Abstract
Purpose
Evaluation of vitamin D (vD) status and risk factors for low vD among breastfeeding mother–infant dyads in a population at high risk for vD deficiency.
Subjects and methods
We measured serum 25-hydroxyvitamin D (25(OH)D) and parathyroid hormone at 1 month postpartum in 60 consecutive exclusively breastfeeding Arab mother–infant dyads enrolled in a high dose vD supplementation study to prevent vD deficiency in Doha, Qatar, (latitude 25°N) during summer months. Data were collected on demography, sun exposure, and vD supplementation. Comparison with a US cohort was evaluated. vD deficiency was defined as serum 25(OH)D <50 nmol/L and severe deficiency categorized as 25(OH)D <25 nmol/L in mothers and infants.
Results
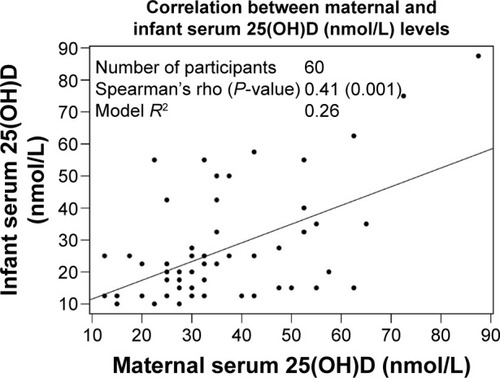
Mean maternal age was 29 years and 77% had college or university education. Maternal median 25(OH)D was 32.5 nmol/L and 78% were vD-deficient and 20% had 25(OH)D <25 nmol/L. Only 42% of mothers had reportedly taken vD supplements postpartum and median dietary vD intake (119 IU/day) and calcium (490 mg/day) were low. Maternal median sun index score (sun exposure [hours/week] × body surface area exposed while outdoors) was 0. Maternal 25(OH)D correlated with percent body surface area exposure while outdoors (rs=0.37, P=0.004). Infant median 25(OH)D was 20 nmol/L and 83% were deficient, while 58% had 25(OH)D <25 nmol/L. Infant 25(OH)D correlated with maternal levels (rs=0.41, P=0.001). None of the infants received vD supplement at 1 month of age and median sun index score was 0. Infant’s parathyroid hormone showed negative correlations with 25(OH)D (rs=−0.28, P=0.03). Sun exposure, vD supplementation rate, and vD status were lower in Doha than Cincinnati, US cohort.
Conclusion
vD deficiency is common in breastfeeding mother–infant dyads in this sunny environment and is associated with sun avoidance and low vD intake. We suggest corrective vD supplement of breastfeeding mothers and their infants, which should preferably start during pregnancy.
Introduction
Vitamin D (vD) status in humans mostly depends on skin exposure to ultraviolet B radiation and dietary sources provide only a small amount of body vD requirement.Citation1 vD deficiency leads to serious health consequences, such as rickets in infants and childrenCitation2 and osteomalacia in adults.Citation3 Epidemiologic studies have also shown that vD deficiency or inadequate vD intake during infancy is associated with an increased rate of lower respiratory tract infections in infancyCitation4 and childhoodCitation5,Citation6 and autoimmune-related disease, such as type 1 diabetes.Citation7 However, reduction in childhood pneumonia by vD supplementation has not been proven.Citation8 vD deficiency is common among breastfed infants who lack sunlight exposure and do not receive vD supplementation because of inadequate vD in human milk.Citation2,Citation9,Citation10 Additional factors contributing to low vD status in breastfed infants include low maternal vD status, which would predispose to low infant vD stores at birth and low vD intake from human milk.Citation11,Citation12 Given the importance of breastfeeding and the interrelationship between maternal and infant vD status,Citation12 vD nutrition of breastfeeding mother–infant dyads and the associated risk factors should be of global concern, especially in populations at high risk of vD deficiency.Citation10
In comparison with reports from Western countries, vD deficiency and rickets are more common in infants in South AsianCitation2,Citation13 and Middle Eastern countries,Citation10,Citation14 including Qatar.Citation15 Nutritional rickets were diagnosed in 24% of 540 children attending primary health care clinics in DohaCitation16 and hypocalcemic seizure is reported as a common presentation of vD deficiency in breastfed infants in association with maternal vD deficiency in Qatar.Citation17 Nevertheless, the magnitude of vD deficiency and the relationship among vD status, sunlight exposure, and vD intake in breastfeeding mother–infant dyads, in this and other high-risk populations have not been adequately studied. We, therefore, carried out a study to evaluate the magnitude and risk factors for low vD status in breastfeeding Arab mother–infant dyads in Doha, Qatar (latitude 25°N). We assessed the relationship among maternal and infant vD status and vD intake from diet or supplement, calcium dietary intake, and sunlight exposure.
