventional chemical adjuvants such as bupivacaineCitation19 or Marcaine® (Hospira, Inc, Lake Forest, IL), ubenimex,Citation20 monophosphoryl lipid A,Citation21 QS-21 saponin,Citation22 and levamisoleCitation23 have been investigated successfully. These adjuvants were able to facilitate a positive immune response to the DNA vaccines being tested.
The discovery in 1995 of injecting solid inert beads with DNA-encoded antigens resulted in the priming of CD8T cells for a direct immune response.Citation24 Since then, inert nanoparticles have also been able to induce strong immune responses to protein and peptide antigens in mice,Citation25,Citation26 sheep,Citation18 pigs,Citation27 and cattle.Citation27 In addition, both metals and inorganic nanomaterials have been used in similar biomedical applications. For example, a metal such as gold which is nontoxic, inert, and stable within the body environment has been used as a contrast agent in cancer diagnosis and photodermal cancer therapy. It has also been effectively used as a delivery platform for oligonucleotide, insulin, and genes.Citation28 Metal oxide NPs such as magnetite (Fe3O4) have been used as magnetically targeted drug delivery platforms due to their biodegradability and biocompatibility. Once these NPs are introduced into the blood stream, the particles flow to the specific location of interest in the body where a strong magnetic field can be used to pull them out of suspension and deliver the pharmaceutical payload.Citation29 Furthermore, an inorganic material such as mesoporous silica, with its controllable structural properties and biocompatibility, has been effectively used to deliver calcein.Citation30
In the case of DNA vaccines, cationic nanoparticles have been formulated with plasmid DNA encoding of a reporter gene. This vaccine was able to enhance the in-vitro cell transfection efficiency and achieve a substantial cellular immune response (16–200 times greater than the normal plasmid DNA by itself) in mice cells via a number of delivery routes.Citation4,Citation31–Citation33 Furthermore, it has also been shown that when both the cholera toxin and lipid A were administered with a nanoparticle-based plasmid DNA, there was an overall synergistic effect which enhanced the immune response of the cellular tissues.Citation5,Citation33 Thus, nanoparticles can also be seen as a novel class of adjuvants, with the potential to be effective delivery platforms for proteins and plasmid DNA immunogens, which can successfully induce a positive immune response. In addition, the nanoparticle delivery platform distributes its payload without the usual side effects associated with local tissue damage caused by conventional chemical adjuvants.
In the past, polymeric particles, both synthetic and natural, have been investigated as potential carriers for the delivery of plasmid DNA to provide cellular immunity. These particles have been found to provide suitable accommodation to plasmids of varying sizes and to provide protection to the plasmid DNA payload from the in-vivo effects of extracellular degradation. In addition, these particles have also provided an enhanced response from the immune system. The first polymeric particle delivery system used for delivering DNA used microsized particles of poly (lactideco-glycolide).Citation34 Recently, polymeric nanoparticles have been investigated for possible plasmid DNA vaccine carriers. The most attractive features of using nanosized polymeric delivery systems are: the nanostructure provides an effective scaffold which is capable of providing a controlled release of DNA, polymeric nanoparticles can easily be manufactured, and they are biocompatible and biodegradable.Citation35,Citation36 Recently, a polymeric microparticle study of formulated plasmid DNA encoding of the nucleoprotein gene A/PR/8/34 of the (H1N1) virus revealed an enhanced immune response in miceCitation37 and a biodegradable pHEMA has also been used in a similar drug delivery system.Citation38,Citation39 However, to date there has been no reports of a nanoparticle pHEMA-based avian influenza DNA vaccine for the H6N2 virus. The present study investigated the immunologic effect of a novel polymeric nanomaterial, pHEMA, as a potential plasmid DNA nanocarrier for a vaccine against the wild bird (H6N2) avian influenza virus. A major advantage of using pHEMA as the vaccine carrier is that this particular nontoxic copolymer has FDA approval for use in contact lenses, implant coatings, and prostheses.
