Abstract
We report a case of a torted mature cystic teratoma in a 23-year-old, sexually inactive, virgin female which necessitated immediate laparoscopy. The patient and her family stressed that the integrity of the hymen must be maintained at any cost, for cultural reasons. We opted out of our routine intravaginal preparation for laparoscopic surgery to honor the patient’s request to maintain the integrity of the hymen. Left salpingo-oophorectomy was accomplished, and the specimen was removed using a large nephrectomy endobag. Here, we describe techniques that are useful for this procedure, including the use of gauze attached to ovum forceps to manipulate the uterus through the rectum, and a review of the literature.
Case report
A 23-year-old virgin female of Iraqi descent and Islamic faith presented at the Obstetrics and Gynecology Clinic, Meharry Medical College, Nashville, TN, in November 2010. Her chief complaint was a dull pain in the left lower abdominal/pelvic region. Her cycles were regular and average in amount with no complaints of menorrhagia or dysmenorrhea. Her last menstrual period had occurred 16 days earlier.
Her past medical history was noncontributory. She was generally healthy, had undergone no previous surgery, and had not suffered previously from abdominal or pelvic pain. She had reached menarche at the age of 14 years. The patient was accompanied by her mother who voiced that her daughter was still a virgin and because of their cultural values regarding virginity, any proposed management must preserve the integrity of her daughter’s hymen. The patient weighed 76 kg and was 167 cm in height, with a pulse rate of 82 beats/minute, temperature 98.1°F, blood pressure 100/68 mmHg. An abdominal examination showed a fullness/mass of the left hypochondrium and slight tenderness on palpation. No signs of peritoneal irritation were noted.
Sonography and computed tomography (CT) enabled us to diagnose the mass provisionally. An abdominal ultrasound revealed a cyst that most probably originated from the left ovary. This cyst was about 9 × 7.5 × 11 cm and showed variable echogenicity. A transvaginal ultrasound was declined because of the patient’s virginity. Neither ascites nor free abdominal fluid accumulations were noticed. CT revealed an 8.5 × 8 × 12 cm cystic mass originating from the left ovary. The cyst contained nondependent intracystic spheres of lipid material, favoring the diagnosis of a cystic teratoma. Laboratory results showed a normal full blood count, negative urinary beta human chorionic gonadotrophin, serum beta human chorionic gonadotrophin at 2.4 mIU/L (normal nonpregnant value < 3 mIU/L), and inhibin levels at 13.5 pg/mL (normal early luteal phase is 16–98 pg/mL).
The patient was then counseled and scheduled for a laparoscopic left ovarian cystectomy and a possible left salpingo-oophorectomy. Again, the patient and her family stressed that maintaining her virginity was a priority, even if that meant converting from laparoscopy to laparotomy. Two days later, while awaiting her elective surgical appointment, the patient called in about sudden onset of severe lower abdominal pain that had started 2–3 hours earlier. The patient was instructed to go to the emergency room immediately. Three hours later, the patient presented with acute abdomen, a temperature of 38°C, nausea, and vomiting. A full blood count and urine tests were within normal limits. Immediate surgery was planned to treat the suspected left adnexal torsion.
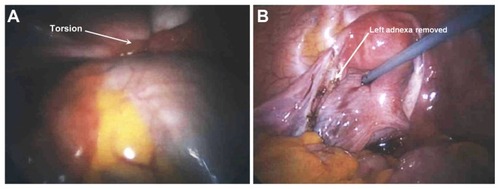
After general anesthesia was induced, we carefully and gently examined the patient’s vaginal area and found it to be almost completely sealed, with a microperforate hymen containing a hymenal opening that would not fit even one finger without disturbing the hymen. To fulfill the patient’s request to maintain her virginity, we asked the circulating nurse to be extra careful around the vulvar area and not to perform the routine intravaginal part of surgical preparation to avoid disturbing the hymen. We positioned the patient in the dorsal supine position instead of the typical dorsal lithotomy position for laparoscopy. After placing the trocars and panoramically viewing the abdominal cavity (), we used a 5 mm probe to stent and antivert the uterus, and we also used a self-locking atraumatic grasper to handle the uterus carefully as needed. We found a left ovarian cyst torted × 3 (, panel A). Because we lacked the option of a uterine manipulator, we raised the intra-abdominal pressure to 22 mmHg to generate additional room for intra-abdominal manipulation and then used a 5 mm laparoscopic uterine probe to manipulate the uterus during the procedure. After finding the right ovary and tube to be normal (, panel B), we untwisted the cyst and started to perform the cystectomy. However, we soon observed some hair and decided to proceed instead with a left salpingo-oophorectomy so as to avoid possible puncture of a dermoid cyst, which could cause chemical peritonitis and affect the patient’s future fertility potential. The left adnexa, which were about 11 × 13 cm upon intraoperative assessment (), did not fit into the normally available endobag, so we used a large nephrectomy bag to remove the specimen from the abdominal cavity. We used the nephrectomy bag through a 10 mm central port, and for visualization, we switched to a 5 mm laparoscope through one of the two 5 mm lateral ports. At the end of the procedure, we noticed that the patient was experiencing moderate bilateral periorbital air emphysema, and although periorbital edema is a rare observation with our surgical team, it likely to have been caused by a combination of relatively high intra-abdominal pressure and a steep Trendelenburg position. However, the periorbital emphysema resolved spontaneously over the next few hours. The patient was kept under observation for 23 hours and then discharged in excellent condition.