Subjects and methods
The mothers were recruited after delivery if they planned to breastfeed for 6 months and agreed to participate in the study. We measured prospectively serum 25-hydroxyvitamin D (25(OH)D) and serum intact parathyroid hormone (PTH) on enrollment at 4 weeks postpartum. The measurement was carried out in 60 consecutive breastfeeding mother–infant dyads among those enrolled in a randomized controlled trial of high-dose vD supplementation to prevent vD deficiency in lactating mothers and their infants. The randomized controlled trial was approved by Hamad Medical Corporation/Weill Cornell Medical College in Qatar joint Institutional Review Board (#13-0036). The mothers gave informed consent to use the information for publications without identifying the mother or the infant.
Eligible subjects were Arab mothers who delivered at term (≥37-week gestation) at Women’s Hospital Al-Wakra, Doha, Qatar, without any reported illness that could affect vD status. Qatar is located at latitude 25°N and the subjects were studied during summer (August and September 2014). The mothers who consented to the trial were enrolled with the infants by the research assistants at 4 weeks postpartum. Demographic, maternal dietary vD, and vD supplements data were collected by trained research nurses using standardized questionnaires. Nutrition Data System for Research (Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN, USA) was used to assess the vD and calcium intakes from food reported in the dietary recall interview. vD supplement intake was assessed during the interview.
Data were also collected on sun exposure behavior, which included the duration of sun exposure and the body surface area (BSA) exposed to sunlight while outdoors. BSA exposed while outdoors was based on the usual mode of clothing using a standardized questionnaire () as previously reported.Citation18 The questionnaire was administered by a research nurse to each mother and her infant at enrollment. Total percentage of BSA exposure while outdoors was calculated as a sum of percentage BSA exposure associated with the subject’s responses for each part of the body. Duration of direct sunlight exposure (hours/week) was also documented. A sun index score which has been shown to correlate with vD status in adults and infantsCitation19–Citation21 was calculated as a product of duration of sunlight exposure (hours/week) and percent BSA exposure while outdoors.
Table 1 Calculation of percent body surface area (% BSA) exposed to sunlightTable Footnotea
Total serum 25(OH)D concentrations were measured by direct competitive chemiluminescence immunoassay on DiaSorin liaison platform (DiaSorin Liaison, Saluggia, VC, Italy). The intra- and inter-assay coefficients of variation were 9.1% and 11.1%, respectively. Serum intact PTH concentrations were measured by chemiluminescence immunoassay (Unicel DxL 600; Beckman Coulter, Inc., Brea, CA, USA) platform. The intra- and inter-assay coefficients of variation were 2.1% and 3.9%, respectively. vD deficiency was defined as serum 25(OH)D <50 nmol/L as a priori cutoff value.Citation22 For this study, serum 25(OH)D <25 nmol/L, which is associated with increased risk of osteomalacia or rickets, was categorized as severe deficiency.Citation10,Citation23
The primary outcome measure was the prevalence of vD deficiency in mothers and infants. The secondary outcome measures were risk factors for vD deficiency. Statistical analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, NC, USA) and statistical significance was set a priori as P<0.05. Spearman’s correlations were used to assess correlations between vD intake and sunlight exposure behaviors and vD status in mothers and infants. Student’s t-tests were conducted to examine differences in normally distributed variables and Wilcoxon rank-sum tests were used when appropriate to test for differences in nonnormally distributed variables. One-way analysis of variance was used to test for associations between categorical and normally distributed continuous variables. The Kruskal–Wallis test was used when appropriate for analyses involving categorical data and nonnormally distributed continuous variables. We also compared sun exposure and vD supplementation and vD status of mother–infant dyads in the current study with a cohort consisting of Caucasian and African–American exclusively breastfeeding mother–infants dyads studied in summer in Cincinnati, OH, USA.Citation18 The Cincinnati cohorts were studied at similar postpartum age, season, and with a comparable method of assessing sun exposure behaviors as in Doha subjects.