Material and methods
Chemicals
All chemicals were purchased from Sigma-Aldrich (Castle Hill, NSW, Australia) and used without further purification. Milli-Q® water (18.3 MΩ cm−1) was used throughout all synthesis procedures involving aqueous solutions. The surfactant used in the preparation of the pHEMA nanoparticles was poly (vinyl alcohol) (PVA) and was prepared by dissolving 1 g of PVA in a 100 mL solution of Milli-Q® water. Throughout the preparation of the nanoparticles, a 1% w/v of PVA was used.
Formulation and optimization of solvent
The optimization of the solvent used for mixing pHEMA and DNA, and the calculation of DNA binding, was determined from a comparative study. The study looked at dissolving 1 g of pHEMA in various solutions where the percentage w/v of an alcohol (ethanol) in a Milli-Q water solution was adjusted. In the first case, a 100 mL solution of pure Milli-Q water was used; the second solution consisted of a mixture composed of 50 mL of Milli-Q water and 50 mL of ethanol; the third solution consisted of a mixture composed of 25 mL of Milli-Q water and 75 mL of ethanol; and the final solution consisted of 100 mL of ethanol. All polymer solvent solutions prepared contained 1% w/v of pHEMA. During the preparation of all loaded and unloaded nanoparticle preparations, 2 mL of pHEMA (1% w/v) was used.
Preparation of pHEMA nanoparticles
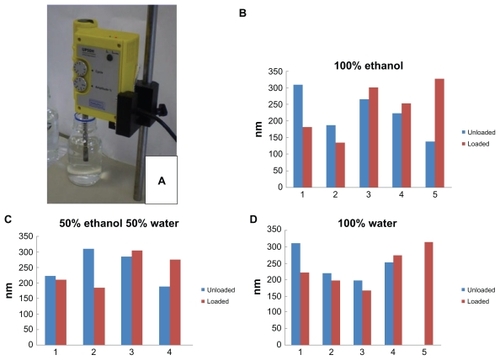
The preparation of the unloaded pHEMA nanoparticles started by adding a 2 mL solution of pHEMA (1% w/v) to a 10 mL glass tube supported in an ice bath. The pHEMA was then exposed to ultrasonic irradiation for 30 seconds before 1 mL of PVA (1% w/v) was added to the glass tube dropwise and then sonicated for a further 10 minutes. The ultrasonic processor used throughout these procedures was a UP50H (50 W, 30 kHz, MS7 Sonotrode (7 mm diameter, 80 mm length)) supplied by Hielscher Ultrasound Technology (see ).
Preparation of plasmid DNA vaccine with pHEMA
The formulation of the pHEMA nanoparticles and the DNA composite begins with a 4 mL solution of pHEMA (1% w/v in 100% ethanol blend) being added to a 10 mL glass tube supported in an ice bath. The solution was then sonicated for 30 seconds before a 2 mL solution (1% w/v) of PVA was added dropwise to the glass tube, which was then sonicated for a further 2 minutes. This was followed by the dropwise addition of 400 μL of plasmid DNA (9.3 μg/μL) to the glass tube and then sonicated for a further 10 minutes. At the end of this time, the solution was filtered three times through a 0.2 μm membrane to remove the surfactant. The filtered solution was then centrifuged at 15,000× g for 20 minutes at room temperature. The resultant pellet was then dissolved in phosphate buffered saline (PBS), and the amount of plasmid DNA coated nanoparticles was calculated by subtracting the amount of DNA in the supernatant from the total DNA added. The DNA concentration in the supernatant was measured by a nanodrop ND-1000 Spectrophotometer (Thermo Scientific, Waltham, MA).
