Abstract
Purpose
Early-stage cervical cancer is usually diagnosed by colposcopy-directed biopsy (CDB) and/or endocervical curettage (ECC), but some neglected lesions must be detected by conization because they are occult. This study aimed to explore the optimal method for detecting these “occult” cervical cancers.
Patients and Methods
A total of 1299 patients who were high-risk for early-stage cervical cancer from five centres in China were prospectively included. We evaluated the diagnostic performance of cytology, HPV testing, colposcopy and CDB&ECC for detecting “occult” cervical cancer and discussed the diagnostic importance of transformation zone (TZ) type, conization length and the proportion of cervical cone excision.
Results
The diagnostic agreement between colposcopy impression and conization was 64.5% and 72.4% between CDB&ECC and conization. Forty-two patients were finally diagnosed with pathologic cancer, and the sensitivities of cytology, colposcopy, CDB&ECC were 4.8%, 7.1%, and 47.4%, respectively. Twenty cases were neglected by CDB&ECC but further diagnosed as cancer by conization, considered to be occult cervical cancer, accounting for 1.6%. Cytologic high-grade squamous intraepithelial lesion (HSIL)+, positive HPV, biopsy HSIL+ and cervical TZ type 3 were considered risk factors for developing HSIL+, while colposcopy impression HSIL+ was not. There was a significant difference between cancerous and HSIL patients in the proportion of cervical cone excision (P<0.001), which was recognized as a risk factor (P<0.001) for detecting cancer, while the length of cervical cone excision was not. The average proportion was 0.62, and the minimal effective proportion was 0.56.
Conclusion
Since the incidence of occult cervical cancer neglected by CDB&ECC, colposcopy and cytology was far beyond expectations, conization is necessary, especially in patients with TZ type 3, high-grade cytology and biopsy results. As the cervical length varies in patients, the proportion of cervical cone excision might be a better indicator for detecting occult cervical cancer.
Highlights/Plain Language Summary
The incidence of neglected early-stage cervical cancer is far beyond expectations.
Conization is necessary for detecting occult cervical cancer, especially for a smooth cervix, and the colposcopy impression does not seem to be reliable.
A minimal proportion of cervical cone excision is proposed rather than a uniform length.
Introduction
Cervical cancer has high morbidity and mortality worldwide, and it accounted for an estimated 570,000 new cancer cases and 311,000 deaths worldwide in 2018.Citation1 Occult cervical cancer is mostly recognized as cervical cancer diagnosed by histopathology after a simple hysterectomy for a benign indication, which indicates that invasive cancer is not suspected before surgery.Citation2,Citation3 Recently, Pretorius et al defined “occult cervical cancer” as invasive cancer diagnosed by conization or hysterectomy but with neither cervical biopsy nor ECC histopathology showing invasive cancer.Citation4 The 5-year survival rate of “occult” cervical cancer patients is less than 50% if they do not receive any proper treatment; therefore, it is urgent and crucial to detect cervical cancer in a very early stage.Citation5
Early detection of cervical cancer comprises cervical cytology and HPV testing, colposcopy impression, and CDB&ECC, which refers to the “three-step” screening process. However, several studies have shown that the diagnostic performance of CDB&ECC for detecting early-stage cervical cancer is far from satisfactory. Some underdiagnosed lesions were further diagnosed as invasive cancer by conization, which were occult and easy to miss.Citation6,Citation7 Diagnostic cervical conization requires omnidirectional cervical sampling, which can greatly improve the early diagnostic rate of early-stage invasive cervical cancer and identify occult cervical cancer.
To date, the reported incidence of occult cervical cancer varies in publications, among which the most recent large-scale study reported an incidence of 0.31%.Citation4,Citation8–Citation10 Few studies have reported the risk factors for occult cervical cancer. Three types of cervical cone excision treatment were described with dimensions to designate thickness, length, and circumference in the International Federation of Cervical Pathology and Colposcopy (IFCPC) nomenclature; however, there is no consensus about the optimal conization size for detecting occult cervical cancer.Citation11
In this study, we analysed the clinical data of women who were at high-risk for early-stage cervical cancer from a multicentre study in China and discussed the optimal approach and correlative factors in detecting “occult” cervical cancer.
Patients and Methods
Patient Selection
A multicentre study was performed in five clinical centres, including the Obstetrics and Gynecology Hospital of Fudan University, Renji Hospital of Shanghai Jiao Tong University School of Medicine, Shanghai First Maternity and Infant Hospital of Tongji University, Shanghai Cancer Hospital of Fudan University, and Tongji Hospital of Tongji University, during the period from July 2016 to September 2019.