Results
Mothers
The mean (standard deviation) maternal age was 29 (4) years. Three (5%) had up to elementary education, eleven (18%) had high school education, and 46 (77%) had college or university education.
The median (interquartile range) serum 25(OH)D was 32.5 nmol/L (25, 45). A total of 47 (78%) mothers were vD-deficient (serum 25(OH)D <50 nmol/L). While 35 (58%) had serum 25(OH)D 25–<50 nmol/L, 12 (20%) were severely deficient (serum 25(OH)D <25 nmol/L). There was a negative correlation between serum 25(OH) D and PTH levels, but the correlation was not statistically significant (rs=−0.22, P=0.09). A total of 21 (35%) mothers had serum 25(OH)D <30 nmol/L and would have been regarded deficient if serum 25(OH)D <30 nmol/L is considered as vD deficiency as recommended by the Institute of Medicine.Citation23
Nineteen (32%) mothers had reported taking prenatal vitamin during pregnancy and 25 (42%) reported taking vD supplementation postpartum. The median dietary vD postpartum and dietary calcium were 119 IU/day (72, 147) and 490 mg/day (353, 698), respectively. The median BSA exposed when outdoors was 9% (9, 16). The median duration of outdoor sunlight exposure was 0 hours/week (0, 0). The median sun index score (duration of sun exposure in hours/week × BSA exposed while outdoors) was also 0 (0, 0).
Predictors of vD status in breastfeeding mothers
In univariate analysis, maternal age (rs=0.30, P<0.02) and the percent BSA exposure while outdoors (rs=0.37, P<0.004) significantly correlated with maternal serum 25(OH)D concentrations. There were no significant relationships between maternal serum 25(OH)D concentrations and educational level, postpartum vD dietary and calcium intakes, and vD supplementation use.
Infants
The infant median 25(OH)D concentration was 20 nmol/L (12.5, 33.8). A total of 50 (83%) infants were vD-deficient (serum 25(OH)D <50 nmol/L), 15 (25%) had values 25–<50 nmol/L, and 35 (58%) were severely deficient (serum 25(OH)D <25 nmol/L). A total of 43 (72%) infants had serum 25(OH)D <30 nmol/L and would have been regarded deficient if serum 25(OH)D <30 nmol/L is considered as vD deficiency as recommended by the Global Consensus Recommendations on Prevention and Management of Nutritional Rickets.Citation24 Infant serum 25(OH) D concentrations were significantly correlated with maternal values (rs=0.41, P=0.001) (). There was a significant negative correlation between infants’ PTH values and 25(OH)D concentrations (rs=−0.28, P=0.03).
Figure 1 Correlation between maternal and infant serum 25(OH)D concentrations.
Abbreviation: 25(OH)D, 25-hydroxyvitamin D.
None of the infants had received vD supplementation by 4 weeks of age. The median percent BSA exposed when infants are outdoors as indicated by the mode of clothing was 26% (14, 28), and the median duration of sunlight exposure in hours/week during the period covered in the interview was 0 hours/week (0, 0). The median sun index score (duration of sun exposure in hours/week × percent BSA exposed while outdoors) was 0 (0, 0). No statistically significant associations were found between infants’ serum 25(OH)D concentrations and sunlight exposure behaviors.
Comparison of Doha with Cincinnati cohorts
In and , we compared data on the sun exposure behaviors, vD supplementation use, and vD status of the mothers () and infants () among the Doha subjects and a subset of Cincinnati exclusively breastfeeding mother–infant dyads studied in summer.Citation18 The sun exposure behaviors, vD supplementation rate, and vD status in summer months were lower in mothers and infants in the Doha cohort than in the cohort of Cincinnati mother–infant dyads.