Characterization of pHEMA nanoparticles
The structural and morphological features of the dispersed pHEMA nanoparticles were investigated using field-emission scanning electron microscopy (FESEM). Samples were dropped onto a conventional SEM stub and the latter coated with Au. All FESEM scans were taken using a high resolution Zeiss 1555 Variable Pressure Field Emission at 3 kV with a 30 μm aperture under 1 × 10−10 Torr pressure. Atomic force microscopy (AFM) imaging of the pHEMA nanoparticles was carried out by first dropping a few drops of an ethanol solution containing the nanoparticles onto a freshly cleaved mica substrate and then allowing the solution to evaporate before imaging the dry substrate using a Pico-Plus AFM operating in Tapping Mode (molecular imaging). The probes used during the scanning mode were silicon tips with a spring constant of 42 N/m and a resonant frequency of 300 kHz. The dynamic light scattering (DLS) technique was used to investigate the pHEMA nanoparticle sizes. The loaded and unloaded pHEMA nanoparticles were dispersed in ethanol prior to being investigated by the DLS. The detector used was a Malvern Zetasizer 3000 HAS (Malvern Instruments, Ltd, Worcestershire, UK) (633 nm) operated at 25°C.
Antibody response in animal (chicken) model
For Australian biosecurity reasons, a low pathogenic avian influenza virus, A/Eurasian coot/Western Australia/2727/1979 (H6N2), isolated from a healthy Eurasian coot (Fulica atra) in Australia, was selected to perform this DNA vaccine adjuvant study. The procedure of combining the pCAG-HAk plasmid DNA that expresses the complete hemagglutinin (HA) gene of the avian influenza virus (H6N2), together with a Kozak sequence, in a pCAGGS vector used in the DNA vaccine has been previously described by Shan et al.Citation40
Vaccination regime
All bird experiments were carried out with the approval of Murdoch University’s animal ethics committee, and all experiments were conducted in accordance with the Australian National Health and Medical Research Council’s (NHMRC) code of practice for the care and use of animals for scientific purposes. The birds selected for this study were 3-week-old Hy-Line chickens that were free from the avian influenza. The chickens were accommodated in free-range pens with access to feed and water, and were maintained at the Animal Resource Centre, Murdoch University, Perth, Western Australia.
The experimental immunization protocol used in the bird vaccine study is presented in and contains information regarding bird numbers and vaccine dosage. During the protocol, each bird received two intramuscular injections of 0.2 mL at 3-week intervals. The injection procedure involved a 0.1 mL dose being injected in each leg. Over this period, the six control birds received a 200 μL dose of PBS without adjuvant, five birds received a 100 μL dose of pCAG-HAk without adjuvant, and the remaining sets of birds received doses of 10 μL, 100 μL, and 200 μL of pCAG-HAk with pHEMA. Sera samples were collected weekly to detect and monitor the H6 specific antibody of hemagglutination-inhibition (HI).Citation40,Citation41 Three weeks after the booster vaccination, each bird received a 0.5 mL dose of the wild bird H6N2 avian influenza virus (106.5 EID50/0.1 mL) via three delivery routes. In the first route, the bird received 0.1 mL of the H6N2 virus by nasal instillation, the second 0.1 mL was introduced via eye drops, and the final 0.3 mL dose was delivered through an oral route. Following the virus challenge, a daily observation of all birds was undertaken and either oropharyngeal or cloacal swabs were collected every second day over a 7-day period. The virus isolation procedure was performed in accordance with the manual of diagnostic tests and vaccines for terrestrial animals.Citation41