Women who were at high risk for early-stage cervical cancer were prospectively enrolled in this study. The inclusion criteria were: 1) patients with cytology results as atypical squamous cells, cannot exclude HSIL (ASC-H)/HSIL (no HPV testing required) regardless of the histopathology results from colposcopy biopsy; or 2) patients with CDB&ECC histopathology as HSIL regardless of the cytology or colposcopy results; or 3) HPV16/18 positive patients; or 4) patients with cytology results as atypical squamous cells of undetermined significance (ASC-US)/atypical glandular cells (AGC) with a positive HPV test; or 5) patients with cytology results as low-grade squamous intraepithelial lesion (LSIL) (no HPV testing required); or 6) patients with a colposcopy impression as HSIL with CDB&ECC histopathology as LSIL. The exclusion criteria were as follows: 1) women who were pregnant; 2) patients with acute inflammation of the pelvis and lower genital tract; or 3) patients with other severe diseases. The inclusion and exclusion criteria were strictly applied while enrolling the clinical cases. All patients were fully informed about the procedure and the aim of this study. Signed informed consent for study participation was collected before the colposcopy, and institutional review board approval was obtained. During the study period, all patients who met the inclusion and exclusion criteria were asked their intention to participate in the study. The participants could withdraw at any time, and they were free to engage in HPV testing and TCT cytology during the follow-up. This study was conducted in accordance with the Declaration of Helsinki.
Data Collection
A total of 1324 clinical cases from five research centres were enrolled in the study, and all enrolled patients were followed up at 6-month intervals until a clinical decision on whether to perform conization was made and the histopathology of the conization was recorded. Up to August 31, 2019, a total of 1299 patients completed all follow-up visits, and their clinical data were integrated. Clinical characteristics, cervical cytology, HPV testing, comprehensive colposcopy impression, histopathological results of CDB&ECC, and cervical conization of these patients were recorded. The histopathology result of the conization was recognized as the “gold standard”.
Cytology was tested by the ThinPrep cytologic test (TCT) or the liquid-based cytology test (LCT). HPV testing and typing were performed by the Cobas 4800 HPV test (Roche Molecular Systems, Pleasanton, California), Aptima HPV assay (Hologic Gen-Probe, San Diego, California), Hybrid Capture II (Qiagen, Gaithersburg, MD, USA), or HPV Genotyping Real-Time PCR Kit (Jiangsu Bioperfectus Technologies, Jiangsu, China). Colposcopy was performed by 10 experienced colposcopists who had at least 5 years of experience with the 2011 IFCPC colposcopy terminology. A Leisegang BG/LED Y/C optoelectronic integrated digital colposcopy system (Leisegang Feinmechanik Optik GmbH, Berlin, Germany) was used to evaluate the cervical lesions; images were obtained by an optical camera (Canon EOS600D). All colposcopies were performed according to a standard protocol, including the application of 5% acetic solution, Lugol’s iodine solution for the Schiller test, and punch biopsies of suspicious sites. ECC was performed when (1) the entire squamocolumnar junction and the margins of any visible lesion were not visible under the colposcope; (2) high-grade cervical cytology (ASC-H, HSIL, cancer, AGC, AIS) was present.
Transvaginal ultrasound was applied to measure the length of the cervix before conization. Conization was performed on the principle of IFCPC guidance, and different diathermy loops were used depending on the size of the cervical lesions and the location of the transformation zone. Taking into account a short cervix length and fertility preferences, individual adjustments were implemented in some patients. The length of the cervical cone excision was finally measured and reported by pathologists. The length proportion of the cervical cone excision was defined as the length of the cervical cone excision/the full length of the cervix. Each cone tissue was cut into 12 pieces, embedded into a paraffin block, and processed by a standardized protocol. The histopathology results were interpreted and verified by 2 experienced pathologists. Cervical cancer staging in this study was based on the International Federation of Gynecology and Obstetrics (FIGO) 2018.
Statistical Analysis
All data were analysed by SPSS 20.0 statistical software, and chi-square analysis was applied to analyse the difference between the average value and percentage. The Mann–Whitney test was applied to analyse the difference between the median value and distribution. Sensitivity, specificity, Youden index, and Cohen’s kappa (κ) coefficient were applied to evaluate the diagnostic consistency between different screening methods and conization. Binary logistic regression was applied to explore the risk factors for cervical lesions. P <0.05 was considered statistically significant.