Table 2 Maternal sun exposure, vitamin D supplement, and vitamin D status in Doha and Cincinnati studyTable Footnote*
Table 3 Infant sun exposure, vitamin D supplement, and vitamin D status in Doha and Cincinnati studyTable Footnote*
Discussion
From this study, vD deficiency appears highly prevalent in Arab mothers and breastfeeding infants in Doha, Qatar, at latitude 25°N. Severe deficiency associated with increased risk of rickets was common in the infants. As anticipated, vD deficiency in mothers was associated with low sunlight exposure and inadequate vD intake. Most of the mothers lacked exposure to sunlight and wore extensive clothing, which contribute to minimal BSA exposure while outdoors. The sun index core was negligible despite abundant sunshine at a latitude that could support significant vD synthesis in the summer months when the study was done.Citation25 Lack of variations in sun index scores and small sample size prevented the use of linear regression remodeling. However, compared with a cohort of mothers of mixed ethnicity in Cincinnati with similar average available sunshine hours/day, the Cincinnati cohort had a median sun index score of 196 compared with a score of 0 among the Doha mothers in summer months. In spite of the high degree of sunshine deprivation, postpartum vD supplementation was reported in only 42% of mothers in Qatar and the intake was in the form of multivitamins, which provided 20–400 IU of vD per day. The prenatal use of vD supplements was lower than postnatal use and the reason was not clear. The average maternal daily dietary vD (119 IU) was low. It is, therefore, not surprising that a very high proportion (78%) of the mothers in the study had vD deficiency (serum 25(OH)D level <50 nmol/L) compared with 11% in the cohort of mothers from Cincinnati. The high prevalence of college education among the mothers in the study is a reflection of patient characteristics, who were mostly Arab expatriates. Expatriates require higher education for employment in the health institutions. It is of interest that in this and another studyCitation16 from Qatar, higher educational status was not associated with higher vD status. This may be because sun avoidance behavior is similar irrespective of educational status.
We conclude that low sun exposure combined with inadequate corrective vD intake contributed to the low vD status and high prevalence of vD deficiency among Arab mothers in Doha.
vD deficiency of varying degrees has been reported previously among breastfeeding mothers in other at-risk populations in Mexico,Citation26 the People’s Republic of China,Citation26 Turkey,Citation27 India,Citation28 and the United Arab Emirates.Citation29 In these studies, different cutoff values of serum 25(OH)D concentrations were used to define vD deficiency. In a Global Exploration of Human Milk study of cohorts of exclusive breastfeeding mothers, 62% of 113 mothers from Mexico City and 52% of 112 mothers from Shanghai had serum 25(OH)D <50 nmol/L, while only 6.2% of mothers in Mexico City and 2.5% of mothers in Shanghai had serum 25(OH)D <30 nmol/L.Citation26 In contrast, studies from Turkey,Citation27 India,Citation28 and the United Arab EmiratesCitation29 reported 46%, 48%, and 61% of mothers, respectively, had serum 25(OH)D <25 nmol/L categorized as severe deficiency. In the Global Exploration of Human Milk study,Citation26 which evaluated sunlight exposure and vD supplementation use in relation to vD status of breastfeeding mothers and infants, the authors concluded that the prevalence of vD deficiency in diverse populations appear to depend on sunlight exposure behaviors and vD supplementation use. This is in support of the findings in this study.
