Abstract
Purpose
Gestational diabetes mellitus (GDM) continues to be a significant health disorder triggering harmful complications in pregnant women and fetuses. Our knowledge of GDM epidemiology in Yemen is largely based on very limited data. The aim of this study was, therefore, to determine the prevalence and risk factors of GDM among pregnant women in Dhamar governorate, Yemen.
Patients and methods
A total of 311 subjects were randomly selected for this cross sectional survey. Health history data and blood samples were collected using a pretested questionnaire. To determine the prevalence of GDM, the fasting and random blood glucose techniques were applied according to the recommendations of the American Diabetes Association, using alternative methods that are more convenient to the targeted population. Poisson’s regression model incorporating robust sandwich variance was utilized to assess the association of potential risk factors in developing GDM.
Results
The prevalence of GDM was found to be 5.1% among the study population. Multivariate analysis confirmed age ≥30 years, previous GDM, family history of diabetes, and history of polycystic ovary syndrome as independent risk factors for GDM prevalence. However, body mass index ≥30 kg/m2 and previous macrosomic baby were found to be dependent risk factors.
Conclusion
This study reports new epidemiological information about the prevalence and risk factors of GDM in Yemen. Introduction of proper maternal and neonatal medical care and health education are important in order to save the mother and the baby.
Introduction
Gestational diabetes mellitus (GDM) is defined as “carbohydrate intolerance resulting in hyperglycemia of variable severity with onset or first recognition during pregnancy”.Citation1 Maternal hyperglycemia causes fetal hyperinsulinemia.Citation2 Many maternal and fetal adverse effects are associated with this carbohydrate disorder, such as fetal macrosomia, perinatal mortality, cesarean delivery, and preeclampsia.Citation3,Citation4 Later in life, this affected community tends to suffer from more complications, such as type 2 diabetes mellitus and obesity, however.Citation5–Citation7 Early diagnosis of GDM is, therefore, imperative to avoid such health problems.
Published reports show variations in the prevalence rates of GDM in most countries of the Arabian Peninsula, which comprises two distinct economies: the high-economy Gulf Cooperation Countries (GCC), and the poor, neglected Yemen. GDM was reported to vary between 4.2% and 24.9% in the GCC countries of Oman, Qatar, Bahrain, Kuwait, Saudi Arabia, and the United Arab Emirates.Citation8–Citation15 In Yemen, however, there are no epidemiological results reported in the literature, PubMed and Google Scholar databases, about the prevalence and risk factors of GDM.
Several health factors increase the risk of developing GDM: for example, older age, previous GDM, body mass index (BMI) >30 kg/m2, family history of diabetes, previous macrosomic baby weighing ≥4.5 kg, and ethnicity of high prevalence, particularly South Asian, black Caribbean, and Middle Eastern.Citation16 In addition, history of polycystic ovary syndrome (PCOS), glycosuria in current pregnancy, history of chronic hypertension, and previous stillbirth were indicated as significant predictors.Citation17–Citation19 Other risk factors were also reported; for a detailed review, see the clinical guideline of National Collaborating Centre for Women’s and Children’s Health.Citation6
Although the 75 g oral glucose tolerance test (OGTT) is the most reliable diagnostic technique for confirming GDM, using this method has been confirmed to be time consuming and expensive and to induce discomfort in the patients and the health providers.Citation20 Recently, the American Diabetes Association (ADA) recommended alternative procedures that are more adaptable. The ADA suggested that GDM can be confirmed without an OGTT when on 2 consecutive days a pregnant woman’s fasting blood glucose (FBG) level is >126 mg/dL or random blood glucose (RBG) level is >200 mg/dL.Citation21 More details on this topic can be found in the Handbook of Clinical Laboratory Testing During Pregnancy.Citation20
However, the early recognition of GDM prevalence is essential for considering the size of this health problem, taking the curative measures, and increasing the awareness of vulnerable women regarding the risk factors that would be important to prevent or at least decrease the risk of adverse outcome. Therefore, the present study aimed to determine the prevalence of GDM using the FBG and RBG techniques and to investigate the potential risk factors among pregnant women in Dhamar governorate, Yemen.