Table 1 Immunization protocol in chicken vaccine study
Results and discussion
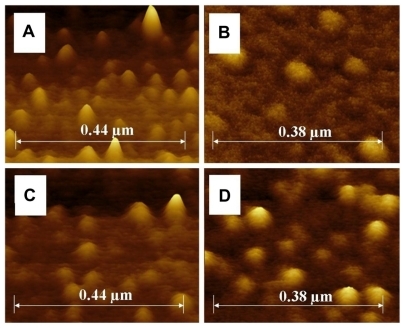
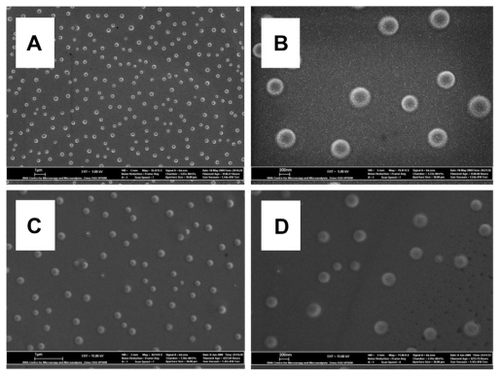
Optimization of the solvent revealed that the pHEMA nanoparticles prepared with 100% ethanol produced the highest DNA binding rate. The total plasmid DNA used in each solvent experiment was 581.3 ng/μL, and the maximum DNA binding rate was found in 100% ethanol solution, with only 28.3 ng/μL of DNA remaining in the supernatant (see ). Thereafter, 100% ethanol was used for the preparation of the pHEMA adjuvant vaccine for the rest of the study. In the 100% water case, the unloaded particles of pHEMA ranged in size from 168 to 314 nm, with the unloaded particles being larger in most cases. In the 50% ethanol and 50% water case, the pHEMA particles ranged in size from 185 to 311 nm, with the unloaded particles being larger in half of the trials. While in the 100% ethanol case, the pHEMA particles ranged from 136 to 328 nm, with the unloaded particles being smaller in more than half of the trials (see ). presents FESEM images of the unloaded and DNA-loaded pHEMA nanoparticles; the images reveal that the nanoparticles range in size from 120 to 330 nm and have spherical morphology. This is confirmed by the AFM profile images of the unloaded and loaded pHEMA nanoparticles presented in . The DLS, FESEM, and AFM analysis all confirm that the nanoparticles range in size from 120 to 330 nm; the morphology is spherical in the unloaded system and appears to be unchanged by the incorporation of the DNA.
Table 2 The effect of solvent composition on plasmid DNA binding to pHEMA
Figure 2 Field-emission scanning electron microscopy images of the unloaded and DNA-loaded pHEMA nanoparticles with the spherical particle morphology. (A) Unloaded pHEMA nanoparticles at low magnification (scale bar 1 μm) and (B) at high magnification (scale bar 200 nm); and (C) DNA-loaded pHEMA nanoparticles at low magnification (scale bar 1 μm) and (D) at high magnification (scale bar 200 nm).
Figure 3 Atomic force microscopy profile images of the unloaded and DNA-loaded pHEMA nanoparticles with spherical particle morphology. (A) Unloaded pHEMA nanoparticles at low magnification and (B) at high magnification; and (C) DNA-loaded nanoparticles of pHEMA at low magnification and (D) at a higher magnification.
Abbreviations: DNA, deoxyribonucleic acid; pHEMA, poly (2-hydroxyethyl methacrylate).
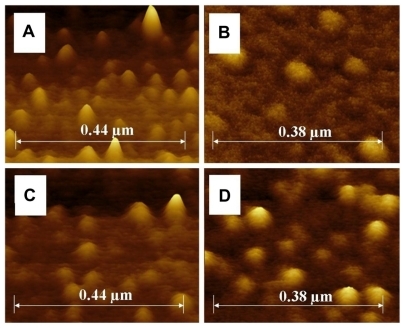
Abbreviations: DNA, deoxyribonucleic acid; pHEMA, poly (2-hydroxyethyl methacrylate).
Following DNA loading procedures, the efficiency of the nanovaccine was tested in a bird (Hy-Line chicken) model. Three weeks post second vaccination, no H6 HI antibody titer was detected in any of the Hy-Line chickens. At the end of 10 days post virus challenge, all birds sero-converted with a range of HI titers, which are presented in . There was a significant difference (P < 0.05) in the geometric mean titer of the HI antibody prior to and post virus challenge using the paired-sample t-test.