The associations of low vD status in the mothers include increased risk of osteomalacia and possibly cancers and autoimmune diseases.Citation3,Citation30 Mothers in this study are likely to have low vD status at birth. As vD status of the infants at birth is related to the mothers’ vD,Citation11,Citation31 the infants of such mothers are likely to have low vD stores at birth. In addition, mothers with low vD are likely to produce milk that is deficient in vD for their nursing infants. Therefore, in breastfeeding mothers with vD deficiency, their infants are at an increased risk of continuing low vD status during infancy, which could lead to development of rickets and an increased risk of lower respiratory infections.Citation4–Citation6
The high prevalence of vD deficiency in infants in this study is not unexpected because most infants were unsupplemented with vD at the time of study and lacked sunlight exposure. vD supplementation of breastfeeding infants at an age of 2–12 months is recommended by the Ministry of Health as part of health policy for infants in this population. The infants in this study were enrolled at 1 month of age and hence were not on vD supplementation. As reported by the mothers, most of the infants were not exposed to sunlight. This could be due to the time of the study because according to the custom, mothers usually stay indoors and infants are not taken out in the first 40 days after birth. The median sun index score, therefore, was 0 compared with a median score of 84 among a Cincinnati cohort living at a similar latitude but who do not have the custom of postnatal restriction. In addition, we speculate that the low vD status is aggravated by low vD stores at birth and low human milk vD intake due to maternal vD deficiency. There is a need for increased awareness among health care providers in this environment of the risk of high prevalence of vD deficiency among breastfeeding mother–infant dyads in early postpartum. Therefore, vD supplementation should start from birth as recommended by the Global Consensus Recommendation on Prevention and Management of Nutritional Rickets and the American Academy of Pediatrics for the prevention of rickets.Citation24,Citation32
In view of the high prevalence of vD deficiency in mothers and infants, preventive strategies should target both mothers and infants. It is of note that recent studies have shown that high-dose maternal vD supplementation of 5,000 IU/dayCitation33 and 6,400 IU/dayCitation34 alone during lactation repletes mother and infant vD status without adverse events and provides a possible option to prevent vD deficiency in the mother and her nursing infant. If the objective of vD supplementation during lactation is to prevent vD deficiency in breastfeeding mothers and their infants, studies of maternal supplementation alone are warranted especially in populations where vD deficiency is of epidemic proportion.
Limitations
The limitations of this study include a small sample size. In addition, the number of the comparative mother–infant groups from Cincinnati was small and included non-Arabs of mixed ethnicity. We did not evaluate the effect of skin pigmentation, which can affect vD synthesis. However, our study provided additional information on vD status and associated risk factors for low vD status in this high-risk population.
Conclusion
In conclusion, this study confirms a high prevalence of vD deficiency in exclusively breastfeeding mother–infant dyads, which is associated with lack of sunlight exposure and inadequate vD intake in an area with abundant natural sunshine. Because of interrelationship between mother and infant vD status, especially in a setting of exclusive breastfeeding, we suggest a vD supplementation strategy to prevent vD deficiency in both mothers and infants in this and other populations at a high risk of vD deficiency.
Acknowledgments
This study is financially supported by Qatar National Research Fund (NPRP 6-1151-3-275). An abstract on the prevalence and risk factors for low vitamin D status among breastfeeding mothers and infants was presented at the Annual Pediatrics and Pediatric Emergency Medicine Conference from March 29 to 31, 2016, Atlanta, GA, USA, as part of a report on randomized controlled trial of vitamin D supplementation to prevent vitamin D deficiency in Arab mothers and infants in Qatar.
Disclosure
The authors report no conflicts of interest in this work.
References
- HolickMFMcCollum Award Lecture, 1994: vitamin D – new horizons for the 21st centuryAm J Clin Nutr19946046196308092101
- ThacherTDFischerPRStrandMAPettiforJMNutritional rickets around the world: causes and future directionsAnn Trop Paediatr200626111616494699
- HolickMFVitamin D deficiencyN Engl J Med2007357326628117634462
- KaratekinGKayaASalihogluOBalciHNuhogluAAssociation of subclinical vitamin D deficiency in newborns with acute lower respiratory infection and their mothersEur J Clin Nutr200963447347718030309