Patients and methods
Study area and subjects
The study was conducted in Dhamar governorate. It is located ~100 km south of Sana’a, the capital city of Yemen. The area is situated at an altitude of ~1,600–3,200 m with average temperature ranging from −1°C to 19°C. The economy is mostly agricultural. Dhamar governorate comprises 12 rural districts, and Dhamar city houses the main health facilities. The health centers associated with antenatal care clinics that were included in this study are Dhamar General Hospital, Maternal and Child Health Center, Mehrass Dispensary for Gynecology and Obstetrics, and Dar Al Shifa Hospital.
A total of 311 nondiabetic pregnant women participated in this study. They were aged 15–49 years with a gestational age ranging from 24 to 40 weeks. Before commencing data collection, informative meetings were held with the subjects in order to give a clear description of the aim of the study. All study subjects gave verbal consent. They were informed that their involvement was completely voluntary and they could decline to contribute at any point during the survey. The protocol of the study had been approved by the ethics committee of the faculty, Thamar University Medical Ethics Committee.
Study design
This was a cross sectional study carried out between August 2013 and March 2014. The sample size was calculated based on the middle prevalence value of GDM in the Arabian Peninsula (10%) with a 95% confidence level and a ±3.4 degree of precision. The study subjects were randomly selected from the antenatal care clinics using a systematic sampling method. Several visits were made to the antenatal care clinics, where demographic and anthropometric data and blood samples were collected from the participants by trained health staff. To determine the prevalence of GDM, the methods of FBG and RBG were used for diagnosing the blood samples according to the ADA criteria.Citation20,Citation21 A pregnant woman with GDM was confirmed if on 2 consecutive days, the level of her FBG or RBG was >126 or 200 mg/dL, respectively. As stated in the “Introduction” section, many health history factors increase the risk of developing GDM. Hence, the differences between the pregnant women groups (women with risk factors and women with no risk factors) were calculated with reference to the prevalence of GDM.
Questionnaire
The pregnant women selected for the study were interviewed, in their antenatal care clinics settings, using a pretested questionnaire constructed in Arabic, the native language of the participants. The questions were designed to gather information on their health history. Information on the following potential risk factors was collected during this survey: age ≥35 years, BMI ≥30 kg/m2, previous GDM, family history of diabetes, previous macrosomic baby, previous stillbirth, and history of PCOS.
Anthropometric assessment
Height and weight of all the participants were measured and recorded. The height was measured to the nearest 0.1 cm without shoes or any other tampered material with the participant standing on a flat surface. Pregravid weight was recorded to the nearest 0.1 kg. The BMI (kg/m2) was then calculated.
Biochemical screening
The collected blood samples were centrifuged, and blood glucose was immediately examined in the antenatal care clinic settings. Two analytical procedures were used, and the mean was calculated: glucose oxidase method (Lab Kit, Madrid, Spain) using a spectrophotometer RT-9200 semiautomatic chemistry analyzer and hexokinase method (Roche Diagnostics, GmbH, Mannheim, Germany) using a COBAS/INTEGRA 400/400 plus system.Citation22,Citation23 The operational descriptions of the FBG and RBG samples were as the following, respectively: no caloric intake for at least 8 hours; and any time of the day without regard to the time since the last meal.
Data analysis
The present study used the IBM SPSS (Version 22.0) statistical software for analysis of the data. General characteristics of the study participants were presented as a mean ± standard error of the mean (SEM) or percentage (%). For the data analysis, all the study variables were dichotomously evaluated. They were GDM prevalence (FBG ≤126 mg/dL or RBG ≤200 mg/dL =0 and FBG >126 mg/dL or RBG >200 mg/dL =1), age (<35 years =0 and ≥35 years =1), BMI (<30 kg/m2 =0 and ≥30 kg/m2 =1), previous GDM (no =0 and yes =1), family history of diabetes (no =0 and yes =1), previous macrosomic baby (no =0 and yes =1), previous stillbirth (no =0 and yes =1), and history of PCOS (no =0 and yes =1). Univariate analysis was used to examine the association between GDM as the dependent variable and the health history as the explanatory variables. Variables that showed an association with GDM at a P-value of ≤0.2 were used to adjust the multivariate regression model in order to evaluate their independent effect in developing GDM.Citation24,Citation25 According to the recent literature of regression models that are most appropriate for the cross sectional studies, Poisson’s regression model incorporating the robust sandwich variance was used to estimate the prevalence risk (PR).Citation26,Citation27 As a result, the estimated risk (ER) of GDM was then calculated (ER = PR −1). P≤0.05 was considered as the level of significance.
