Abstract
Purpose:
To investigate to what degree the presence of hypertension (HTN) and poor glycemic control (GC) influences the likelihood of having microalbuminuria (MAU) among Cuban Americans with type 2 diabetes (T2D).
Methods:
A cross-sectional study conducted in Cuban Americans (n = 179) with T2D. Participants were recruited from a randomly generated mailing list purchased from Knowledge-Base Marketing, Inc. Blood pressure (BP) was measured twice and averaged using an adult size cuff. Glycosylated hemoglobin (A1c) levels were measured from whole blood samples with the Roche Tina-quant method. First morning urine samples were collected from each participant to determine MAU by a semiquantitative assay (ImmunoDip).
Results:
MAU was present in 26% of Cuban Americans with T2D. A significantly higher percentage of subjects with MA had HTN (P = 0.038) and elevated A1C (P = 0.002) than those with normoalbuminuria. Logistic regression analysis showed that after controlling for covariates, subjects with poor GC were 6.76 times more likely to have MAU if they had hypertension compared with those without hypertension (P = 0.004; 95% confidence interval [CI]: 1.83, 23.05).
Conclusion:
The clinical significance of these findings emphasizes the early detection of MAU in this Hispanic subgroup combined with BP and good GC, which are fundamentals in preventing and treating diabetes complications and improving individuals’ renal and cardiovascular outcomes.
Introduction
In past years, numerous studies have described the role of microalbuminuria (MAU) as a predictor of cardiovascular disease (CVD) and death among subjects with type 2 diabetes (T2D).Citation1–Citation3 MAU is one of the earliest clinical signs for diabetic nephropathy and a significant risk factor for progression to proteinuria.Citation1 Additionally, hypertensive T2D individuals with MAU have an increased risk of developing end-stage renal disease (ESRD).Citation4 Risk factors known to be associated with CVD and diabetic nephropathy are high blood pressure (BP) and elevated glycosylated hemoglobin (A1c).Citation5,Citation6 Achieving adequate BP and glycemic control (GC) plays an essential role in preventing renal and CVD events in individuals with T2D.
A current secondary analysis from the Hispanic Health and Nutritional Examination Survey (HHANES)Citation7 indicated that Cuban Americans have higher serum cholesterol and systolic BP than Puerto Ricans and Mexican Americans. Furthermore, compared with other Hispanic subgroups, Cuban Americans have the highest proportion of hypertension (HTN) and mean serum creatinine levels.Citation8 Smith and BarnettCitation9 examined the National Center for Health Statistics (NCHS) from 1996 to 1997 and concluded that Cuban Americans 35 years of age and older have the highest percentage of diabetes-related deaths compared with other Hispanics.
Although previous studies have shown significant differences and diversity within Hispanics, further studies conducted in the Cuban American population are scarce. Over the past decade, the prevalence of T2D has increased, especially among Cuban Americans who have a higher incidence of diabetes (8.2%) compared with 6.6% of non-Hispanic Whites.Citation10 The high incidence of T2D combined with an increased risk for developing diabetes complications warrants further examination of the Cuban American population. Screening for MAU can detect individuals at risk for renal dysfunction and CVD events and possibly reduce the burden associated with diabetes complications. Therefore, the purpose of this study was to investigate to what degree the coexistence of HTN and poor GC influences the likelihood of having MAU among Cuban Americans with T2D. It was hypothesized that individuals with T2D, HTN, and poor GC will have an increased likelihood to test positive for MAU. It was further hypothesized that this association will be stronger after controlling for confounding variables.
Methods
Design
This was a cross-sectional study conducted in Cuban Americans with and without T2D.