Results
Clinical Characteristics of the Patients
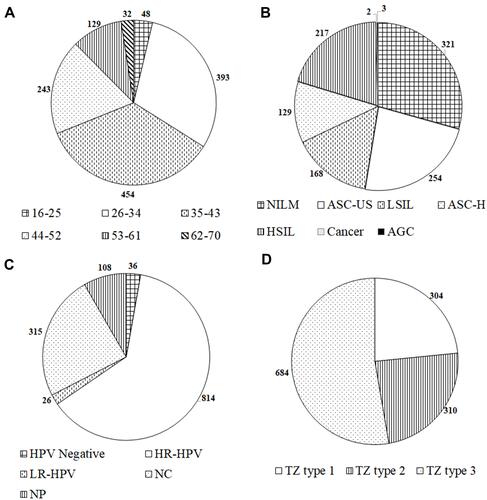
All 1299 patients who were at high risk for early-stage cervical cancer completed follow-up visits and received conization with exact histopathology results. illustrates the clinical characteristics of the patients. The mean age of these patients was 39.6±9.8 years (range 16–69 years), 32.0% (393/1299) of them were 26–34 years old, 36.9% (454/1299) of them were 35–43 years old, and 20.0% (243/1299) of them were 44–52 years old. Among them, 1094 patients had cytology results, 29.4% (321/1094) were cytology negative for intraepithelial lesion or malignancy (NILM), 23.2% (254/1094) were cytology ASC-US, 15.4% (168/1094) were cytology LSIL and 32.1% (351/1094) had high-grade cytology (ASC-H, HSIL, cancer, AGC). A total of 1191 patients received HPV testing, 97.0% (1155/1191) of whom were HPV positive. In addition, 68.4% (814/1191) of them were high-risk HPV (HR-HPV) positive, nearly half (50.6%) of which were HPV16 positive. A total of 1298 patients underwent colposcopy assessment of the transformation zone (TZ), 23.4% (304/1298) of whom were TZ type 1, 23.9% (310/1298) of whom were TZ type 2, and 52.7% (684/1298) of whom were TZ type 3.
Figure 1 Clinical characteristics of the enrolled patients. (A) Age distribution. (B) Cytology result. (C) HPV infection status. (D) Distribution of transformation zone type.
Diagnostic Performance of the Screening Procedure in Detecting Cervical Cancer
The diagnostic agreement between the colposcopy impression and the conization histopathological diagnosis was 64.5% (837/1298). In this research, 96.9% (31/32) of cervical cancers were missed by colposcopy impressions, including lesions staged IA1, IA2, and IB1. The diagnostic agreement between the histopathology of CDB&ECC and conization was 72.4% (890/1229). The sensitivity and specificity of CDB&ECC for detecting cervical cancer diagnosed by conization were 31.0% (9/29) and 99.3% (1191/1200), respectively. McNemar’s chi test showed consistency between CDB&ECC and conization (P=0.061). The Cohen’s κ coefficient was 0.372 (P<0.001). The detailed information is tabulated in .
Table 1 Correlation Between Colposcopy Impression, CDB&ECC and Conization
Considering that CDB&ECC-diagnosed cervical cancer might not be detected by conization as the lesion has been removed by the punch biopsy, we recognized either CDB&ECC- or conization histopathology-diagnosed cancer as pathologic cervical cancer. In our study, the number of pathologic cervical cancer patients was 42. These patients were all positive for HPV, and 73.8% (31/42) of them were HR-HPV infected. The diagnostic performances of cytology under different criteria are shown in . The sensitivity and specificity of cytology ACS-H+ were 45.2% (19/42) and 68.4% (720/1052) for detecting pathologic cervical cancer, respectively. It had the highest Youden index of 0.137 among the different cytology diagnostic criteria. The sensitivity and specificity of cytology cancer were 4.8% (2/42) and 99.7% (1049/1052), respectively. It had the highest Cohen’s κ coefficient of 0.078 with histopathology results among the different cytology diagnostic criteria (P=0.014). Two patients did not receive colposcopy, and the sensitivity and specificity of the colposcopy impression as cancer were 7.1% (3/42) and 96.8% (1256/1298) for detecting pathologic cervical cancer, respectively. A total of 38 pathologic cervical cancer patients underwent CDB&ECC, and its sensitivity was 47.4% (18/38). In microinvasive (staged IA1 and IA2) pathologic cervical cancer, the sensitivity of CDB&ECC was 48.6% (17/35), and 33.33% (1/3) of stage IB1 pathologic cervical cancer patients were detected by CDB&ECC.
Table 2 Diagnostic Value of Cytology Under Different Criteria in Detecting Pathologic Cervical Cancer
Analysis of Screening Results for Occult Cervical Cancer
We considered the lesions that were diagnosed as pathologic cervical cancer but missed by CDB&ECC as “occult” cervical cancer, whose rate was 52.6% (20/38), accounting for 1.6% (20/1229) among all patients who underwent CDB&ECC. Similarly, the lesions that were diagnosed as pathologic HSIL but were underdiagnosed by CDB&ECC were “occult” HSIL, whose rate was 7.5% (86/1141) among pathologic HSIL and accounted for 7.0% (86/1229) of all patients who received CDB&ECC.
In total, 20 patients were recognized as having occult cervical cancer in our research (). Eighteen patients were staged IA1 and 2 were staged IB1 by the histopathology results of conization. In terms of cytology, 50% (10/20) of patients had low-grade cytology results (NILM, ASC-US, LSIL), and 50% (10/20) of patients had high-grade cytology results (ASC-H, HSIL, cancer). All occult cervical cancer patients were HPV positive, 95.0% (19/20) of them were HR-HPV infected, 9 patients were HPV 16 positive, and only one was low-risk HPV (LR-HPV) positive, for HPV 28. A total of 80.0% (16/20) of patients had a colposcopy impression of HSIL, 2 patients had a colposcopy impression of cancer, and the remaining 2 patients had LSIL. The CDB&ECC histopathology results of these occult cervical cancer patients were all HSIL.
