Abstract
Interferon-beta is widely used for the treatment of relapsing multiple sclerosis. The drug is usually well tolerated, but autoimmune adverse effects, including kidney disease, have been reported. Only a few cases of hemolytic uremic syndrome-thrombotic microangiopathy associated interferon-alpha have been described so far, and even fewer with beta-interferon. We report a patient who developed thrombotic microangiopathy during treatment with interferon-beta and improved after discontinuation and steroid therapy. Complement cascade and antiphospholipid antibodies are investigated. The spectrum of renal diseases associated with interferon-beta treatment is also reviewed.
Introduction
Interferons are well established agents for standard therapy in several malignancies, hepatitis C, idiopathic pulmonary fibrosis, and multiple sclerosis.Citation1,Citation2 Despite this, adverse autoimmune effects associated with their use have been reported, including minimal change disease in the kidney,Citation2–Citation5 collapsing focal segmental glomerulosclerosis,Citation6,Citation7 membranous glomerulonephritis,Citation8 acute renal failure,Citation9 lupus nephritis,Citation10,Citation11 acute renal failure,Citation12 and thrombotic microangiopathy.Citation13–Citation18 These side effects are most often associated with interferon-alpha therapy, rather than interferon-beta. The mechanism for this is not clear. Glomerular endothelial cells express and secrete ADAMTS 13.Citation17 The low activity of ADAMTS 13 has been associated with the presence of an anti- ADAMTS 13 IgG antibody during treatment with interferon-alpha 2a,Citation16 which could explain these adverse side effects, but no mechanism has been described to explain this with interferon-beta. In the following report, we describe a case of hemolytic uremic syndrome causing thrombotic microangiopathy and chorioretinitis after several months on treatment with interferon-beta which is much rarer. It responded successfully to drug withdrawal and steroid therapy.
Case report
A 37-year-old woman was admitted to our hospital with acute renal failure, hypertension, subnephrotic proteinuria, nausea, and vomiting. She reported a 20-year history of multiple sclerosis, adequately controlled with steroids. She had been treated with interferon-beta due to a sensitive relapse affecting the spinal cord and both legs during the last five months. The patient refused other medications. She had no recent history of fever or diarrhea. She reported a two-week history of mild fatigue and arthralgia in the left tarsus, treated with ibuprofen. On admission, the patient had a blood pressure of 205/110 mmHg. She was well hydrated and, apart from pedal edema, physical examination was unremarkable. No skin lesions were detected.
Laboratory test results are shown in . A possible diagnosis of acute renal injury secondary to thrombotic microangiopathy associated with interferon-beta was suggested. Urinalysis showed no leucocytes, erythrocytes, or nitrites. Proteins were 1.7 g/24 hours. Urine culture showed no pathogens.
Table 1 Results of laboratory investigations
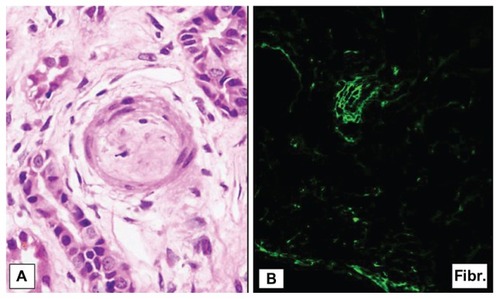
Cancer markers were negative. Chest x-ray was unremarkable and renal ultrasound showed kidneys of normal size with a normal echogenic cortex and no hydronephrosis. A kidney biopsy was performed and histological studies showed ischemic changes in 12 of 35 glomeruli studied (). Some other glomeruli showed chronic glomerular microangiopathic lesions with duplication of the glomerular basement membrane (). There was moderate interstitial edema with mild inflammatory cell infiltration and patchy tubular atrophy. The arterioles and intralobular arteries showed marked subintimal fibromucoid edema narrowing the lumen ( arrows, ). An immunofluorescence study showed only fibrinogen deposits in the arterial wall ().
Figure 1 (A) Ischemic changes in the upper glomeruli (arrow). Marked subintimal fibromucoid edema narrowing the lumen in the intralobular arterioles (arrows) and (B) duplication of glomerular basement membrane.
