Abstract
Purpose
To determine the association of postpartum depression with domestic violence experiences among women in Asia.
Background
Postpartum depression (PPD) is an important cause of maternal morbidity as well as mortality. There is increasing evidence that domestic violence (DV) increases the risk of PPD.
Methods
We performed literature searches using the databases PUBMED, SCOPUS, Web of Science and Google Scholar, for studies published between January 2010 and May 2019. The keywords “postpartum”, “postnatal”, “depression”, and “violence” were used. Observational studies conducted within Asia, and written in the English language, were included.
Results
In the 38 studies included in this review (with 37,087 participants), the prevalence of PPD ranged between 8.2% to 70% and that of DV between 6.1% to 67.4%. There were 1.6 to 7.1 higher odds of PPD among sufferers of DV. Intimate partner violence (IPV) was the most relevant factor that women experiencing psychological abuse (which was the most prevalent form of IPV) were more at risk for, and violence/intimidation by other family members was also associated with PPD. Domestic violence increased the risk of suicidal ideation in PPD.
Discussion
The findings of the review unequivocally shows the association between domestic violence and PPD. Maternal mental health is a neglected area of healthcare in many parts of Asia. Likewise, domestic violence is a readily recognized, but inadequately addressed social issue. We recommend that healthcare workers be trained to recognize and support the women who are vulnerable to violence and depression during pregnancy and postpartum. Policies need to be developed at national and global levels to tackle these issues with utmost urgency.
Introduction
Postpartum depression (PPD) refers to depressive disorder occurring in the postpartum period. It is one of the most frequent complications during the post-partum period.Citation1 It has lasting effects on the mother, the child as well as the societal and marital relationship, which makes it a serious public health problem.Citation2 If left untreated, it may lead to dysfunctional mother-child interaction which contributes to problems like difficulty in breast feeding and failure to thrive.Citation3 It has also been shown to affect the cognitive development of the child, and leads to behavioral problems, disturbed sleep, and risk for anxiety and mental illness.Citation4 Postpartum depression can also have lasting effects on the mother’s mental health. Significant number of women who have PPD go on to develop recurrent long-term major depressive episodes in the future. In severe cases, the mother may commit suicide or cause harm to the child. There are social implications of this illness as well, such as social isolation of the mother, discord between partners, disruption of the family structure and lack of care for the newborn.Citation5–Citation7 Domestic violence (DV) refers to
Any act carried out with the intention of physically or emotionally harming another person who is related to you by blood; present or prior marriage or common law marriage. It includes hitting, shoving, kicking, biting, throwing body down, slapping, choking, using a weapon against; intimidation or threats; isolation, restricting or controlling activities; taking person's money, keeping them from getting or keeping a job, making them ask for money; forcing sexual activities without the will of the person.
The term “domestic violence” is used in many countries to refer to partner violence but the term can also encompass child or elder abuse, or abuse by any member of a household.Citation8
Intimate partner violence is one of the most prevalent forms of violence against women and includes physical, sexual, and emotional abuse as well as controlling actions by an intimate partner. It has been acknowledged as a violation of the basic human rights.Citation9 Abuse and neglect occurring in children less than 18 years old is known as Childhood Maltreatment (CM). It includes sexual abuse (Childhood Sexual Abuse or CSA), neglect, physical and emotional ill-treatment and commercial and other forms of exploitation, leading to either actual or potential harm to the child’s well-being.Citation10
There is increasing evidence that one important predictor of postpartum depression is women’s exposure to violence,Citation11–Citation17 with many literatures focused on PPD and partner victimization.Citation13,Citation14 Experiences of abuse and violence are particularly important during pregnancy and postpartum, a period when significant relations and personalities are being restructured.Citation18
The results of a meta-analysis study showed that women who had history of experiencing any form of violence events were at a higher risk of developing PPD compared with the reference group. Moreover, diverse kinds of violence such as sexual, emotional, and physical violence, as well as other forms of domestic or childhood violence also increased the risk of developing PPD.Citation19 Less well understood, however, is the relationship between postpartum depression and earlier experiences such as childhood maltreatment or abuse.Citation20,Citation21
The WHO multi-country study found prevalence of physical partner violence in pregnancy ranging from 1% in urban Japan to 28% in provincial Peru, with prevalence in most sites of 4–12%.Citation22 Similarly, a review which included research from 19 countries found prevalence ranging from 2% in settings such as Australia, Denmark and Cambodia, to 13.5% in Uganda, with the majority ranging between 4% and 9%.Citation23 A few facility-based studies in some settings have found even higher prevalence, including one from Egypt with an estimated prevalence of 32% and a review of studies from Africa that found a prevalence as high as 40% in some settings.Citation24,Citation25 Violence during pregnancy has been associated with miscarriage; late entry into prenatal care; stillbirth; premature labor and birth; fetal injury; and low-birth-weight or small-for-gestational-age infants. IPV may also account for a proportion of maternal mortality, although this association is often unrecognized by policymakers.Citation12,Citation26
Traumatic stress is thought to be the main mechanism that explains why partner violence may cause subsequent depression and suicide attempts. Exposure to traumatic events can lead to stress, fear and isolation, which, in turn, may lead to depression and suicidal behavior.Citation27 The findings of a study revealed that significant depressive symptomatology at 8 weeks postpartum is associated with childhood physical and sexual abuse.Citation28 Additionally, several studies have reported significant positive associations between childhood maltreatment and depression at some point in the postpartum period.Citation21,Citation29–Citation31 However, there is mixed reports as to the timing of PPD onset, depending on a history of childhood abuse. Lesser and Koniak in 2000, found childhood maltreatment to be predictive of early (4–6 weeks) but not later (6 or 12 months) depression,Citation32 while Minnes et. all in 2008, found that childhood maltreatment predicted later depression (6 or 12 months postpartum) but not in the immediate postpartum period. On the contrary, some studies have found no associations at all.Citation33
Postpartum depression as well as domestic violence both are issues extensively prevalent in Asia. While there have been several studies within Asia regarding the association of postpartum depression and domestic violence, there is a lack of a review that consolidates the findings of different countries and regions. This review aimed to study the prevalence of domestic violence and depression in various countries within Asia, to explore association between the two variables and to develop a complete picture of the issues in the context of Asia.