Table 3 Detailed Results of the “Three-Step” Screening Procedure of Occult Cervical Cancer Patients
Identifying Risk Factors for HSIL+ and Cancer Patients Based on the Regression Model
Binary logistic regression was applied to clarify risk factors for the HSIL+ and cervical cancer patients. According to reports from the previous literature, we included cytology, HPV, colposcopy impression, CDB&ECC, and TZ type in the model.
The logistic regression results showed that cytology HSIL+, HPV positivity, CDB&ECC HSIL+ and TZ type 3 were risk factors for HSIL+. The odds ratios (ORs) of cytology HSIL+, HPV positive, CDB&ECC HSIL+ and TZ type 3 were 1.615 (95% CI: 1.004–2.597), 2.575 (95% CI: 1.164–5.699), 2.572 (95% CI: 1.709–3.871) and 1.526 (95% CI: 1.046–2.225), respectively. Cytology ASC-US, LSIL, ASC-H, colposcopy impression, and TZ type 2 were not recognized as risk factors for HSIL+ in the logistic regression model (P>0.05). illustrates the results of the logistic regression in predicting HSIL+.
Figure 2 Binary logistic regression results to identify risk factors for HSIL+ patients.
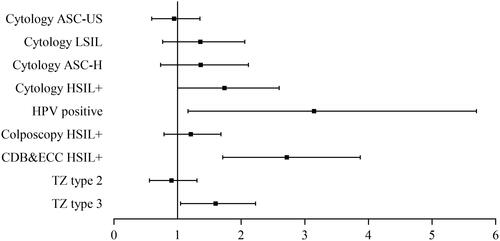
Likewise, in terms of early-stage cervical cancer, the same factors, including cytology, HPV, colposcopy impression, CDB&ECC, and transformation zone type, were also analysed by logistic regression. However, none of these factors were significant for predicting cervical cancer (P>0.05).
Analysis of Transformation Zone Type and Conization Length
In our study, the proportion of cervical TZ type 1 decreased with the upgrading severity of the cervical lesions. The proportions of TZ type 1 in normal/inflammatory, LSIL and HSIL+ patients were 28.9% (33/114), 26.3% (42/160) and 22.4% (229/1024), respectively. A total of 20.0% (4/20) of occult cervical cancer patients were TZ type 1. Among patients with different grade lesions, the proportion of TZ type 2 was the highest in LSIL patients, which was 34.4% (63/160). The proportion of cervical TZ type 3 increased with increasing severity of cervical lesions from LSIL to early-stage cervical cancer. A total of 69.0% (29/42) of early-stage cancer patients were TZ type 3, and 54.4% (534/982) of HSIL patients were TZ type 3. A total of 75.0% (15/20) of occult cervical cancer patients were TZ type 3, which was the highest among all cervical lesions. The findings above are shown in in detail.
Figure 3 (A) Distribution of the transformation zone in patients with different grades of cervical lesions. (B) Difference in length proportion of cervical cone excision between cervical cancer patients and HSIL patients. *Significant difference between two groups (P < 0.05). (C) ROC curve of the length proportion of cervical cone excision in detecting cervical cancer.
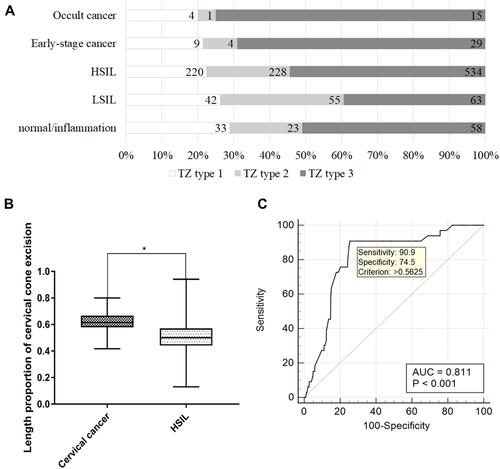
The range of conization length with the detection of cervical cancer and HSIL was 0.7–2.1 cm and 0.2–2.5 cm, respectively. The difference in the length of the cervical cone excision was not significant between cervical cancer and HSIL patients (P=0.207), whose mean length was 1.106±0.081 cm in cancer patients and 1.209±0.015 cm in HSIL patients. However, the difference in the length proportion of cervical cone excision was significant between cancer and HSIL patients (P<0.001), whose mean proportion was 0.619±0.014 in cancer patients and 0.504±0.004 in HSIL patients (). Binary logistic regression revealed that the proportion of cervical cone excision length was a risk factor for cervical cancer (P<0.001), while the cervical cone excision length was not. The ROC curve showed that a length proportion of cervical cone excision >0.563 was associated with detecting cervical cancer, with a sensitivity and specificity of 90.91% and 74.52%, respectively ().