Study population
Data from a complete sample set of Cuban Americans with and without T2D were used in the present study. Recruitment of participants was conducted in alternate phases of potential subjects with and without T2D, age matching subjects by age groups. During a 1-year period, approximately 10,000 letters outlining the study were mailed to subjects aged 30 years or older with and without diabetes. Letters were sent in English and Spanish and included an invitation flyer to which interested participants could respond. The participants were initially recruited by random selection (every tenth address) from a randomly generated mailing list. The list of addresses was purchased from KnowledgeBase Marketing, Inc., Richardson, TX, USA. This company provided a mailing list of Cuban Americans identified as with and without T2D from Miami-Dade and Broward Counties, Florida. Three percent (n = 300) of the letters were returned due to unknown addresses. From the remaining delivered mail, 4% (n = 388) responded. Interested participants were initially interviewed on the phone, at which time the study purpose was explained and the age and gender of the responders were determined. To ascertain T2D status, each participant was asked for the age of diagnosis and initial treatment modalities. Only 18 subjects did not qualify for the study for not being Cuban Americans (n = 2), age younger than 30 years (n = 9), and having other chronic illnesses (n = 7). If a subject was determined to be eligible, then their participation was requested at the Human Nutrition Laboratory at Florida International University (FIU). Participants were instructed to refrain from smoking, consuming any food and beverages except water, and doing any unusual exercise for at least 8 hours prior to their blood collection. Subjects with T2D were matched for age and gender with subjects without diabetes. This study was approved by the Institutional Review Board at FIU. The purpose and protocol of the study were explained to the subjects, and their written consent, either in Spanish or English, was obtained prior to the commencement of the study. Seven participants reported not having diabetes but were reclassified because their lab results classified them as having T2D according to American Diabetes Association (ADA) standards. These subjects were given their laboratory results and referred to their physicians. For the data analysis, subjects with caloric intakes >5000 kcals (n = 2) and missing A1c levels (n = 2) were excluded. For two participants, we were unable to perform A1c analysis. In total, we included only the data from subjects with T2D (n = 179) who were aged 30 years and older.
Study variables
A sociodemographic questionnaire was given to each participant to complete, which included questions related to age, gender, smoking status, medications for diabetes, HTN, and cholesterol. Height and weight were measured using a Seca balance scale (Seca Corp, Columbia, MD, USA). Body mass index (BMI) was calculated as weight in kg/height in m2. BP was measured twice then averaged in participants in a sitting position after a 15-minute rest using a random zero sphygmomanometer (Tycos 5090-02 Welch Allyn Pocket Aneroid Sphygmomanometer, Arden, NC, USA) and a stethoscope (Littmann Cardiology, 3M, St Paul, MN, USA). HTN was defined as follows: systolic BP ≥ 140 mm Hg systolic or diastolic BP ≥ 90 mm Hg or using antihypertensive treatment.Citation11
Dietary assessment
Dietary intake was measured using a validated semiquantitative food frequency questionnaire (FFQ) developed by Willett et al.Citation12 This FFQ has also been validated by Nath and HuffmanCitation13 exclusively for the Cuban American population. Participants self-reported average consumption of specified amounts of various foods over the past year and chose from frequency responses ranging from “never” to “six or more servings per day”. In addition to food items, the FFQ included questions about type and duration of vitamin/mineral supplement use, alcohol consumption, and specific details about fat, salt, and sugar used in cooking and as condiments. Macro- and micronutrient intake was calculated by multiplying frequency of consumption by the nutrient value of the food item obtained from the Harvard University Food Composition Database (Boston, MA, USA).
Blood collection
Venous blood (20 mL) was collected from each subject after an overnight fast (at least 8 hours) by a certified phlebotomist using standard laboratory techniques. Blood samples were collected into a Vacutainer® Serum Separator Tube (SST) (Becton, Dickinson and Company, Franklin Lakes, NJ) for analysis of lipids and another tube containing ethylenediamine tetraacetic acid to analyze A1c. After coagulation was completed (30–45 minutes), the SST was centrifuged at 2500 RPM for 30 minutes. Lipid panel was assayed by enzymatic methods, and A1c percentages were measured from whole blood samples with the Roche Tina-quant method by Laboratory Corporation of America, Miami, FL, USA (LabCorp®). Poor GC was defined according to the ADA standards (A1c > 7%).Citation14
Urinary albumin
Fresh, single-voided, first morning urine samples were collected from each participant to determine MAU by a semi-quantitative assay (ImmunoDip, Diagnostic Chemicals Limited, Oxford, CT, USA). ImmunoDip Urinary Albumin Test uses a monoclonal antibody against human serum albumin to detect MAU. The study conducted by Davidson et alCitation15 was designed to evaluate the clinical performance of the ImmunoDip dipstick compared with a reference measure recommended by the ADA for detecting MAU (albumin:creatinine ratio <30 ug/mg [negative]; >30 ug/mg [positive]) determined by laboratory techniques (Quest Hitachi 717 autoanalyzer). Additionally, results from the ImmunoDip were compared with quantitatively measured albumin concentrations as a secondary outcome. Urinary albumin concentrations were considered <18 mg/L (negative) and >18 mg/L (positive). Screening for MAU with ImmunoDip exhibited a sensitivity of 96% and specificity of 80% when compared with albumin:creatinine ratio >30 ug/mg. When ImmunoDip was examined against quantitatively measured albumin concentrations, the dipstick yielded a sensitivity of 95% and specificity of 94%. Recommendations from the National Academy of Clinical Biochemistry (NACB) for the diagnosis and management of diabetes indicated that a useful semiquantitative screening test for MAU should have a sensitivity >95%.Citation16 The ImmunoDip dipstick fulfilled the requirements from the NACB as a screening tool to detect MAU. In our study, positive for MAU was defined as urinary albumin concentrations of >18 mg/L in spot collection. This cut-off value was established by the manufacturer (ImmunoDip, Diagnostic Chemicals Ltd) and corresponded to albumin:creatinine ratio >30 ug/mg values for MAU detection.Citation15
Data analysis
All analyses were performed using SPSS Version 17 (SPSS Inc., Chicago, IL, USA). T-tests and Chi-square tests were performed to compare means and proportion differences between subjects with and without MAU. Unadjusted odds ratios and logistic regression analysis were conducted to investigate the extent to which HTN and GC are associated with an increased likelihood of having MAU. Controlled variables included in the logistic regression analysis were age, gender, BMI, known duration of diabetes, total cholesterol levels, diabetes and cholesterol medications, smoking, total kcal and protein intake, and intake of potassium, phosphorous, and sodium. The level of significance was set at P < 0.05.