Methodology/Materials and Methods
Search Strategy and Search Terms
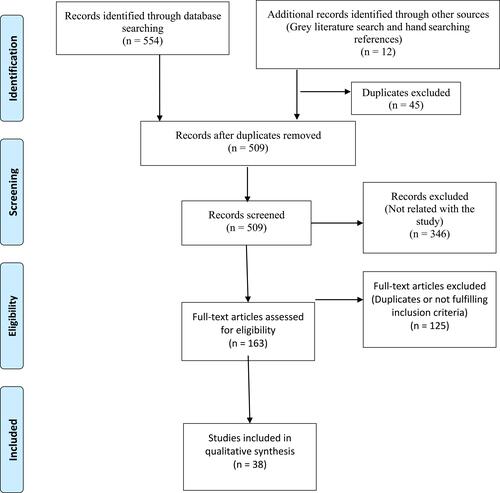
The review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for systematic review. PRISMA is the preferred minimum set of items to be reported in a systematic review, mostly applied for review of clinical trials but currently also used as a basis for review of other types of studies. Articles included in this review were identified through the following databases: PUBMED, SCOPUS, WEB OF SCIENCE and GOOGLE SCHOLAR. Original research articles published (or completed) between January 2010 to May 2019 were considered. The search terms used for the study have been listed in . The search terms were used in multiple combinations to identify the keywords as well as Mesh (Medical Subject Heading) specific for each database. The search was expanded and focused through Boolean Operators “OR” and “AND” respectively. Grey literature was searched in the databases Google Scholar, Scopus and Web of Science, as well as in the websites of key agencies (including WHO- SEARO, WHO- GMI and WHO- IRIS) and hand searching of references. The search terms are shown in .
Table 1 Search Terms
Selection Criteria
This review is a mixed-method review in which quantitative as well as qualitative articles were included. This was done in an effort to maximize the findings in the topic and make the results more relevant.Citation34 Articles were considered for inclusion in the review if they fulfilled the following criteria:
studies that included experience of lifetime domestic violence (Intimate Partner violence or childhood violence) as a predictor variable.
Studies that included postpartum depression as the outcome variable.
Studies conducted within Asia.
Studies written in the English language.
Observational study design.
Published/completed between January 2010 to May 2019.
Original research articles.
Exclusion Criteria: duplicates and unrelated studies were excluded.
Quality Assessment of Papers
Since the review included both qualitative and quantitative studies, predetermined criteria for quality assessment were developed based on existing tools and through consultation with experts. The quality of the paper was assessed based on the following characteristics: study setting, sample size, sampling technique, statistical methods and measurement tools of variables. An article was considered to have adequate quality if it fulfilled the following criteria:
conducted in community setting or hospital setting.
Fulfilled the minimum required sample size calculated for the study.
Probability sampling method used (in case of non-probability sampling, enough evidence provided to support the rationale behind it).
Measurement tools used for the variables were either:
standardized questionnaire that has been validated.
Self-developed questionnaire whose validity and reliability have been clearly mentioned and are adequate.
Data Extraction
Following the search of the databases, all the selected articles were downloaded into the reference manager software, EndNote v9. The downloaded titles and abstracts were initially checked for duplicates through the software and all recognized duplicate articles were removed. The studies that were obtained were initially screened through their titles. The study titles that explicitly included the study area as a region, country or city within Asia; as well as studies that did not mention the study area in the title were taken over to the next step of evaluation (abstract or full text). Studies that explicitly mentioned study area outside Asia, were excluded in the same round. The abstracts were then screened to exclude any studies not fulfilling the inclusion criteria (for example, study area, reference population, variables et cetera). In case of doubt about the inclusiveness, the paper was carried on to the next stage of screening. Full text of the remaining articles was obtained via Open Access journal or by borrowing from the University library. The full texts were extensively reviewed to ensure inclusion criteria and to exclude any more duplicates missed by the software. In the final stage, the quality of the included studies was assessed and the full text of the articles was analyzed to extract the following data: study design, number of participants included, country of study, prevalence of postpartum depression and domestic violence, type of violence, and the odds of domestic violence experience among sufferers of postpartum depression. Other studies have been reviewed and cited in the introduction as well as discussion, to have a better understanding of the subject as well as to interpret the results better. However, they have not been included in the systematic review. The selection flowchart has been illustrated in .