Results
General characteristics of the participants
A total of 311 pregnant women aged 15–49 years participated in this survey. The mean (±SEM) of age and BMI were 25.14 years (±0.37) and 24.61 kg/m2 (±0.19), respectively. shows the general health characteristics of the subjects according to the frequency (%) of the potential risk factors of GDM. The most frequent variables were previous stillbirth (29.6%) and family history of diabetes (23.2%). Accordingly, 12.5% of the pregnant women were ≥35 years, 12.2% had previous macrosomic baby, and 10% reported history of PCOS, whereas 5.8% women were obese (BMI ≥30 kg/m2) and 2.9% reported previous GDM.
Table 1 General health characteristics of the pregnant women participated in the study (N=311)
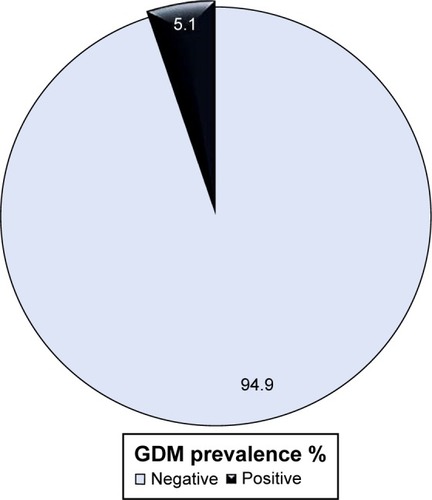
Prevalence of GDM
shows the prevalence of GDM among the study participants in Dhamar governorate, Yemen. GDM was diagnosed in 16 (5.1%) women, based on the ADA alternative methods of FBG and RBG.
Association of the potential risk factors with GDM
Dependent effect of the potential risk factors
The univariate regression analysis revealed a significant association between GDM and age ≥35 years, BMI ≥30 kg/m2, previous GDM, family history of diabetes, previous macrosomic baby, and history of PCOS (). Previous stillbirth, however, emerged as an insignificant risk factor for GDM. In the light of this analysis, the PR of GDM increases by 8.97 times by age ≥35 years (GDM =23.1 vs 2.6; P<0.001); by as much as 3.76 times among the BMI group ≥30 kg/m2 (GDM =16.7 vs 4.4; P=0.026); by 26.10 times in pregnant women who reported previous GDM (GDM =77.8 vs 3.0; P<0.001); and by 7.30, 4.31, and 3.01 times in those with a family history of diabetes (GDM =15.3 vs 2.1; P<0.001), a previous macrosomic baby (GDM =15.8 vs 3.7; P=0.003), and a history of PCOS (GDM =12.9 vs 4.3; P=0.043), respectively. Because all the health variables, including previous stillbirth, showed P-values of ≤0.2, they were used to develop the multivariate regression model.
Table 2 Univariate analysis for the potential risk factors of GDM among the pregnant women in Dhamar area, Yemen (N=311)
Independent effect of the potential risk factors
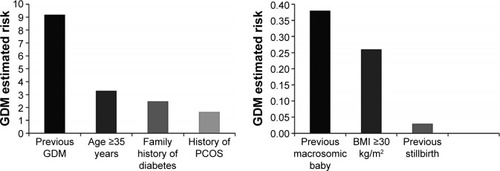
The independent effect of each potential risk factor on the prevalence of GDM is shown in . The multivariate analysis confirmed age (PR =4.29; P=0.005), previous GDM (PR =10.18; P<0.001), family history of diabetes (PR =3.48; P=0.049), and history of PCOS (PR =2.66; P=0.046) as independent risk factors for developing GDM among the study participants. BMI ≥30 kg/m2 and a previous macrosomic baby, however, emerged as dependent risk factors (P>0.05).