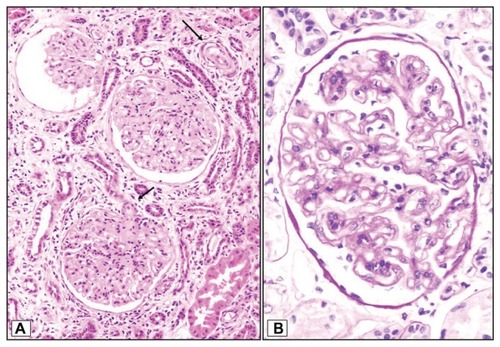
Figure 2 (A) Moderate interstitial edema with mild inflammatory cell infiltration and patched tubular atrophy with (B) fibrinogen deposits in the arterial wall in the immunofluorescence study.
The patient was finally diagnosed with thrombotic microangiopathy associated with interferon-beta, so the drug was withdrawn and immunosuppressive therapy was started with 1 mg/kg/day of prednisone because leg symptoms of multiple sclerosis had started immediately. Doses of steroids were reduced and finally withdrawn over a period of one month, while glatiramer acetate was started. The leg symptoms of multiple sclerosis disappeared in a few days. Her hypertension was controlled with enalapril and irbesartan. Hematological abnormalities and serum lactate dehydrogenase levels returned to the normal range, and renal function slowly recovered a serum creatinine of 1.0 mg/dL.
Discussion
Interferon-beta is widely used for the treatment of relapsing multiple sclerosis. It is postulated that interferon-beta acts in this disease by inhibiting activation and proliferation of T cells.Citation1,Citation2 The drug is usually well tolerated, but constitutional side effects and autoimmune adverse events have been reported.Citation19,Citation20
The similarities between some manifestations of systemic lupus erythematosus, those of viral infections, and side effects of immunotherapy with recombinant interferons, such as fever, arthralgia, myalgia, and fatigue, are evident. In fact, interferon-alpha is a central mediator in systemic lupus erythematosus, and specific neutralizing antibodies are now in clinical trials for the treatment of this disease.Citation21 Our case can be immediately catalogued as a thrombotic microangiopathy-hemolytic uremic syndrome, which would explain the acute kidney injury. The absence of diarrhea made atypical hemolytic uremic syndrome very unlikely. She had no symptoms or serological findings suggestive of systemic sclerosis, malignancy, malignant hypertension, or antiphospholipid syndrome. The presence of autoreactive antibodies, particularly antiphospholipid antibodies and antithyroid antibodies, are associated with an increased risk of interferon-beta antibodies in patients with multiple sclerosis on long-term therapy.Citation22 However, we did not find any of these antibodies in our patient. Kidney complications have not been directly attributed to multiple sclerosis.Citation2
Renal side effects including minimal change disease,Citation2–Citation5 collapsing focal segmental glomerulosclerosis,Citation6–Citation8 membranous nephropathy,Citation9 lupus nephritis,Citation10,Citation11 acute renal failure,Citation12 and thrombotic microangiopathy,Citation13–Citation23 are most often associated with interferon therapy rather than with interferon-beta. The incidence of transient proteinuria during interferon-beta therapy is around 20%. To our knowledge, this is the fourth case of hemolytic uremic syndrome induced by interferon-beta. Two of these patients were treated with corticosteroids and plasmapheresis, and another was only treated with supportive antihypertensive and antiproteinuric therapies. The fourth patient was diagnosed also with pseudo-SLE and treated with immunosuppressants. In all of them interferon-beta was withdrawn. The spectrum of kidney disease related to interferon-beta is shown in .
Table 2 Spectrum of renal diseases induced by interferon-beta
The mechanism by which interferon could induce thrombotic microangiopathy lesions and nephrotic syndrome remains unclear.Citation14 Pleiotropic drugs such as interferon might disrupt complex pathways of complement regulation and play a role in endothelial damage.Citation21 In recent years, mutation of complement system regulators (factors H and I, and membrane cofactor protein) have been directly implicated in the induction of atypical hemolytic uremic syndrome.Citation24,Citation25 However, we did not found any of these alterations in our case. Furthermore, a recent publication described a case of low ADAMTS 13 activity associated with the presence of an anti-ADAMTS 13 IgG antibody during treatment with interferon-alpha 2a.Citation16 Glomerular endothelial cells express and secrete ADAMTS 13.Citation17 It has been suggested that pre-eclampsia is also associated with decreased levels of ADAMTS 13.Citation18
The delayed appearance of thrombotic microangiopathy observed in our case and others suggest that the development of renal lesions may be the result of cumulative effects.Citation14,Citation22 In conclusion, thrombotic microangiopathy-hemolytic uremic syndrome induced by interferon-beta is an unusual side effect manifested as acute or subacute kidney injury. Attempts should be made to detect it as soon as possible, and to clarify the mechanism of microangiopathy lesions.