Results
The search strategy yielded 554 citations, of which 163 were assessed in the full-text form. Out of these, 38 studies were included in the review. There were 2 qualitative studies, 8 longitudinal and 28 cross-sectional studies. One study out of these was a thesis dissertation paper (which fulfilled the inclusion criteria and underwent the quality assessment). The included studies were from the following countries: Iran, Malaysia, Pakistan, Japan, Bangladesh, Nepal, Turkey, India, Vietnam, Israel, China, Thailand, Timor-Leste. Articles retrieved from each of the databases are shown in .
Table 2 Articles Retrieved from Each Database
The data extraction table () shows characteristics of studies included in the review and findings from all included studies.
Table 3 Data Extraction Table Showing the Characteristics and Findings of Studies Included
Results from Qualitative Studies
One study subcategorized “Domestic Violence” among postpartum women, using thematic analysis of in-depth interview. The study consisted of 21 women, all of whom screened positive for Postpartum Depression (EPDS score between 10–14). Most of these women admitted to having experienced domestic violence, either in the form of IPV or in the form of violence perpetrated by other family members. The violence occurred before, during pregnancy or after the birth of the child. They also expressed how the violence had led to constant fear during the period of postpartum. Another study consisting of 137 women found the prevalence of PPD to be 26.3%. The women who had experienced domestic violence during pregnancy or childbirth were found to have particularly higher risk for developing PPD.
Results from Cross-Sectional and Longitudinal Studies
The prevalence of PPD in the studies range between 8.2% (Japan) to 70% (Pakistan). Most of the studies (n= 31) have used the Edinburgh Postnatal Depression Scale (EPDS), which has been translated and validated in the respective languages. Two studies used Hospital Anxiety and Depression Scale (HADS) while 2 used Structured Clinical Interview for DSM-5 (SCID). One study each used the Beck’s Depression Inventory (BDI), Center for Epidemiological Studies–Depression scale and the 12 item Short Form Survey (SF-12). The prevalence of domestic violence ranged between 6.1 to 77.2% and was measured by Abuse Assessment Scale (AAS), Conflict Tactics Scale (CTS), WHO standard questionnaire, Index of Spousal Abuse (ISA), respective MoH violence questionnaire or proforma questionnaire (which were developed based on one or more of the standard questionnaires).
Out of the 38 studies, only 1 study found no association between DV and PPD while all the others found a significant association. For studies that expressed the association in Odds Ratio, it ranged between 1.6 to 7.1, while for the Relative Risk the range was between 1.6 and 3.3. The measures of association lied within the confidence interval for each of the studies.
Domestic Violence was found to have a clear association with Postpartum Depression and the most commonly studied DV in the studies was Intimate Partner Violence. Three studies measured Domestic Violence in general while two studies measured experiences of childhood violence (one in the form of Childhood maltreatment and the other in the form of Childhood Sexual Abuse). The remaining studies measured one or all forms of IPV. Among physical, emotional and sexual violence; emotional (psychological/verbal) form of abuse was found to be most prevalent. The prevalence ranged between 2.6% to 72.8%. Prevalence of psychological violence ranged between 3.7% to 82% and that of sexual violence ranged between 1.2% to 65%. Violence occurring during pregnancy was found by most studies to pose a higher risk for PPD. Likewise, psychological violence was the most prevalent as well as the highest risk-posing form of violence for PPD. Regarding Childhood Violence, both Childhood maltreatment and Childhood Sexual Abuse were found to be significantly associated with PPD.
The prevalence of various types of Domestic Violence; and the association with Postpartum Depression (expressed as the measure of association in separate articles) have been demonstrated in .
Table 4 Prevalence of Different Types of Domestic Violence and Association with Postpartum Depression
Discussion
Postpartum period is a time of rapid changes in the psychology as well as physiology of a mother. While on one hand she has to deal with added responsibility of the baby, on the other hand she has much to deal with regarding her own physical and emotional situation. Mothers are vulnerable to developing psychological disorders like Postpartum Blues and Postpartum Depression.
In the western part of the world, the prevalence of PPD in most studies has been shown to be between 10-20%.Citation71 However, various studies have noted that the prevalence of PPD is higher in the Lower- and Middle-Income Countries than in High or Higher Middle Income Countries.Citation72,Citation73 A review article regarding the prevalence of PPD in Asian women found the overall weighted prevalence to be about 28%.Citation74 In the context of South-Asia, studies from countries like India, Nepal and Pakistan have shown the prevalence to be between 19–36% in various studies.Citation70,Citation75–Citation78 Our current review found a similar prevalence of PPD, although the prevalence was found to be lower in studies conducted in Japan.