Table 3 Multivariate analysis for the potential risk factors of GDM among the pregnant women in Dhamar, Yemen (N=311)
GDM estimated risk
shows the adjusted ER of developing GDM among Yemeni pregnant women in Dhamar governorate, Yemen. Previous GDM showed the strongest association (ER =9.18), followed by age ≥35 years (ER =3.29), family history of diabetes (ER =2.48), and history of PCOS (ER =1.66). Accordingly, a lower degree of GDM risk was shown by previous macrosomic baby (ER =0.38), BMI ≥30 kg/m2 (ER =0.26), and previous stillbirth (ER =0.03).
Discussion
The main objectives of this survey were to determine the prevalence of GDM and predict the potential risk factors among the pregnant women in Yemen. The present study revealed that the prevalence rate of GDM is 5.1% among the study population in Dhamar governorate. This result is both in conflict and in agreement with some studies conducted in the neighboring countries of Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, and the United Arab Emirates. In general, the prevalence rate observed in this survey is related to the universal range varying from 3% to 14% among all pregnancies in different populations.Citation28 Although not all the potential risk factors showed independent and/or significant associations with GDM, the effect of these risks could be influenced by moderating or confounding variables.
Although the OGTT was not performed, this work is the first step toward enhancing our knowledge of GDM prevalence and its risk factors in Yemen. The study presented a lower rate of GDM prevalence than those reported in most of the neighboring GCC countries, ranging from 10.1% to 24.9%.Citation10–Citation15 However, it has a number of similarities with the results of the studies by Barakat et al (4.2%) in Oman and Al-Kuwari and Al-Kubaisi (6.4%) in Qatar.Citation8,Citation9 A recent review study examined the factors associated with GDM care in these countries,Citation29 which showed that the reported variations in the prevalence rates of GDM could be attributed to multiple factors, such as the use of different criteria of diagnosis, increase in the economic migration of multiethnic population, increase in the rates of obesity, and limitation of the conducted surveys. The circumstances in Yemen are completely different and cannot be compared to those of the high-income GCC countries. Food insecurity and malnutrition are chronic stress factors in Yemen. According to the United Nations World Food Program, Yemen is on the edge of famine, with almost half of the Yemeni people being food insecure.Citation30 Yemen also has one of the highest rates of malnutrition in the world.Citation31 Moreover, at the time of writing, Yemeni people are facing a destructive regional war and global terrorism, which is pushing the economy and health services to serious collapse.
In agreement with previous reports around the world, the following health variables have been found to be significant risk factors for GDM during the univariate analysis: age ≥35 years, BMI ≥30 kg/m2, previous GDM, family history of diabetes, previous macrosomic baby, and history of PCOS.Citation16–Citation18 Although the outcome of the adjusted multivariate model showed BMI ≥30 kg/m2 and previous macrosomic baby as dependent risks for GDM, the probability that these variables had regulated the independent association of the other variables is statistically accepted. Kew et al concluded that a prior pregnancy that resulted in a macrosomic baby is not necessarily presumptive evidence of undiagnosed GDM but may be a result of the influence of other predictors, such as obesity.Citation32 A previous study from Iran reported stillbirth during previous pregnancy as a significant predictor for GDM.Citation19 But this association was not revealed in this survey, which showed similar outcomes as those of a multicenter, randomized, controlled trial that was conducted on 440 pregnant women (220 GDM and 220 controls) in Saudi Arabia.Citation33
The results of the present study revealed previous GDM, age ≥35 years, family history of diabetes, and history of PCOS as the strongest predictors for developing GDM. Evidences from earlier surveys indicated that previous GDM and age ≥35 years are more associated with GDM than the other risk factors.Citation10,Citation34 Family history of diabetes was concluded in several cross sectional and prospective studies as a highly significant risk for developing GDM.Citation35,Citation36 Wang et al found that 54.9% of the incidence of GDM was significantly found among pregnant women with PCOS compared to 14.3% of those in the control group.Citation18 Therefore, recognizing such risk factors among pregnant women in Yemen is important and should be done by the medical staff in order to prevent the adverse effects of GDM. However, women with no risk factors are also at risk of developing GDM. Low sensitivities and specificities had been produced when risk factors were used alone as a screening test.Citation37 A study by Moses et al detected GDM in 39.2% of the pregnant women with no risk factors.Citation38 The present study gives information about the risks of GDM that can help improve primary health care measures. However, all pregnant women should be examined to see whether they carry the risk factors.