Table 3 Antibody response prior to and post virus challenge
presents the level of virus shedding in both the oropharyngeal and cloacal swabs in vaccinated birds following the H6N2 avian influenza virus challenge. Comparing the pCAG-HAk vaccinated group with the naive control group, we can see that the virus excretion rate in the oropharyngeal swabs of 70.8% in the naive group was reduced to 45% in the pCAG-HAk group following the virus challenge. While cloacal swabs for the naive control group recorded a 12.5% value, the pCAG-HAk vaccinated group was reduced to 0% value for the post virus challenge.
Table 4 Virus shedding level in chickens vaccinated with plasmid pCAG-HAk and pHEMA adjuvants following the virus challenge
reveals that there is a significant difference between the pCAG-HAk vaccinated group and the naive control group for both oropharyngeal and cloacal swabs. In comparison with the naive control group, the 100 μg pHEMA adjuvanted plasmid pCAG-HAk group has shown a significant decrease in virus shedding in both oropharyngeal and cloacal swabs. This result suggests that using pHEMA as an adjuvant has improved the immune response to the DNA vaccine pCAG-HAk. It is suspected that a major factor that contributed to the improved immune response produced by the pHEMA lies in its hydrophilic nature and its positive surface charge that was conveyed from the ethanol solvent. This positive surface charge significantly improves the absorption of plasmid DNA than the water solvent, see . The plasmid DNA is believed to be absorbed onto the surface of pHEMA nanoparticles through an electrostatic interaction or by covalent binding. Importantly, this bonding mechanism did not appear to damage the plasmid DNA’s immunization performance. In addition, the bonding mechanism appears to be complex because the optimum effect occurred in the bird group that received the 100 μg dose. Both the 10 and 200 μg dose groups were less effective. The mechanisms behind the observed adjuvant effect have not yet been resolved. Some possible mechanisms that could have affected the performance of the pHEMA nanoparticle delivery platform include: the surface distribution of the plasmid DNA on the nanoparticles, the delivery platform prevented effective DNA degradation, which in turn affected the targeting of the DNA to antigen presenting cells.Citation34,Citation42 Another factor that needs to be investigated further is the effect of the nanoparticle size used in the delivery platform. In this study, the pHEMA nanoparticle size ranged from 120 to 330 nm, and this size range could have influenced the delivery mechanism. Recent studies have shown that the size of the nanoparticles being used as the DNA delivery platforms can have a significant effect on the DNA vaccine efficacy.Citation5,Citation18,Citation25,Citation43
The use of particular delivery platforms as a novel method of delivering a payload of proteins and/or plasmid DNA immunogens to induce a positive immune response is a research area that is currently receiving a great deal of interest. The characteristics of both micro- and nanosized particles can have a significant impact on the overall performance of the delivery system. For example, the size, shape, and surface properties such as hydrophobicity and surface charge directly affect the efficiency of the particular delivery system.Citation44 Recently, a variety of inert nanoparticles was investigated and found to be effective delivery vehicles for protein and peptide antigens.Citation4,Citation28–Citation30,Citation39,Citation45,Citation46 However, the application of nanoparticles as delivery platforms with DNA vaccines as payloads is only at the exploratory stage.Citation33,Citation43 In this present preliminary study, the potential application of using a biodegradable, nontoxic copolymer (pHEMA nanoparticles) as a delivery platform to carry pCAG-HAk plasmid DNA has been investigated. In the past, pHEMA has been used in drug delivery systems;Citation26,Citation31 however, to date, it appears that this study is the first to use pHEMA nanoparticles as an adjuvant in DNA vaccination.
Conclusion
This preliminary study suggests that using pHEMA nanoparticles as a nanocarrier/adjuvant have improved the immune response to the DNA vaccine pCAG-HAk. A reduction in virus shedding was detected in both oropharyngeal and cloacal swabs for the 100 μg pHEMA adjuvant DNA vaccine. Three pHEMA adjuvant doses (10, 100, and 200 μg) were investigated. The study revealed that there was a dose response effect, with the 100 μg producing the most significant amount of virus shedding. The mechanism behind this adjuvant effect has not been resolved, but the reduction of virus shedding in the oropharynx of chickens challenged with the wild bird H6N2 influenza virus warrants further investigation.