Discussion
In this large-scale multicentre study, we identified 20 early-stage cervical cancer patients (stage IA1-IB1) who were missed by CDB&ECC before conization among 1299 patients who were high-risk for early-stage cervical cancer and received CDB&ECC. We analysed the screening features of “occult” cervical cancer patients, discussed risk factors for patients with HSIL+ and cervical cancer, and evaluated the importance of transformation zone (TZ) type, length and length proportion of cervical cone excision.
With the development of colposcopy, the diagnostic value of CDB&ECC has been improved, but misdiagnosis still occurs. The diagnostic discrepancy between CDB&ECC and conization has been reported in previous studies, reporting an underdiagnosis rate ranging from 6.4% to 23.1%.Citation7,Citation12–Citation19 The diagnostic agreement between CDB&ECC and conization was 43–85.8% according to those studies, and our study reported a relatively high concordance rate, 72.4%. As the last step of the “three-step” screening procedure, CDB&ECC is the most convincing procedure before diagnostic conization.
The possibility of fertility preservation in early-stage cervical cancer patients requires early diagnosis and timely treatment. In this study, 42 patients with early-stage cervical cancer were identified by conization or CDB&ECC, most of whom had microinvasive cancer, including FIGO stage IA1 and IA2 lesions. Excluding 4 patients who did not undergo CDB&ECC and received diagnostic conization directly, 47.4% of early-stage cervical cancers were distinguished by CDB&ECC, which was higher than the previously reported 18.0–25.0%.Citation20,Citation21 In our study, the sensitivity of CDB&ECC for detecting microinvasive cancer was 48.6%, which was higher than previous results from monocentre studies, ranging from 4.4%-33.3%.Citation21–Citation27 These findings suggest that gynaecologists have increased awareness of microinvasive cancer, and more cervical cancer patients are being diagnosed and receiving appropriate treatment in the early stage. A total of 45.2% of early-stage cervical cancer patients had high-grade cytology, which coincided with the reported rate of 42.1% in Slovenia.Citation28 The incidence of cervical cancer increased with the upgrading of cytology and was 3.1% and 5.4% in patients with low-grade and high-grade cytology, respectively, consistent with previously reported rates.Citation7,Citation29–Citation31 However, 50.0% of early-stage cervical cancer was cytologic NILM/ASC-US in our study, which implied that the diagnostic performance of cytology was not satisfactory. The Slovenian study further indicated that underdiagnosed smears were not related to FIGO stage.Citation28 A study in China pointed out that colposcopic impression often resulted in underdiagnosis of cervical cancer with an underestimated rate of 70.7%,Citation32 but this was much higher in our study (92.9%).
For occult cervical cancer, most gynaecologists have focused on accidentally diagnosed cancer by histopathology after hysterectomy, and only a few monocentre studies about conization pathologic cancer missed by CDB&ECC have been reported.Citation4,Citation8 Through a multicentre clinical study, we expanded the sample volume prospectively and identified 20 patients with occult cervical cancer. Despite increased attention and fewer missed diagnoses, the incidence of occult cervical cancer was still well beyond our expectations and it clearly requires increased attention in clinical practice, since it was 1.6% of all patients who underwent CDB&ECC. A total of 95.0% of occult cervical patients were HR-HPV positive, and 50.0% of patients had high-grade cytology, which was parallel to previous data of 96.4% and 56.8% in our clinical centre.Citation8 This finding implies that the sensitivity of HR-HPV testing was higher than that of high-grade cytology. Interestingly, an LR-HPV-infected patient with occult cervical cancer who was HPV28 positive was found in our study.
In our study, 10% of occult cervical cancer was diagnosed by colposcopy impression, which was higher than the previous rate of 3.5%.Citation4 The proportion of CDB&ECC HSIL in all occult cancer patients was 100.0% in our study, compared to 95.0% in the previous study conducted in our clinical centre and 78.9% in Pretorius’s study.Citation4,Citation8 Similar to Pretorius’s study,Citation4 1.9% of CDB&ECC HSIL patients were further diagnosed with occult cervical cancer. These findings indicate that attention should be given to patients with high-grade cytology, HR-HPV positivity, HSIL+ colposcopy impression and CDB&ECC results, since they may need to receive diagnostic cervical conization to exclude cancer. As the epidemiology shows, after early interventions for occult cervical cancer, the 5-year survival rate is 98%, and the 10-year survival rate is 70%.Citation33
Our study also paid attention to HSIL that CDB&ECC failed to detect, and the under-diagnosed rate was 7.5% in pathologic HSIL, basically coinciding with another study in China, which presented an under-diagnosed rate as 5.8% and revealed that irregular vaginal bleeding, CDB&ECC HSIL, and multiple biopsies were independent risk factors for under-diagnosis of HSIL.Citation34 Previous studies revealed that women with HSIL cytology, HPV16/18-positive, and high-grade colposcopic impressions were at high risk of HSIL.Citation35 We applied binary logistic regression to identify the risk factors for HSIL+ patients, which indicated that cytology HSIL+, HPV positive, CDB&ECC HSIL+ and TZ type 3 were risk factors for pathologic HSIL+, while colposcopy impression was not. Our result was in line with previous research in general, but colposcopy impression was not considered a risk factor for HSIL+. A possible explanation was that the consistency of colposcopy, as a subjective visual technique, was not standardized in the multicentre studies, and its quality control needs to be improved. Our results also indicated that patients with incomplete visibility of the TZ need to be further evaluated to exclude HSIL+. However, the number of patients with early-stage cervical cancer and “occult” cervical cancer was relatively small in our study, and the logistic regression model was not significant in predicting cervical cancer. A previous study revealed that the visibility of the squamocolumnar junction was associated with the incidence of occult cervical cancer, while cervical cytology before colposcopy was not.Citation36
The TZ is the area of the transformed metaplastic squamous epithelium, whose regression into the endocervix causes difficulty in detecting cervical lesions. In our study, the proportion of TZ type 1 was the highest in the normal cervix and cervicitis and decreased when the intraepithelial lesion occurred and progressed. The proportion of TZ type 3 increased with the progression of cervical lesions and reached its highest level in cervical cancer. The discrepancy between the histopathology results between CDB and conization was reported to be correlated with TZ type, and increased risk has been noted in patients with TZ type.Citation37,Citation38 In our study, 75.0% of occult cervical cancer patients were TZ type 3, which indicated that many cervical cancer patients with TZ type 3 might be missed by CDB due to declines in diagnostic agreement.