Conclusion
To the best of our knowledge, this is the first report showing the prevalence of GDM in Yemen. GDM is seen to affect ~5% of the population. The results indicated previous GDM, age ≥35 years, family history of diabetes, and history of PCOS as independent risk factors. BMI ≥30 kg/m2 and previous macrosomic baby increased the risk of GDM but in a dependent manner. However, previous stillbirth was an insignificant variable. The results of the present study highlight the importance of early screening, diagnosis, and treatment of this maternal health concern. Introduction of proper educational programs about the risk factors of GDM is an essential preventive measure to decrease the risk of adverse perinatal outcome. Further studies in different regions of Yemen are recommended to reveal the general prevalence of GDM in the country.
Acknowledgments
The authors would like to thank the following fourth-year students of the Medical Laboratories Sciences (academic year 2012/2013) for their help in the collection of the study data: M Al-Mutahher, M AL-Halani, G AL-Mohalla, M Al-Madwamy, S AL-Manarri, S Saleh, A Mana, M Al-Marhabi, H Zyad, S Hassan, A Daban, B Al-Mogad, E Naser, A AL-Athraay, and Y Al-Haj. The authors would also like to acknowledge the staff of Dhamar public and private hospitals and health centers for their generous support and cooperation in the collection and analysis of the study data. The efforts of the pregnant women for their participation in this study are highly appreciated. This work was financially supported by the Faculty of Medicine and Health Sciences, Thamar University.
Disclosure
The authors report no conflicts of interest in this work.
References
- AlbertiKGZimmetPZDefinition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultationDiabet Med19981575395539686693
- PedersenJWeight and length at birth of infants of diabetic mothersActa Endocrinol (Copenh)195416433034213206643
- CrowtherCAHillerJEMossJRFor ACHOIS Trial GroupEffect of treatment of gestational diabetes mellitus on pregnancy outcomesN Engl J Med2005352242477248615951574
- DoddJMCrowtherCAAntoniouGBaghurstPRobinsonJSScreening for gestational diabetes: the effect of varying blood glucose definitions in the prediction of adverse maternal and infant health outcomesAust N Z J Obstet Gynaecol200747430731217627686
- SilvermanBLRizzoTAChoNHMetzgerBELong term effects of the intrauterine environment. Northwestern university diabetes in pregnancy centerDiabetes Care199821suppl 2B142B1499704242
- National Collaborating Centre for Women’s and Children’s HealthDiabetes in Pregnancy: Management of Diabetes and Its Complications from Preconception to the Postnatal PeriodLondonRCOG Press2008
- LeeHJangHCParkHKMetzgerBEChoNHPrevalence of type 2 diabetes among women with a previous history of gestational diabetes mellitusDiabetes Res Clin Pract200881112412918456364
- BarakatMNYoussefRMAl-LawatiJAPregnancy outcomes of diabetic women: charting Oman’s progress towards the goal of the Saint Vincent declarationAnn Saudi Med201030426527020622342
- Al-KuwariMGAl-KubaisiSBPrevalence and predictors of gestational diabetes in QatarDiabetol Croat2011406570
- BenerASalehNMAl-HamaqAPrevalence of gestational diabetes and associated maternal and neonatal complications in a fast-developing community: global comparisonsInt J Womens Health2011336737310.2147/ijwh.s2609422140323
- RajabKEIssaAAHasanZARajabEJaradatAAIncidence of gestational diabetes mellitus in Bahrain from 2002–2012Int J Gynaecol Obstet20121171747722265190
- SultanFAnanGAhmedSClinical epidemiology of gestational diabetes in KuwaitKuwait Med J200436195198