Results
MAU was present in 26% (n = 47) of Cuban Americans with T2D. There was a significantly higher percentage of subjects with MAU classified as hypertensive (P = 0.038) and taking diabetes medication (P = 0.039) compared with those without MAU. Additionally, subjects who tested positive for MAU had significantly higher A1c levels (P = 0.002) than those with normoalbuminuria ().
Table 1 Characteristics of subjectsTable Footnotea
Unadjusted odds ratios indicated that subjects with poor GC were 3.96 times more likely to have positive MAU if they had HTN compared with those without HTN (P = 0.014; 95% confidence interval [CI] 1.25, 12.5) (). Logistic regression analysis showed that after controlling for covariates, subjects with poor GC were 6.76 times more likely to have MAU if they had HTN compared with those without HTN (P = 0.004; 95% CI 1.83, 23.05) ().
Figure 1 Unadjusted odds ratios (OR) for microalbuminuria (MAU) among hypertensive Cuban Americans with poor glycemic control.a
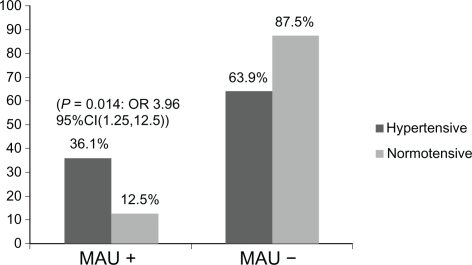
Table 2 Likelihood of having microalbuminuria among Cuban Americans with poor glycemic controlTable Footnotea
Discussion
The results of this study showed that HTN and poor GC are major contributors to increasing the likelihood of having MAU among Cuban Americans with T2D. The combination and/or interaction of these factors over time might increase the risk for progression to proteinuria/ESRD and CVD in this population. Our findings are supported by the multicenter study conducted in Europe that found that the likelihood of having MAU increases in patients when HTN and poor GC are present along with other coexisting risk factors for CVD.Citation17 Ravid et alCitation5 reported from their longitudinal study that a combination of risk factors, including abnormal BP, plasma cholesterol, A1c levels, high BMI, and male gender, identifies a group of individuals for poor renal and cardiovascular outcomes.
Maintaining adequate BP and GC is an important therapeutic goal among individuals with T2D. The UK Prospective Diabetes Study (UKPDS),Citation18 a longitudinal study with a 10-year median follow-up, showed that exposure over time to hyperglycemia was associated with diabetes complications in subjects with T2D. This study also indicated that for every 1% reduction in A1c level, the risk for microvascular complications decreased by 37% and diabetes-related death by 21%. A study by Thomaseth et alCitation19 showed that in hypertensive T2D subjects with incipient diabetic nephropathy, both tight BP control and optimal GC delay the progression of glomerular filtration rate deterioration. Additionally, hypertensive individuals with T2D under tight BP control experience a reduction in risk for microvascular and macrovascular complications.Citation20
The mechanism and pathways involving MAU with diabetic nephropathy and CVD are not fully understood. They may be interrelated with endothelial dysfunction and inflammation.Citation21 Stehouwer et alCitation22 examined the relationship between endothelial dysfunction and inflammation with MAU and risk of death in a prospective study among subjects with T2D. The results of that study showed that those participants with MAU, endothelial dysfunction, and inflammation had an increased risk in mortality; however, the associations of these variables with risk of mortality were independent from each other. Hyperglycemia and obesity were associated with an increase in markers of endothelial dysfunction and inflammation activity,Citation22 possibly indicating that the combinations of these factors may be interrelated in increasing the risk of death.