Most studies focused on the uniformity of the optimal length of cervical cone excision to avoid positive margins and reported its correlation with obstetrics prognosis, presenting an optimal length.Citation39,Citation40 However, no significant difference was found in the length of cervical cone excision between cone-diagnosed HSIL patients and cervical cancer patients in this study. To date, no publication has emphasized the proportion of cone excision length for detecting cervical cancer. The length of the cervix in our study varied among the women, owing to individualized variation or conization history. We converted the length to the length proportion of cervical cone excision, which can individualize its application. Our findings revealed that the length proportion of cervical cone excision was significantly higher in cervical cancer patients than in HSIL patients, and conization reached the best diagnostic value when the excision was performed above a length proportion of 0.563.
Despite the applicable results, our study has some limits. First, we only collected patients from five tertiary clinical centres in China, which may lead to selective bias that restricts the application of our findings. Second, 25 patients were lost to follow-up in our study, which may partially impact our conclusion. Third, not all enrolled patients finished all “three-step” screening procedures, resulting in incomplete information to fully elucidate the diagnostic value of the screening methods. Although the application of our findings is restricted and a study of a larger size needs to be performed for further verification and supplementation, our findings suggest the importance of conization for patients with TZ type 3 for detecting occult cervical cancer and we propose using the minimal length proportion (>0.56) of cervical cone excision, other than a uniform length.
Ethical Approval and Consent to Participate
Institutional review board/ethics committee approval was obtained from Fudan University Obstetrics and Gynecology Hospital for this study (reference number: Kyy2018-81), and written informed consent was obtained from the patients for publication of this report.
Acknowledgments
This study was supported by the Science and Technology Commission of Shanghai Municipality (No. 19411960100; No. 18411963600) and the National Natural Science Foundation of China (Grant No. 81701398). The authors thank the Shanghai Key Laboratory of Female Reproductive Endocrine Related Diseases.
Disclosure
The authors report no conflicts of interest in this work.
References
- Arbyn M, Weiderpass E, Bruni L, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020;8(2):e191–e203. doi:10.1016/S2214-109X(19)30482-6
- Narducci F, Merlot B, Bresson L, et al. Occult invasive cervical cancer found after inadvertent simple hysterectomy: is the ideal management: systematic parametrectomy with or without radiotherapy or radiotherapy only? Ann Surg Oncol. 2015;22(4):1349–1352. doi:10.1245/s10434-014-4140-5
- Lu HW, Li J, Liu YY, et al. Can radical parametrectomy be omitted in occult cervical cancer after extrafascial hysterectomy? Chin J Cancer. 2015;34(9):413–419. doi:10.1186/s40880-015-0041-7
- Pretorius RG, Belinson JL, Peterson P. Loop electrosurgical excision procedure or cervical conization to exclude cervical cancer before simple hysterectomy. J Low Genit Tract Dis. 2020;24(2):202–205. doi:10.1097/LGT.0000000000000519
- Choi DH, Huh SJ, Nam KH. Radiation therapy results for patients undergoing inappropriate surgery in the presence of invasive cervical carcinoma. Gynecol Oncol. 1997;65(3):506–511. doi:10.1006/gyno.1997.4711
- Subramaniam A, Fauci JM, Schneider KE, et al. Invasive cervical cancer and screening: what are the rates of unscreened and underscreened women in the modern era? J Low Genit Tract Dis. 2011;15(2):110–113. doi:10.1097/LGT.0b013e3181f515a2
- Kim SI, Kim SJ, Suh DH, Kim K, No JH, Kim YB. Pathologic discrepancies between colposcopy-directed biopsy and loop electrosurgical excision procedure of the uterine cervix in women with cytologic high-grade squamous intraepithelial lesions. J Gynecol Oncol. 2020;31(2):e13. doi:10.3802/jgo.2020.31.e13