Postpartum depression is a complex issue in Asia because while in the Western culture women overtly express their changes in mood and depressive symptoms, in Asian cultures new mothers tend to manifest their emotional problems through somatic complaints.Citation79,Citation80 Studies have shown that many Asian cultures have an avoidance tendency toward accepting postpartum mental illness with an absence of reference to the disease entirely. For example, in countries like India, Philippines and Jordan, PPD is something people do not know and/or talk about.Citation81,Citation82 Cultural postpartum practices differ in Asia and other parts of the world. Many countries in Asia still follow the traditional practice of separating the mother from the rest of the family for a specified period of time considering her to be “dirty” or as a means to restore the yin and yang in her body. While on the one hand it provides physical rest to the mother, on the other it seriously hampers her psychological well-being. Likewise, Asian cultures still emphasize the gender of the newborn (most preferring boys over girls), which has been shown to be a risk factor for PPD among Asian women.Citation83–Citation85 Further, one review article showed that one of the factors contributing to PPD in Asian societies was that women cannot reject traditional rituals that are imposed on them by their caregivers during postpartum period.Citation86
The psychological burden of childbirth and child-rearing gets compounded in mothers who lack enough support from their partners. They become more prone to the postnatal psychological illnesses. In fact, if the mother has experienced Domestic Violence (particularly IPV), her risk of PPD gets multiplied several folds.Citation87 Our review showed that DV is significantly associated with PPD in almost all the studies included.
WHO found that globally 1 in 3 or 35%, of women have experienced some form of violence (ie physical and/or sexual violence) by an intimate partner.Citation27 Intimate partner violence (IPV) happens in any situation and among all socioeconomic, religious and cultural clusters of women. According to WHO, the prevalence estimates of intimate partner violence range from 23.2% in high-income countries and 24.6% in the WHO Western Pacific region to 37% in the WHO Eastern Mediterranean region, and 37.7% in the WHO South-East Asia region.Citation88 The highest prevalence of IPV has been found in Africa and South-East Asia. Along with high prevalence, there is also higher social acceptability toward violence inflicted by a partner in these regions.Citation26 Furthermore, studies in Asia have shown that men considered beating of wife by a husband to be a normal and accepted thing.Citation89 Similarly, experience of childhood maltreatment and abuse have been found to increase the risk of depression among postpartum women. Studies included in our review, which studied the association of CM/CSA and PPD, found significant association between the two. Traumatic stress experienced during domestic violence leads to fear and isolation, which, in turn, leads to depression.Citation27
The findings of this review unequivocally show an association between domestic violence and PPD. Maternal mental health is a neglected area of healthcare in many parts of Asia. Likewise, domestic violence is a readily recognized, but inadequately addressed social issue. Addressing the issue of Domestic Violence is especially challenging in the context of several countries in Asia because of the gender norms that influence marital violence, based on which violence inflicted by a husband is perceived as a normal and acceptable phenomenon.Citation90 A study conducted in Tibet showed that women justified being beaten by husband for making mistakes, and that violence was only considered unjustified if the husband inflicted it on the wife while she is working for the family. Violence in itself was considered a relatively acceptable matter.Citation91 Furthermore, it has been shown that women who have experienced violence in the household usually choose not to disclose it to or seek help from others. The National Family Health Survey in India (2014/2015) showed that only 14% of women who had ever experienced violence had sought help; among whom only 1% sought help from doctor or medical personnel.Citation9 This culture of keeping domestic violence behind hidden doors can contribute significantly to a rise in postpartum depression. Hence, it is important to understand the sensitivity of the issues of domestic violence and postpartum depression in the cultural context of Asian countries, and the vulnerabilities of women in this area.
Recommendations
We recommend that healthcare workers be trained to recognize and support the women who are vulnerable to violence and depression during pregnancy and postpartum.
Policies need to be developed at national and global levels to tackle these issues with utmost urgency. While developing policies, local cultural variations should be kept in mind and the option which addresses the issues in the most culturally acceptable way should be chosen.
Studies need to be conducted regarding the screening, diagnostic and intervention strategies most suited for vulnerable women.
Limitations
Our review does not include a meta-analysis, which would have provided additional strength to the findings of the review. The review includes studies from a limited number of countries; as a result of which the trend of domestic violence and postpartum depression as well as the challenges in these countries are not represented (further reviews with altered inclusion criteria, eg, wider timeframe, need to be conducted). Furthermore, the review is inherently prone to the bias present in the designs of studies included in the review.
Acknowledgment
The authors would like to thank Chulalongkorn University for supporting this study.
Disclosure
The authors report no conflicts of interest in this work.
References
- Guintivano J, Manuck T, Meltzer-Brody S. Predictors of postpartum depression: a comprehensive review of the last decade of evidence. Clin Obstet Gynecol. 2018;61(3):591–603. doi:10.1097/GRF.0000000000000368
- Jones I, Shakespeare J. Postnatal depression. BMJ. 2014;349:g4500. doi:10.1136/bmj.g4500
- Henderson JJ, Evans SF, Straton JA, Priest SR, Hagan R. Impact of postnatal depression on breastfeeding duration. Birth. 2003;30(3):175–180. doi:10.1046/j.1523-536X.2003.00242.x
- Kendall-Tackett KA. Depression in New Mothers: Causes, Consequences and Treatment Alternatives. Routledge; 2016.