Figure 1 Panoramic view of the abdominal cavity. Left dermoid cyst torted × 3 (panel A). A view of the pelvis after removal of the left adnexa (panel B). The right adnexa appear normal.
Her postoperative course was uneventful. The gross pathology evaluation of the cyst revealed a 9 × 8 × 12.5 cm cyst containing hair, fat globules, and three teeth. The ovary also measured approximately 6 × 4 × 2 cm in its largest dimensions, with smaller cystic lesions. The microscopic examination confirmed a diagnosis of benign teratoma (dermoid cyst).
Discussion
Ovarian teratoma occurs in a wide range of ages, with a peak during the reproductive years.Citation1 It is considered to be the most common ovarian neoplasm in both pediatric and adult populations,Citation2 in the first two decades of life, and accounts for more than two-thirds of benign ovarian neoplasms.Citation3,Citation4 Among 118 cases with ovarian teratoma, 85.6% were found to be younger than 40 years.Citation5 Another study based on a cohort of 112 patients with mature ovarian teratoma found that the surgeries performed for these patients ranged from unilateral oophorectomy to total hysterectomy with bilateral oophorectomy, and within this group of patients, ovarian function was preserved in 75% of the patients.Citation6
Laparoscopic surgery in adult virgin women is not common in Western communities and is extremely underreported in the medical literature. Intra-abdominal pressure is referred to in the literature as a safe measure to overcome entry-related complications,Citation7 and some reports indicate that an increase in intra-abdominal pressure of over 20 mmHg for a period of 5 minutes is associated with changes in heart rate, mean arterial blood pressure, arterial oxygen saturation, and intratracheal pressure that are still within the normal range.Citation8 Other reports advocate the use of higher intra-abdominal pressure for additional safety to protect against organ injury because there are no changes in cardiovascular parameters between 15 mmHg and 30 mmHg.Citation9 In our case, we found that elevating intra-abdominal pressure to a level of 22 mmHg throughout the procedure was not only a safe measure to avoid entry-related complications but was also a very helpful maneuver to provide additional room to facilitate dealing with the large adnexal lesion laparoscopically in the absence of the intravaginal uterine manipulator (due to the need to preserve virginity).
Other approaches may also be considered. A personal communication with colleagues in the Middle East (where laparoscopic interventions in virgin patients are not uncommon) suggested using gauze attached to ovum forceps to manipulate the uterus via the rectum and may be considered as an alternative technique in such cases.
Laparoscopy is generally a safe procedure, but not free from the complications encountered in 0.1%–10% of cases.Citation10 These side effects range from entry injury through to some major side effects, including visceral injury and injury to major blood vessels. Our surgical team followed a combination of increased intra-abdominal pressure and careful intra-abdominal manipulation in addition to the Trendelenburg position to reduce these possible side effects. To our knowledge and based on a Medline search using the keywords “virgin”, “ovarian teratoma”, and laparoscopy, there has not been a publication describing the use of laparoscopic intervention for teratoma in virgin patients. Therefore, we feel that our report provides a useful insight in regard to such cases.
Conclusion
Teratomas in virgin adolescent patients are relatively common, and with globalization, intercultural communication and the trend for immigration from the Middle East to western countries, encountering such cases will become more common for surgeons. Enhancing the knowledge about how to address the cultural needs of such patients is an important part of providing a comprehensive clinical service to an increasingly diverse patient population.
Disclosure
The authors report no conflicts of interest in this work.
References
- SelvaggiSMTumors of the ovary, maldeveloped gonads, fallopian tube, and broad ligamentArch Pathol Lab Med2000124347710705419
- SavasiILacyJAGerstleJTStephensDKivesSAllenLManagement of ovarian dermoid cysts in the pediatric and adolescent populationJ Pediatr Adolesc Gynecol200922636036419589709
- BerekJSNatarajanSOvarian and fallopian tube cancerBerekJSBerek and Novak’s Gynecology14th edPhiladelphia, PALippincott Williams and Wilkins2007
- AzizkhanRGCatyMGTeratomas in childhoodCurr Opin Pediatr1996832872928814409
- LakkisWGMartinMCGelfandMMBenign cystic teratoma of the ovary: a 6-year reviewCan J Surg19852854444464027793
- Morillo ConejoMMartin CanadasFMunoz CarmonaVOvarian mature teratoma. Clinico-pathological study of 112 cases and review of the literatureGinecol Obstet Mex200371447454 Spanish14686056
- The ABCs of a safer laparoscopic entryJ Minim Invasive Gynecol200613324925116698536
- HypolitoOHAzevedoJLde Lima Alvarenga CaldeiraFMCreation of pneumoperitoneum: noninvasive monitoring of clinical effects of elevated intraperitoneal pressure for the insertion of the first trocarSurg Endosc20102471663166920035347
- VilosGAVilosAGAbu-RafeaBHollett-CainesJNikkhah-AbyanehZEdrisFThree simple steps during closed laparoscopic entry may minimize major injuriesSurg Endosc200923475876418626703
- ChandlerJGCorsonSLWayLWThree spectra of laparoscopic entry access injuriesJ Am Coll Surg2001192447849011294405