- Cong Q, Song Y, Wang Q, et al. A large retrospective study of 12714 cases of LEEP conization focusing on cervical cancer that colposcopy-directed biopsy failed to detect. Biomed Res Int. 2018;2018:5138232. doi:10.1155/2018/5138232
- Giannella L, Mfuta K, Gardini G, Rubino T, Fodero C, Prandi S. High-grade CIN on cervical biopsy and predictors of the subsequent cone histology results in women undergoing immediate conization. Eur J Obstet Gynecol Reprod Biol. 2015;186:68–74. doi:10.1016/j.ejogrb.2015.01.015
- Noothong S, Inthasorn P, Warnnissorn M. Pathological discrepancy between colposcopic directed cervical biopsy and Loop Electrosurgical-Excision Procedures (LEEPs) in patients with biopsies proven high grade cervical intraepithelial neoplasia. Taiwan J Obstet Gynecol. 2017;56(5):628–631. doi:10.1016/j.tjog.2017.08.009
- Bornstein J, Bentley J, Bösze P, et al. 2011 colposcopic terminology of the international federation for cervical pathology and colposcopy. Obstet Gynecol. 2012;120(1):166–172. doi:10.1097/AOG.0b013e318254f90c
- Chappatte OA, Byrne DL, Raju KS, Nayagam M, Kenney A. Histological differences between colposcopic-directed biopsy and loop excision of the transformation zone (LETZ): a cause for concern. Gynecol Oncol. 1991;43(1):46–50. doi:10.1016/0090-8258(91)90007-r
- Stoler MH, Vichnin MD, Ferenczy A, et al.; FUTURE I, II and III Investigators. The accuracy of colposcopic biopsy: analyses from the placebo arm of the Gardasil clinical trials. Int J Cancer. 2011;128(6):1354–1362. doi:10.1002/ijc.25470
- Duesing N, Schwarz J, Choschzick M, et al. Assessment of cervical intraepithelial neoplasia (CIN) with colposcopic biopsy and efficacy of loop electrosurgical excision procedure (LEEP). Arch Gynecol Obstet. 2012;286(6):1549–1554. doi:10.1007/s00404-012-2493-1
- Witt BL, Factor RE, Jarboe EA, Layfield LJ. Negative loop electrosurgical cone biopsy finding following a biopsy diagnosis of high-grade squamous intraepithelial lesion: frequency and clinical significance. Arch Pathol Lab Med. 2012;136(10):1259–1261. doi:10.5858/arpa.2011-0494-OA
- Kabaca C, Koleli I, Sariibrahim B, et al. Is cervical punch biopsy enough for the management of low-grade cervical intraepithelial neoplasia? J Low Genit Tract Dis. 2014;18(3):240–245. doi:10.1097/LGT.0b013e3182aa08f6
- Jung Y, Lee AR, Lee SJ, Lee YS, Park DC, Park EK. Clinical factors that affect diagnostic discrepancy between colposcopically directed biopsies and loop electrosurgical excision procedure conization of the uterine cervix. Obstet Gynecol Sci. 2018;61(4):477–488. doi:10.5468/ogs.2018.61.4.477
- Stuebs FA, Schulmeyer CE, Mehlhorn G, et al. Accuracy of colposcopy-directed biopsy in detecting early cervical neoplasia: a retrospective study. Arch Gynecol Obstet. 2019;299(2):525–532. doi:10.1007/s00404-018-4953-8
- Hinkova N, Tsvetkov C, Tanchev L, Strateva D, Gorchev G. The role of colposcopy in diagnosis of pre-cancer and cancer of the uterine cervix. Akush Ginekol. 2010;49(6):37–40. Bulgarian.
- Luo XM, Song L, Wu JL, et al. Analysis of the reported data of national rural cervical cancer screening project from 2012 to 2013, China. Zhonghua Yu Fang Yi Xue Za Zhi. 2016;50(4):346–350. Chinese. doi:10.3760/cma.j.issn.0253-9624.2016.04.012
- Sopracordevole F, Clemente N, Alessandrini L, et al. Detection of occult endocervical glandular dysplasia in cervical conization specimens for squamous lesions. Pathol Res Pract. 2017;213(3):210–216. doi:10.1016/j.prp.2016.12.015
- Palmer JE, Amarad P, Ellis K, Dudding N, Smith J, Tidy JA. The outcome for women with microinvasive cervical cancer with stromal invasion 1 mm or less: should we always re-excise? Int J Gynecol Pathol. 2012;31(5):470–474. doi:10.1097/PGP.0b013e31824a1d8d
- Gao SJ, Wang Q, Zheng RL, et al. Retrospective analysis of positive leep surgical margin and residual lesion in 246 patients with cervical high grade squamous intraepithelial lesion and micro invasive cancer after leep conization. Tumor. 2011;31(4):359–363.