- Meltzer-Brody S, Stuebe A. The long-term psychiatric and medical prognosis of perinatal mental illness. Best Pract Res Clin Obstet Gynaecol. 2014;28(1):49–60. doi:10.1016/j.bpobgyn.2013.08.009
- Stein A, Pearson RM, Goodman SH, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384(9956):1800–1819. doi:10.1016/S0140-6736(14)61277-0
- Sadock B, Ruiz P. Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences. Walters Kluwer; 2015.
- Heise L, Ellsberg M, Gottemoeller M. Ending violence against women. Popul Rep. 1999;27(4):1.
- Sciences IIfP ICF. National Family Health Survey (NFHS-4), 2015–16. India: IIPS Mumbai; 2017.
- Choi KW, Sikkema KJ. Childhood maltreatment and perinatal mood and anxiety disorders: a systematic review. Trauma Violence Abuse. 2016;17(5):427–453. doi:10.1177/1524838015584369
- Do HP, Tran BX, Nguyen CT, Vo TV, Baker PRA, Dunne MP. Inter-partner violence during pregnancy, maternal mental health and birth outcomes in Vietnam: a systematic review. Child Youth Serv Rev. 2019;96:255–265. doi:10.1016/j.childyouth.2018.11.039
- Abbaszadeh A, Kermani FP, Safizadeh H, Nakhee N. Violence during pregnancy and postpartum depression. Pak J Med Sci. 2011;27(1):177–181.
- Beydoun HA, Beydoun MA, Kaufman JS, Lo B, Zonderman AB. Intimate partner violence against adult women and its association with major depressive disorder, depressive symptoms and postpartum depression: a systematic review and meta-analysis. Soc Sci Med. 2012;75(6):959–975. doi:10.1016/j.socscimed.2012.04.025
- Howard LM, Oram S, Galley H, Trevillion K, Feder G. Domestic violence and perinatal mental disorders: a systematic review and meta-analysis. PLoS Med. 2013;10(5):e1001452. doi:10.1371/journal.pmed.1001452
- Krahé B. Violence against women. Curr Opin Cell Biol. 2018;19:6–10. doi:10.1016/j.copsyc.2017.03.017
- Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol. 2010;202(1):5–14. doi:10.1016/j.ajog.2009.09.007
- Lydsdottir LB, Howard LM, Olafsdottir H, Einarsson H, Steingrimsdottir T, Sigurdsson JF. Adverse life experiences and common mental health problems in pregnancy: a causal pathway analysis. Arch Womens Ment Health. 2019;22(1):75–83. doi:10.1007/s00737-018-0881-7
- Huth-Bocks AC, Krause K, Ahlfs-Dunn S, Gallagher E, Scott S. Relational trauma and posttraumatic stress symptoms among pregnant women. Psychodyn Psychiatry. 2013;41(2):277–301. doi:10.1521/pdps.2013.41.2.277
- Zhang S, Wang L, Yang T, et al. Maternal violence experiences and risk of postpartum depression: a meta-analysis of cohort studies. Eur Psychiatry. 2019;55:90–101. doi:10.1016/j.eurpsy.2018.10.005
- Carlson EB, Furby L, Armstrong J, Shlaes J. A conceptual framework for the long-term psychological effects of traumatic childhood abuse. Child Maltreat. 1997;2(3):272–295. doi:10.1177/1077559597002003009
- Li Y, Long Z, Cao D, Cao F. Maternal history of child maltreatment and maternal depression risk in the perinatal period: a longitudinal study. Child Abuse Negl. 2017;63:192–201. doi:10.1016/j.chiabu.2016.12.001
- García-Moreno C, Jansen H, Ellsberg M, Heise L, Watts C. WHO Multi-Country Study on Women’s Health and Domestic Violence Against Women. Vol. 204. Geneva: World Health Organization; 2005:1–18.
- Devries KM, Kishor S, Johnson H, et al. Intimate partner violence during pregnancy: analysis of prevalence data from 19 countries. Reprod Health Matters. 2010;18(36):158–170. doi:10.1016/S0968-8080(10)36533-5
- Campbell J, Garcia-Moreno C, Sharps P. Abuse during pregnancy in industrialized and developing countries. Violence Against Women. 2004;10(7):770–789. doi:10.1177/1077801204265551
- Shamu S, Abrahams N, Temmerman M, Musekiwa A, Zarowsky C. A systematic review of African studies on intimate partner violence against pregnant women: prevalence and risk factors. PLoS One. 2011;6(3):e17591. doi:10.1371/journal.pone.0017591
- Organization WH. Understanding and Addressing Violence Against Women: Intimate Partner Violence. World Health Organization; 2012.
- Organization WH. Global and Regional Estimates of Violence Against Women: Prevalence and Health Effects of Intimate Partner Violence and Non-Partner Sexual Violence. World Health Organization; 2013.