The usual course of MAU is progressive; however, not all T2D individuals with MAU will develop macroalbuminuria. Several authors have documented remission and/or regression of MAU in subjects with T2D.Citation23–Citation27 Antihypertensive therapy has been shown to reduce or slow the progression of diabetic nephropathy. In a 6-year prospective study, remission and regression to normoalbuminuria were observed in about 50% of T2D individuals.Citation23 Other factors independently linked with remission and/or regression of MAU were proper BP and GC and short duration of MAU. The study by Chan et alCitation24 with a 5-year mean follow-up of T2D patients with MAU treated with angiotensin-converting enzyme (ACE) inhibitor medications showed a 13% reduction in urinary albumin excretion (UAE). In addition, the authors pointed out the main role that BP and GC play in renal function. T2D individuals treated with angiotensin receptor blockers (ARBs) (eg, irbesartan and valsatran) experienced a 38% and 44% reduction in UAE over 2-year and 6-month follow-ups, respectively.Citation25,Citation26 Evidence from another prospective study with a 7.8-year follow-up indicated that 30% of the participants on antihypertensive therapy achieved remission to normoalbuminuria.Citation27 Additionally, the odds for remission to normoalbuminuria increased in these participants with every 1% decrease in A1c level. Furthermore, in a study conducted by Mogensen et al,Citation28 urinary albumin:creatinine ratio was decreased by 50% after a 3-month combination treatment with ARB and ACE inhibitors in hypertensive T2D individuals with MAU. Remission and/or regression of MAU may not only conserve renal function but also reduce the risk of CVD.
MAU is one of the earliest clinical signs of renal impairment. Testing for MAU has been recommended by the ADA in individuals with T2D to be performed at diagnosis of diabetes and every year afterwards.Citation29 The ImmunoDip dipstick is a rapid and easy screening test to perform, does not involve equipment and/or skilled personnel, exhibits a high sensitivity, requires only a random urine sample (first morning urine is recommended), and has a relatively low cost. However, this test does not quantify urinary albumin values and requires confirmation with a secondary analysis. This method can be used in a physician’s office and/or research setting as a first screening tool to detect the presence of MAU. The clinical significance of early screening and monitoring for MAU is possibly to improve individuals’ prognosis for microvascular and macrovascular complications, especially among T2D individuals with other concomitant conditions.
Limitations of the study
First, due to the cross-sectional design of the study, single-voided urine was collected to measure MAU, and we were not able to determine the cause–effect relationship between the variables. Second, due to the relatively small sample size in this study, our sample of Cuban Americans with T2D is not representative of the entire Cuban American population living in the USA. Nevertheless, to our knowledge, this is the first and only study that has examined the relationship between MAU, HTN, and GC in this Hispanic subgroup, which has an increased risk for T2D and CVD.
Conclusion
Early detection of MAU in this population may provide more valuable treatment and improve individuals’ renal and CVD outcomes. The therapeutic goals and strategies for MAU should focus on preventing long-term complications associated with T2D, such as kidney and heart diseases. Further investigations need to be carried out to fully understand the mechanism and absolute CVD risk that an individual with T2D has when MAU coexists with other comorbidities.
Acknowledgements
This research was funded by a grant from NIH/MBRS/SCOREAC#124401529/42 to the corresponding author.
Disclosure
The authors report no conflicts of interest in this work.