- WayseVYousafzaiAMogaleKFilteauSAssociation of subclinical vitamin D deficiency with severe acute lower respiratory infection in Indian children under 5 yEur J Clin Nutr200458456356715042122
- RothDEShahRBlackREBaquiAHVitamin D status and acute lower respiratory infection in early childhood in Sylhet, BangladeshActa Paediatr201099338939319900174
- HypponenELaaraEReunanenAJarvelinMRVirtanenSMIntake of vitamin D and risk of type 1 diabetes: a birth-cohort studyLancet200135892921500150311705562
- Manaseki-HollandSMaroofZBruceJEffect on the incidence of pneumonia of vitamin D supplementation by quarterly bolus dose to infants in Kabul: a randomised controlled superiority trialLancet201237998241419142722494826
- WeisbergPScanlonKSLiRCogswellMENutritional rickets among children in the United States: review of cases reported between 1986 and 2003Am J Clin Nutr2004806 Suppl1697S1705S15585790
- DawoduAAgarwalMSankarankuttyMHardyDKochiyilJBadrinathPHigher prevalence of vitamin D deficiency in mothers of rachitic than nonrachitic childrenJ Pediatr2005147110911116027707
- HollisBWWagnerCLAssessment of dietary vitamin D requirements during pregnancy and lactationAm J Clin Nutr200479571772615113709
- DawoduATsangRCMaternal vitamin D status: effect on milk vitamin D content and vitamin D status of breastfeeding infantsAdv Nutr20123335336122585912
- AgarwalNFaridiMMAggarwalASinghOVitamin D Status of term exclusively breastfed infants and their mothers from IndiaActa Paediatr201099111671167420545930
- MollaAMBadawiMHal-YaishSSharmaPel-SalamRSMollaAMRisk factors for nutritional rickets among children in KuwaitPediatr Int200042328028410881586
- BenerAAl-AliMHoffmannGFHigh prevalence of vitamin D deficiency in young children in a highly sunny humid country: a global health problemMinerva Pediatr2009611152219179999
- BenerAHoffmannGFNutritional rickets among children in a sun rich countryInt J Pediatr Endocrinol2010201041050221048925
- SolimanASalamaHAlomarSShatlaEEllithyKBedairEClinical, biochemical, and radiological manifestations of vitamin D deficiency in newborns presented with hypocalcemiaIndian J Endocrinol Metab201317469770323961489
- DawoduAZallaLWooJGHeightened attention to supplementation is needed to improve the vitamin D status of breastfeeding mothers and infants when sunshine exposure is restrictedMatern Child Nutr201410338339722708508
- SpeckerBLValanisBHertzbergVEdwardsNTsangRCSunshine exposure and serum 25-hydroxyvitamin D concentrations in exclusively breast-fed infantsJ Pediatr198510733723763839846
- DawoduAAbsoodGPatelMBiosocial factors affecting vitamin D status of women of childbearing age in the United Arab EmiratesJ Biosoc Sci19983044314379818552
- Barger-LuxMJHeaneyRPEffects of above average summer sun exposure on serum 25-hydroxyvitamin D and calcium absorptionJ Clin Endocrinol Metab200287114952495612414856
- HolickMFBinkleyNCBischoff-FerrariHAEvaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guidelineJ Clin Endocrinol Metab20119671911193021646368
- Institute of MedicineDietary Reference Intakes for Calcium and Vitamin DWashington, DCThe National Academies Press2011
- MunnsCFShawNKielyMGlobal Consensus Recommendations on Prevention and Management of Nutritional RicketsJ Clin Endocrinol Metab2016101239441526745253
- HolickMFChenTCLuZSauterEVitamin D and skin physiology: a D-lightful storyJ Bone Miner Res200722Suppl 2V28V3318290718
- DawoduADavidsonBWooJGSun exposure and vitamin D supplementation in relation to vitamin D status of breastfeeding mothers and infants in the global exploration of human milk studyNutrients2015721081109325665158
- AndiranNYordamNOzonARisk factors for vitamin D deficiency in breast-fed newborns and their mothersNutrition2002181475011827764
- SethAMarwahaRKSinglaBVitamin D nutritional status of exclusively breast fed infants and their mothersJ Pediatr Endocrinol Metab200922324124619492580
- DawoduAAgarwalMHossainMKochiyilJZayedRHypovitaminosis D and vitamin D deficiency in exclusively breast-feeding infants and their mothers in summer: a justification for vitamin D supplementation of breast-feeding infantsJ Pediatr2003142216917312584539
- BikleDNonclassic actions of vitamin DJ Clin Endocrinol Metab2009941263418854395
- DawoduAAkinbiHVitamin D nutrition in pregnancy: current opinionInt J Womens Health2013533334323843706
- WagnerCLGreerFRPrevention of rickets and vitamin D deficiency in infants, children, and adolescentsPediatrics200812251142115218977996
- OberhelmanSSMeekinsMEFischerPRMaternal vitamin D supplementation to improve the vitamin D status of breast-fed infants: a randomized controlled trialMayo Clin Proc201388121378138724290111
- HollisBWWagnerCLHowardCRMaternal versus infant vitamin D supplementation during lactation: a randomized controlled trialPediatrics2015136462563426416936