- Dennis C-L, Vigod S. The relationship between postpartum depression, domestic violence, childhood violence, and substance use: epidemiologic study of a large community sample. Violence Against Women. 2013;19(4):503–517. doi:10.1177/1077801213487057
- Muzik M, Marcus SM, Flynn H, Rosenblum KL. Depression during pregnancy: detection, comorbidity and treatment. Asia Pac Psychiatry. 2010;2(1):7–18. doi:10.1111/appy.2010.2.issue-1
- Dennis C-L, Coghlan M, Vigod S. Can we identify mothers at-risk for postpartum anxiety in the immediate postpartum period using the State-Trait Anxiety Inventory? J Affect Disord. 2013;150(3):1217–1220. doi:10.1016/j.jad.2013.05.049
- Meltzer-Brody S, Bledsoe-Mansori SE, Johnson N, et al. A prospective study of perinatal depression and trauma history in pregnant minority adolescents. Am J Obstet Gynecol. 2013;208(3):211. e1-. e7. doi:10.1016/j.ajog.2012.12.020
- Lesser J, Koniak-Griffin D. The impact of physical or sexual abuse on chronic depression in adolescent mothers. J Pediatr Nurs. 2000;15(6):378–387. doi:10.1053/jpdn.2000.16714
- Leigh B, Milgrom J. Risk factors for antenatal depression, postnatal depression and parenting stress. BMC Psychiatry. 2008;8(1):24. doi:10.1186/1471-244X-8-24
- Harden A. Mixed-methods systematic reviews: integrating quantitative and qualitative findings. Focus. 2010;2010(25):1–8.
- Afshari P, Tadayon M, Abedi P, Yazdizadeh S. Prevalence and related factors of postpartum depression among reproductive aged women in Ahvaz, Iran. Health Care Women Int. 2019;1–11. doi:10.1080/07399332.2019.1578779
- Ahmad NA, Silim UA, Rosman A, et al. Postnatal depression and intimate partner violence: a nationwide clinic-based cross-sectional study in Malaysia. BMJ Open. 2018;8:5. doi:10.1136/bmjopen-2017-020649
- Ahmadzad-Asl M, Davoudi F, Zarei N, Mohammad-Sadeghi H, Rasoulian M. Domestic violence against women as a risk factor for depressive and anxiety disorders: findings from domestic violence household survey in Tehran, Iran. Arch Womens Ment Health. 2016;19(5):861–869. doi:10.1007/s00737-016-0626-4
- Ali NS, Azam IS, Ali BS, Tabbusum G, Moin SS. Frequency and associated factors for anxiety and depression in pregnant women: a hospital-based cross-sectional study. Sci World J. 2012;2012:1–9. doi:10.1100/2012/653098
- Amemiya A, Fujiwara T. Association between maternal intimate partner violence victimization during pregnancy and maternal abusive behavior towards infants at 4 months of age in Japan. Child Abuse Negl. 2016;55:32–39. doi:10.1016/j.chiabu.2016.03.008
- Azad R, Fahmi R, Shrestha S, et al. Prevalence and risk factors of postpartum depression within one year after birth in urban slums of Dhaka, Bangladesh. PLoS One. 2019;14:5. doi:10.1371/journal.pone.0215735
- Bhusal BR, Bhandari N. Identifying the factors associated with depressive symptoms among postpartum mothers in Kathmandu, Nepal. Int J Nurs Sci. 2018;5(3):268–274. doi:10.1016/j.ijnss.2018.04.011
- Bulut SD, Alatas E, Gunay G, Bulut S. The relationship between postpartum depression and intimate partner violence. J Clin Anal Med. 2017;8(2):164–167. doi:10.4328/JCAM.4801
- Dubey C, Gupta N, Bhasin S, Muthal RA, Arora R. Prevalence and associated risk factors for postpartum depression in women attending a tertiary hospital, Delhi, India. Int J Social Psychiatry. 2012;58(6):577–580. doi:10.1177/0020764011415210
- Esie P, Osypuk TL, Schuler SR, Bates LM. Intimate partner violence and depression in rural Bangladesh: accounting for violence severity in a high prevalence setting. SSM Popul Health. 2019;7.
- Fisher J, Tran T, La BT, Kriitmaa K, Rosenthal D, Tran T. Common perinatal mental disorders in northern Viet Nam: community prevalence and health care use. Bull World Health Organ. 2010;88(10):737–745. doi:10.2471/BLT.09.067066
- Fishera J, Tran TD, Biggs B, Dang TH, Nguyen TT, Tran T. Intimate partner violence and perinatal common mental disorders among women in rural Vietnam. Int Health. 2013;5(1):29–37. doi:10.1093/inthealth/ihs012
- Islam MJ, Broidy L, Baird K, Mazerolle P. Intimate partner violence around the time of pregnancy and postpartum depression: the experience of women of Bangladesh. PLoS One. 2017;12(5):e0176211. doi:10.1371/journal.pone.0176211
- John VG. Predictors of Postpartum Depression Among Women in Karachi, Pakistan. 2017.