References
- MogensenCEMicroalbuminuria predicts clinical proteinuria and early mortality in maturity-onset diabetesN Engl J Med198431063563606690964
- DinneenSFGersteinHCThe association of microalbuminuria and mortality in non-insulin-dependent diabetes mellitus. A systematic overview of the literatureArch Intern Med199715713141314189224218
- ValmadridCTKleinRMossSEKleinBEThe risk of cardiovascular disease mortality associated with microalbuminuria and gross proteinuria in persons with older-onset diabetes mellitusArch Intern Med200016081093110010789601
- IsmailNBeckerBStrzelczykPRitzERenal disease and hypertension in non-insulin-dependent diabetes mellitusKidney Int19995511289893112
- RavidMBroshDRavid-SafranDMain risk factors for nephropathy in type 2 diabetes mellitus are plasma cholesterol levels, mean blood pressure, and hyperglycemiaArch Intern Med1998158999810049588433
- ParkJYKimHKChungYEIncidence and determinants of microalbuminuria in Koreans with type 2 diabetesDiabetes Care19982145305349571337
- AponteJDiabetes-related risk factors across Hispanic subgroups in the Hispanic health and nutritional examination survey (1982–1984)Public Health Nurs20091233819154190
- RodriguezRAHernandezGTO’HareAMCreatinine levels among Mexican Americans, Puerto Ricans, and Cuban Americans in the Hispanic Health and Nutrition Examination SurveyKidney Int20046662368237315569328
- SmithCABarnettEDiabetes-related mortality among Mexican Americans, Puerto Ricans, and Cuban Americans in the United StatesRev Panam Salud Publica200518638138716536924
- Centers for Disease Control and Prevention: 2007 National Diabetes Fact Sheet http://www.cdc.gov/diabetes/pubs/estimates07.htm#4. Accessed October 5, 2010.
- National High Blood Pressure Education Program Coordinating CommitteeThe Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 reportJ Am Med Assoc20032891925602572
- WillettWCSampsonLStampferMJReproducibility and validity of a semiquantitative food frequency questionnaireAm J Epidemiol198512251654014201
- NathSDHuffmanFGValidation of a semiquantitative food frequency questionnaire to assess energy and macronutrient intakes of Cuban AmericansInt J Food Sci Nutr20055630931416236592
- American Diabetes AssociationStandards of medical care in diabetes: 2010Diabetes Care201033Suppl 1S11S6120042772
- DavidsonMBBazarganMBakrisGImmunoDip: an improved screening method for microalbuminuriaAm J Nephrol200424328428815087587
- SacksDBBrunsDEGoldsteinDEGuidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitusClin Chem200248343647211861436
- RossiMCNicolucciAPellegriniFIdentifying patients with type 2 diabetes at high risk of microalbuminuria: results of the DEMAUND (Developing Education on Microalbuminuria for Awareness of reNal and cardiovascular risk in Diabetes) StudyNephrol Dial Transplant20082341278128418039647
- StrattonIMAdlerAINeilHAAssociation of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational studyBr Med J2000321725840541210938048
- ThomasethKPaciniGMorelliPImportance of glycemic control on the course of glomerular filtration rate in type 2 diabetes with hypertension and microalbuminuria under tight blood pressure controlNutr Metab Cardiovasc Dis200818963263818060749
- UK Prospective Diabetes Study GroupTight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study GroupBr Med J199831771607037139732337
- PerssonFRossingPHovindPEndothelial dysfunction and inflammation predict development of diabetic nephropathy in the Irbesartan in Patients with Type 2 Diabetes and Microalbuminuria (IRMAU 2) studyScand J Clin Lab Invest200868873173818609080
- StehouwerCDGallMAUTwiskJWIncreased urinary albumin excretion, endothelial dysfunction, and chronic low-grade inflammation in type 2 diabetes: progressive, interrelated, and independently associated with risk of deathDiabetes20025141157116511916939
- ArakiSHanedaMSugimotoTFactors associated with frequent remission of microalbuminuria in patients with type 2 diabetesDiabetes200554102983298716186402
- ChanJCKoGTLeungDHLong-term effects of angiotensin-converting enzyme inhibition and metabolic control in hypertensive type 2 diabetic patientsKidney Int200057259060010652036
- ParvingHHLehnertHBröchner-MortensenJIrbesartan in Patients with Type 2 Diabetes and Microalbuminuria Study Group. Long-term effects of angiotensin-converting enzyme inhibition and metabolic control in hypertensive type 2 diabetic patientsN Engl J Med20013451287087811565519
- VibertiGWheeldonNMMicroalbuminuria reduction with valsartan in patients with type 2 diabetes mellitus: a blood pressure-independent effectCirculation2002106667267812163426
- GaedePTarnowLVedelPRemission to normoalbuminuria during multifactorial treatment preserves kidney function in patients with type 2 diabetes and microalbuminuriaNephrol Dial Transplant200419112784278815328385
- MogensenCENeldamSTikkanenIRandomised controlled trial of dual blockade of reninangiotensin system in patients with hypertension, microalbuminuria, and non-insulin dependent diabetes: the candesartan and lisinopril microalbuminuria (CALM) studyBr Med J20003211440144411110735
- American Diabetes AssociationStandards of medical care in diabetes: 2009Diabetes Care200932Suppl 1S13S6119118286