Disclosure
The authors report no conflicts of interest in this work.
References
- WaltherEUHohlfeldRMultiple sclerosis: side effects of interferon beta therapy and their managementNeurology1999531622162710563602
- AravindanAYongJKillingsworthMSuranyiMWongJMinimal change disease with interferon-beta therapy for relapsing remitting multiple sclerosisNDT Plus20103132134
- KamasakaRNakamuraNShiratoKNephrotic syndrome associated with interferon beta-1b therapy for multiple sclerosisClin Exp Nephrol20061022222517009081
- TolaMRCaniattiLMGragnanielloDRecurrent nephrotic syndrome in patient with multiple sclerosis treated with interferon beta 1aJ Neurol200325076876912862038
- NakaoKSugiyamaHMakinoEMinimal change nephrotic syndrome developing during postoperative interferon-beta therapy for malignant melanomaNephron20029049850011961411
- GotsmanIElhalel-DarnitskiMFriedlanderZBeta-interferon-induced nephrotic syndrome in a patient with multiple sclerosisClin Nephrol20005442542611105807
- MarkowitzGSNasrSHStokesMBD’AgatiVDTreatment with INF-α, -β or -γ is associated with collapsing focal segmental glomerulosclerosisClin J Am Soc Nephrol2010560761520203164
- BremerCTLastrapesAAlperABJrInterferon-alpha-induced focal segmental glomerulosclerosis in chronic myelogenous leukemia: a case report and review of the literatureAm J Clin Oncol20032626226412796597
- AutyASalehANephrotic syndrome in a multiple sclerosis patient treated with interferon beta 1aCan J Neurol Sci20053236636816225183
- AbbottIJChangCCSkinnerMJDevelopment and management of systemic lupus erythematosus in an HIV-infected man with hepatitis C and B co-infection following interferon therapy: a case reportJ Med Case Reports200937289
- HansenTNewDReeveRDonneRStephensWAcute renal failure, systemic lupus erythematosus and thrombotic microangiopathy following treatment with beta-interferon for multiple sclerosis: case report and review of the literatureNDT Plus20092466468
- FahalIHMurryNChuPBellGMAcute renal failure during interferon therapyBr Med J19933069738490476
- JadoulMPiessevauxHFerrantACosynsJPvan Ypersele de StriouCRenal thrombotic microangiopathy in patients with chronic myelogenous leukaemia treated with interferon alpha 2bNephrol Dial Transplant1995101111137724004
- BadidCMcGregorBFaivreJMRenal thrombotic microangiopathy induced by interferon αNephrol Dial Transplant20011684684811274286
- MageeCCRenal thrombotic microangiopathy induced by interferon-alphaNephrol Dial Transplant2001162111211211572913
- KitanoKGiboYKamijoAThrombotic thrombocytopenic purpura associated with pegylated-interferon alpha-2a by ADAMTS 13 inhibitor in a patient with chronic hepatitis CHaematologica200691ERC34
- TatiRKristofferssonACStåhlALPhenotypic expression of ADAMTS 13 in glomerular endothelial cellsPLoS One20116e2158721720563
- StepanianACohen-MoattiMSanglierTECLAXIR Study GroupVon Willebrand factor and ADAMTS13: a candidate couple for preeclampsia pathophysiologyArterioscler Thromb Vasc Biol2011311703170921512165
- AlanogluGKilbasSArslanCSenolAKutluhanSAutoimmune hemolytic anemia during interferon-beta-1b treatment for multiple sclerosisMult Scler20071368368517548453
- GargNWeinstock-GuttmanBBhasiKLockeJRamanathanMAn association between autoreactive antibodies and anti-interferon-beta antibodies in multiple sclerosisMult Scler20071389589917468449
- BroughtonACosynsJPJadoulMThrombotic microangiopathy induced by long-term interferon-β theraphy for multiple sclerosis: a case reportClin Nephrol2011539640022000560
- UbaraYHaraSTakedatuHHemolytic uremic syndrome associated with beta-interferon therapy for chronic hepatitis CNephron1998801071089730725
- HerreraWGBalizetLBHarbertsSWBrownSTOccurrence of a TTP-like syndrome in two women receiving beta interferon therapy for relapsing multiple sclerosisNeurology1999Supp 2A153
- AndersHJLichnekertJAllamRInterferon-α and -β in kidney inflammationKidney Int20107784885420237459
- NorisMRemuzziGAtypical hemolytic-uremic syndromeN Engl J Med20093621676167919846853