- Kabir ZN, Nasreen H-E EM. Intimate partner violence and its association with maternal depressive symptoms 6–8 months after childbirth in rural Bangladesh. Glob Health Action. 2014;7(1):24725. doi:10.3402/gha.v7.24725
- Khooharo Y, Majeed T, Das C, Majeed N, Majeed N, Choudhry AM. Associated risk factors for postpartum depression presenting at a teaching hospital. Ann King Edward Med Univ. 2010;16(2):87.
- Miura A, Fujiwara T. Intimate partner violence during pregnancy and postpartum depression in Japan: a cross-sectional study. Front Public Health. 2017;5. doi:10.3389/fpubh.2017.00081
- Murray L, Dunne MP, Van Vo T, Anh PNT, Khawaja NG, Cao TN. Postnatal depressive symptoms amongst women in Central Vietnam: a cross-sectional study investigating prevalence and associations with social, cultural and infant factors. BMC Pregnancy Childbirth. 2015;15:1. doi:10.1186/s12884-015-0662-5
- Patel HL, Ganjiwale JD, Nimbalkar AS, Vani SN, Vasa R, Nimbalkar SM. Characteristics of postpartum depression in Anand District, Gujarat, India. J Trop Pediatr. 2015;61(5):364–369. doi:10.1093/tropej/fmv046
- Shwartz N, Shoahm-Vardi I, Daoud N. Postpartum depression among Arab and Jewish women in Israel: ethnic inequalities and risk factors. Midwifery. 2019;70:54–63. doi:10.1016/j.midw.2018.12.011
- Tho Tran N, Nguyen HTT, Nguyen HD, et al. Emotional violence exerted by intimate partners and postnatal depressive symptoms among women in Vietnam: a prospective cohort study. PLoS One. 2018;13:11. doi:10.1371/journal.pone.0207108
- Zhang Y, Zou SH, Cao YP, Zhang YL. Relationship between domestic violence and postnatal depression among pregnant Chinese women. Int J Gynaecol Obstet. 2012;116(1):26–30. doi:10.1016/j.ijgo.2011.08.011
- Anjum F, Batool Z. An analytical study of contributory factors of postpartum depression among women in Punjab, Pakistan. RMJ. 2019;44(1):130–133.
- Kirkan TS, Aydin N, Yazici E, Aslan PA, Acemoglu H, Daloglu AG. The depression in women in pregnancy and postpartum period: a follow-up study. Int J Social Psychiatry. 2015;61(4):343–349. doi:10.1177/0020764014543713
- Poçan AG, Aki ÖE, Parlakgümüs AH, Gereklioglu Ç, Dolgun AB. The incidence of and risk factors for postpartum depression at an urban maternity clinic in Turkey. Int J Psychiatry Med. 2013;46(2):179–194. doi:10.2190/PM.46.2.e
- Saito A, Creedy D, Cooke M, Chaboyer W. Effect of intimate partner violence on postpartum women’s health in northeastern Thailand. Nurs Health Sci. 2012;14(3):345–351. doi:10.1111/nhs.2012.14.issue-3
- Silove D, Rees S, Tay AK, et al. Pathways to perinatal depressive symptoms after mass conflict in timor-leste: a modelling analysis using cross-sectional data. Lancet Psychiat. 2015;2(2):161–167. doi:10.1016/S2215-0366(14)00054-6
- Kita S, Haruna M, Matsuzaki M, Kamibeppu K. Associations between intimate partner violence (IPV) during pregnancy, mother-to-infant bonding failure, and postnatal depressive symptoms. Arch Womens Ment Health. 2016;19(4):623–634. doi:10.1007/s00737-016-0603-y
- Lev-Wiesel R, Daphna-Tekoah S. The role of peripartum dissociation as a predictor of posttraumatic stress symptoms following childbirth in Israeli Jewish women. J Trauma Dissociation. 2010;11(3):266–283. doi:10.1080/15299731003780887
- Nhi TT, Hanh NTT, Hinh ND, et al. Intimate partner violence among pregnant women and postpartum depression in vietnam: a longitudinal study. Biomed Res Int. 2019;2019.
- Turkcapar AF, Kadioğlu N, Aslan E, Tunc S, Zayifoğlu M, Mollamahmutoğlu L. Sociodemographic and clinical features of postpartum depression among Turkish women: a prospective study. BMC Pregnancy Childbirth. 2015;15:1. doi:10.1186/s12884-015-0532-1
- Nongrum R, Thomas E, Lionel J, Jacob KS. Domestic violence as a risk factor for maternal depression and neonatal outcomes: a hospital-based cohort study. Indian J Psychol Med. 2014;36(2):179–181. doi:10.4103/0253-7176.130989
- Budhathoki N, Dahal M, Bhusal S, Ojha H, Pandey S, Basnet S. Violence against women by their husband and postpartum depression. J Nepal Health Res Counc. 2012;10(22):176–180.
- Dolatian M, Hesami K, Shams J, Majd HA. Relationship between violence during pregnancy and postpartum depression. Iran Red Crescent Med J. 2010;12(4):377–383.