Acknowledgments
The authors would like to thank Dr Zhong-Tao Jiang for his helpful discussions. Ms Jennifer Millar is also acknowledged for her assistance. Dr Derek Fawcett would like to thank the Bill and Melinda Gates Foundation for his research fellowship.
Disclosure
The authors report no conflict of interest in this work.
References
- RamakrishnaSRamalingamMSampath KumarTSSoboyejoWOBiomaterials: a nano approach1st edBoca Raton, FLCRC Press2010
- GrecoRSPrinzFBSmithRLNanoscale Technology in Biological Systems1st edBoca Raton, FLCRC Press2005
- FengSSNew concept chemotherapy by nanoparticles of biodegradable polymers: where are we now?Nanomedicine20061329730917716160
- CuiZMumperRJGenetic immunization using nanoparticles engineered from micro-emulsion precursorsPharm Res20021993994612180545
- WangRDoolanDLLeTPHedstromRCCoonanKMInduction of antigen-specific cytotoxic T lymphocytes; in humans by a malaria DNA vaccineScience19982824764809774275
- ScheerlinckJPGreenwoodDLParticulate delivery systems for animal vaccinesMethods20064011812416997719
- PattersonKDPyleGFThe geography and mortality of the 1918 influenza pandemicBull Hist Med Spring19916514212021692
- LeeMIruela ArispeMIWuBMDunnJCYModulation of protein delivery from modular polymer scaffoldsBiomaterials200728101862187017184836
- ZhangZFengSSIn vitro investigation on poly (lactide) Tween 80 copolymer nanoparticles by dialysis method for chemotherapyBiomacromolecules200671139114616602731
- SuslickKSFangMMHyeonTNanostructured materials generated by high intensity ultrasound: sonochemical synthesis and catalytic studiesJ Am Chem Soc199611821722179
- BangJHSuslickKSApplications of ultrasound to the synthesis of nanostructured materialsAdv Mater2010221039105920401929
- GengJLiuBXuLHuFNZhuJJFacile route to Zn based II–VI semiconductor spheres, hollow spheres and core/shell nanocrystals and their optical propertiesLangmuir20072320102861029317718525
- PoinernGEJBrundavanamaRKMondinosaNJiangZTSynthesis and characterisation of nanohydroxyapatite using an ultrasound assisted methodUltrason Sonochem200916446947419232507
- ZhangKParkBJFangFFChoiHJSonochemical preparation of polymer nanocompositesMolecules2009142095211019553883
- FreitasSHielscherGMerkleHPGanderBA fast and simple method for producing biodegradable nanospheresEur Cell Mater2004722829
- AbdulhaqqSAWeinerDBDNA vaccines: developing new strategies to enhance immune responsesImmunol Res20084221923219066740
- WilsonKDde JongSDKazemMThe combination of stabilized plasmid lipid particles and lipid nanoparticle encapsulated CpG containing oligodeoxynucleotides as a systemic genetic vaccineJ Gene Med200911142519003796
- ScheerlinckJPGlosterSGamvrellisAMottramPLPlebanskiMSystemic immune responses in sheep, induced by a novel nano-bead adjuvantVaccine2006241124113116202487
- WangBUgenKESrikantanVGene inoculation generates immune responses against human immunodeficiency virus type 1Proc Natl Acad Sci U S A199390415641608483929
- SasakiSFukushimaJHamajimaKAdjuvant effect of Ubenimex on a DNA vaccine for HIV-1Clin Exp Immunol199811130359472658
- SasakiSHamajimaKFukushimaJComparison of intranasal and intramuscular immunization against human immunodeficiency virus type 1 with a DNA-monophosphoryl lipid A adjuvant vaccineInfect Immun1998668238269453648
- SasakiSSuminoKHamajimaKInduction of systemic and mucosal immune responses to human immunodeficiency virus type 1 by a DNA vaccine formulated with QS-21 saponin adjuvant via intramuscular and intranasal routesJ Virol199872493149399573261