- Xiao FY, Wang Q, Zheng RL, Chen M, Su TT, Sui L. Diagnosis and treatment value of colposcopy and loop electrosurgical excision procedure in microinvasive cervical cancer: analysis of 135 cases. Zhonghua Fu Chan Ke Za Zhi. 2016;51(3):186–191. Chinese. doi:10.3760/cma.j.issn.0529-567X.2016.03.005
- Baldauf JJ, Dreyfus M, Ritter J, Philippe E. An analysis of the factors involved in the diagnostic accuracy of colposcopically directed biopsy. Acta Obstet Gynecol Scand. 1997;76(5):468–473. doi:10.3109/00016349709047830
- Byrom J, Douce G, Jones PW, et al. Should punch biopsies be used when high-grade disease is suspected at initial colposcopic assessment? A prospective study. Int J Gynecol Cancer. 2006;16(1):253–256. doi:10.1111/j.1525-1438.2006.00344.x
- Furtado Y, Almeida G, Lima R, Silva K, Maldonado P. Microinvasive squamous carcinoma (FIGO stage IA1) of the cervix: are there colposcopic criteria for the diagnosis? Am J Obstet Gynecol. 2011;205(4):360.e1–4. doi:10.1016/j.ajog.2011.06.036
- Repše-Fokter A, Pogačnik A, Snoj V, Primic-žakelj M, Fležar MS. Review of negative and low-grade cervical smears in women with invasive cervical cancer after the first 3 years of the national cervical screening programme in Slovenia. Cytopathology. 2012;23(1):23–29. doi:10.1111/j.1365-2303.2010.00816.x
- Khuakoonratt N, Tangjitgamol S, Manusirivithaya S, et al. Prevalence of high grade squamous intraepithelial lesion (HSIL) and invasive cervical cancer in patients with low grade squamous intraepithelial lesion (LSIL) at cervical pap smear. Asian Pac J Cancer Prev. 2008;9(2):253–257.
- López-Alegría F, De Lorenzi DS, Quezada OP. Follow-up of women with atypical squamous cells cannot exclude high-grade squamous intraepithelial lesions (ASC-H). Sao Paulo Med J. 2014;132(1):15–22. doi:10.1590/1516-3180.2014.1321597
- Pretorius RG, Belinson JL, Peterson P, Burchette RJ. Factors that virtually exclude cervical cancer at colposcopy. J Low Genit Tract Dis. 2015;19(4):319–322. doi:10.1097/LGT.0000000000000122
- Li J, Wang W, Yang P, et al. Analysis of the agreement between colposcopic impression and histopathological diagnosis of cervical biopsy in a single tertiary center of Chengdu. Arch Gynecol Obstet. 2021;304(4):1033–1041. doi:10.1007/s00404-021-06012-y
- Yamamoto R, Sekiyama K, Higuchi T, et al. Value and limitation of conization as a diagnostic procedure for cervical neoplasm. J Obstet Gynaecol Res. 2019;45(12):2419–2424. doi:10.1111/jog.14118
- Zhang X, Dou Y, Wang M, et al. A retrospective analysis on 1901 women with high grade cervical intraepithelial neoplasia by colposcopic biopsy. Eur J Obstet Gynecol Reprod Biol. 2017;217:53–58. doi:10.1016/j.ejogrb.2017.07.005
- Silver MI, Andrews J, Cooper CK, et al. Risk of cervical intraepithelial neoplasia 2 or worse by cytology, human papillomavirus 16/18, and colposcopy impression: a systematic review and meta-analysis. Obstet Gynecol. 2018;132(3):725–735. doi:10.1097/AOG.0000000000002812
- Qian XY, You ZX, Cao QW, Zou BB, Xing Y. Analysis of the missed diagnosis of invasive carcinoma under the microscope in HSIL diagnosed by colposcopy-guided biopsy and related influencing factors. Zhonghua Fu Chan Ke Za Zhi. 2018;53(9):613–619. Chinese. doi:10.3760/cma.j.issn.0529-567x.2018.09.006
- Ren H, Jia M, Zhao S, Li H, Fan S. Factors correlated with the accuracy of colposcopy-directed biopsy: a systematic review and meta-analysis. J Invest Surg. 2020;30:1–9. doi:10.1080/08941939.2020.1850944
- Fan A, Zhang L, Wang C, Wang Y, Han C, Xue F. Analysis of clinical factors correlated with the accuracy of colposcopically directed biopsy. Arch Gynecol Obstet. 2017;296(5):965–972. doi:10.1007/s00404-017-4500-z
- Kawano K, Tsuda N, Nishio S, et al. Identification of appropriate cone length to avoid positive cone margin in high grade cervical intraepithelial neoplasia. J Gynecol Oncol. 2016;27(5):e54. doi:10.3802/jgo.2016.27.e54
- Bae HS, Chung YW, Kim T, Lee KW, Song JY. The appropriate cone depth to avoid endocervical margin involvement is dependent on age and disease severity. Acta Obstet Gynecol Scand. 2013;92(2):185–192. doi:10.1111/aogs.12025