- Savarimuthu RJS, Ezhilarasu P, Charles H, Antonisamy B, Kurian S, Jacob KS. Post-partum depression in the community: a qualitative study from rural south India. Int J Social Psychiatry. 2010;56(1):94–102. doi:10.1177/0020764008097756
- Edhborg M, Nasreen HE, Kabir ZN. “I can’t stop worrying about everything”-experiences of rural Bangladeshi women during the first postpartum months. Int J Qual Stud Health Well-Being. 2015;10:26226. doi:10.3402/qhw.v10.26226
- Can P. Postpartum Disorders. 2013.
- Parsons CE, Young KS, Rochat TJ, Kringelbach M, Stein A. Postnatal depression and its effects on child development: a review of evidence from low-and middle-income countries. Br Med Bull. 2012;101:1. doi:10.1093/bmb/ldr047
- Shidhaye R, Mendenhall E, Sumathipala K, Sumathipala A, Patel V. Association of somatoform disorders with anxiety and depression in women in low and middle income countries: a systematic review. Int Rev Psychiatry. 2013;25(1):65–76. doi:10.3109/09540261.2012.748651
- Roomruangwong C, Epperson CN. Perinatal depression in Asian women: prevalence, associated factors, and cultural aspects. Asian Biomed. 2011;5(2):179–193. doi:10.5372/1905-7415.0502.024
- Husain N, Parveen A, Husain M, et al. Prevalence and psychosocial correlates of perinatal depression: a cohort study from urban Pakistan. Arch Womens Ment Health. 2011;14(5):395–403. doi:10.1007/s00737-011-0233-3
- Upadhyay RP, Chowdhury R, Salehi A, et al. Postpartum depression in India: a systematic review and meta-analysis. Bull World Health Organ. 2017;95(10):706. doi:10.2471/BLT.17.192237
- Khakurel G, Chalise P, Karki P. Prevalence and risk factors of postpartum depression in mothers attending child immunization clinic of a Teaching Hospital in Kathmandu. J Ins Med. 2018;42(1).
- Baron EC, Hanlon C, Mall S, et al. Maternal mental health in primary care in five low-and middle-income countries: a situational analysis. BMC Health Serv Res. 2016;16(1):53. doi:10.1186/s12913-016-1291-z
- Kim J, Buist A. Postnatal depression: a Korean perspective. Aust Psychiatry. 2005;13(1):68–71. doi:10.1080/j.1440-1665.2004.02153.x
- Evagorou O, Arvaniti A, Samakouri M. Cross-cultural approach of postpartum depression: manifestation, practices applied, risk factors and therapeutic interventions. Psychiatr Q. 2016;87(1):129–154. doi:10.1007/s11126-015-9367-1
- O’Mahony JM, Donnelly TT, Bouchal SR, Este D. Barriers and facilitators of social supports for immigrant and refugee women coping with postpartum depression. Adv Nur Sci. 2012;35(3):E42–E56. doi:10.1097/ANS.0b013e3182626137
- Nahas V, Amasheh N. Culture care meanings and experiences of postpartum depression among Jordanian Australian women: a transcultural study. J Transcult Nurs. 1999;10(1):37–45. doi:10.1177/104365969901000113
- Klainin P, Arthur DG. Postpartum depression in Asian cultures: a literature review. Int J Nurs Stud. 2009;46(10):1355–1373. doi:10.1016/j.ijnurstu.2009.02.012
- Saleh E-S, El-Bahei W, Del El-Hadidy MA, Zayed A. Predictors of postpartum depression in a sample of Egyptian women. Neuropsychiatr Dis Treat. 2013;9:15.
- Goldbort J. Transcultural analysis of postpartum depression. MCN Am J Matern Child Nurs. 2006;31(2):121–126.
- Abdollahi F, Lye M-S, Zain AM, Ghazali SS, Zarghami M. Postnatal depression and its associated factors in women from different cultures. Iran J Psychiatry Behav Sci. 2011;5(2):5.
- Chisholm CA, Bullock L, Ferguson IIJEJ. Intimate partner violence and pregnancy: epidemiology and impact. Am J Obstet Gynecol. 2017;217(2):141–144. doi:10.1016/j.ajog.2017.05.042
- Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts C. WHO Multi-Country Study on Women’s Health and Domestic Violence Against Women: Initial Results on Prevalence, Health Outcomes and Women’s Responses. Geneva: World Health Organization; 2005.
- Poudel-Tandukar K, Poudel KC, Yasuoka J, Eto T, Jimba M. Domestic violence against women in Nepal. Lancet. 2008;371(9625):1664. doi:10.1016/S0140-6736(08)60723-0
- Go VF, Johnson SC, Bentley ME, et al. Crossing the threshold: engendered definitions of socially acceptable domestic violence in Chennai, India. Cult Health Sex. 2003;5(5):393–408. doi:10.1080/136910501164119
- Rajan H. When wife-beating is not necessarily abuse: a feminist and cross-cultural analysis of the concept of abuse as expressed by Tibetan survivors of domestic violence. Violence Against Women. 2018;24(1):3–27. doi:10.1177/1077801216675742