- JinHLiYMaZEffect of chemical adjuvants on DNA vaccinationVaccine2004222925293515246629
- FaloLDKovacsovics-BankowskiMThompsonKRockKLTargeting antigen into the phagocytic pathway in vivo induces protective tumour immunityNat Med199516496537585145
- FifisTGamvrellisACrimeen-IrwinBSize-dependent immunogenicity: therapeutic and protective properties of nano-vaccines against tumoursJ Immunol20041733148315415322175
- FifisTMottramPBogdanoskaVHanleyJPlebanskiMShort peptide sequences containing MHC class I and/or class II epitopes linked to nano-beads induce strong immunity and inhibition of growth of antigen-specific tumour challenge in miceVaccine20042325826615531045
- AucouturierJDupuisLGanneVAdjuvants designed for veterinary and human vaccinesVaccine2001192666267211257407
- MishaBPatelBBTiwariSColloidal nanocarriers: a review on formulation technology, types and applications towards targeted drug deliveryNanomedicine2010692419447208
- PankhurstQAConnollyJJonesSKDobsonJApplications of magnetic nanoparticles in biomedicineJ Phys D Appl Phys200316167181
- SlowingIIVivero-EscotoJLWuCLinVSMesoporous silica nanoparticles as controlled release drug delivery and gene transfection carriersAdv Drug Deliv Rev2008601278128818514969
- CuiZMumperRJIntranasal administration of plasmid DNA-coated nanoparticles results in enhanced immune responsesJ Pharm Pharmacol2002541195120312356273
- CuiZMumperRJTopical immunization using nanoengineered genetic vaccinesJ Control Release20028117318411992690
- CuiZMumperRJThe effect of co-administration of adjuvants with a nanoparticle-based genetic vaccine delivery system on the resulting immune responsesEur J Pharm Biopharm200355111812551699
- SinghMBrionesMOttGO’HaganDCationic microparticles: a potent delivery system for DNA vaccinesProc Natl Acad Sci U S A20009781181610639162
- NguyenDNGreenJJChanJMLangerRAndersonDGPolymeric materials for gene delivery and DNA vaccinationAdv Mater200921847867
- Galindo-RodriguezSAAllemannEFessiHDoelkerEPolymeric nanoparticles for oral delivery of drugs and vaccines: a critical evaluation of in vivo studiesCrit Rev Ther Drug Carrier Syst20052241946416313233
- HartikkaJGeallABozoukovaVPhysical characterization and in vivo evaluation of poloxamer-based DNA vaccine formulationsJ Gene Med20081077078218425981
- PiotrowiczAShoichetMSNerve guidance channels as drug delivery vehiclesBiomaterials2006272018202716239029
- RaoKPNew concepts in controlled drug deliveryPure Appl Chem19987012831287
- ShanSHJiangYPBuZGStrategies for improving the efficacy of a H6 subtype avian influenza DNA vaccine in chickensJ Virol Methods201117322022621333689
- OidéAvian InfluenzaManual of Diagnostic Tests and Vaccines for Terrestrial Animals Office international des epizooties http://www.oie.int/eng/normes/mmanual/2008/pdf/2.03.04.Al.pdf
- KhatriKGoyalAKVyasSPPotential of nanocarriers in genetic immunizationRecent Pat Drug Deliv Formul20082688219075899
- MinigoGScholzenATangCKPoly-L-lysinecoated nanoparticles: a potent delivery system to enhance DNA vaccine efficacyVaccine2007251316132717052812
- XiangSDScholzenAMinigoGPathogen recognition and development of particulate vaccines: does size matterMethods2006401916997708
- LiGPLiuZGLiaoBZhongNSInduction of Th1-type immune response by chitosan nanoparticles containing plasmid DNA encoding house dust mite allergen Der p 2 for oral vaccination in miceCell Mol Immunol20096455019254479
- LoriFCalarotaSALisziewiczJNanochemistry-based immunotherapy for HIV-1Curr Med Chem2007141911191917691933