- ArdawiMSNasratHAJamalHSAl-SaqaafHMMustafaBEScreening for gestational diabetes mellitus in pregnant femalesSaudi Med J200021215516011533772
- WahabiHAFayedAAAlzeidanRAMandilAAThe independent effects of maternal obesity and gestational diabetes on the pregnancy outcomesBMC Endocr Disord2014144724923207
- AgarwalMMDhattGSShahSMGestational diabetes mellitus: simplifying the international association of diabetes and pregnancy diagnostic algorithm using fasting plasma glucoseDiabetes Care20103392018202020519664
- American Diabetes AssociationGestational diabetes mellitusDiabetes Care2000237779
- AshrafiMSheikhanFArabipoorAHosseiniRNourbakhshFZolfaghariZGestational diabetes mellitus risk factors in women with polycystic ovary syndrome (PCOS)Eur J Obstet Gynecol Reprod Biol201418119519925150960
- WangYZhaoXZhaoHRisks for gestational diabetes mellitus and pregnancy-induced hypertension are increased in polycystic ovary syndromeBiomed Res Int2013201318258224371816
- SoheilykhahSMogibianMRahimi-SaghandSRashidiMSoheilykhahSPirozMIncidence of gestational diabetes mellitus in pregnant womenIran J Reprod Med2010812428
- DukesWJChenACJovanovicLDiabetes in pregnancyGronowskiAMHandbook of Clinical Laboratory Testing During PregnancyTotowa, NJHumana Press Inc2004359390
- The Expert Committee on the Diagnosis and Classification of Diabetes MellitusReport of the expert committee on the diagnosis and classification of diabetes mellitusDiabetes Care200225suppl 1S5S20
- TrinderPDetermination of glucose in blood using glucose oxidase with an alternative oxygen receptorAnn Clin Biochem196962427
- KaplanLAGlucosePesceAJKaplanLAPesceAJClinical Chemistry: Theory, Analysis, and CorrelationSt Louis, MOMosby198410321036
- BendelRBAfifiAAComparison of stopping rules in forward regressionJ Am Stat Assoc1977723574653
- GroenwoldRHHKlungelOHGrobbeeDEHoesAWSelection of confounding variables should not be based on observed associations with exposureEur J Epidemiol201126858959321796419
- LeeJTanCSChiaKSA practical guide for multivariate analysis of dichotomous outcomesAnn Acad Med Singapore200938871471919736577
- CoutinhoLMScazufcaMMenezesPRMethods for estimating prevalence ratios in cross sectional studiesRev Saude Publica200842699299819009156
- BenhalimaKCrombruggePVHanssensMDevliegerRVerhaegheJMathieuCGestational diabetes: overview of the new consensus screening strategy and diagnostic criteriaActa Clin Belg201267425526123019800
- OkunoyeGKonjeJLindowSPervaSGestational diabetes in the gulf region: streamlining care to optimise outcomeJ Local Global Health Sci201520152
- United Nations World Food Programme (WFP) [webpage on the internet]Yemen Emergency Available from: http://m.wfp.org/emergencies/yemenAccessed September 27, 2015
- United Nations World Food Programme (WFP) [webpage on the internet]Yemen Comprehensive Food Security Survey. Sana’aWFP Available from: http://documents.wfp.org/stellent/groups/public/documents/ena/wfp219039.pdfAccessed December 17, 2015
- KewSYeCSermerMPostpartum metabolic function in women delivering a macrosomic infant in the absence of gestational diabetes mellitusDiabetes Care201134122608261321972414
- GasimTGestational diabetes mellitus: maternal and perinatal outcomes in 220 Saudi womenOman Med J201227214014422496940
- OstlundIHansonUOccurrence of gestational diabetes mellitus and the value of different screening indicators for the oral glucose tolerance testActa Obstet Gynecol Scand200382210310812648169
- Hossein-NezhadAMaghbooliZVassighARLarijaniBPrevalence of gestational diabetes mellitus and pregnancy outcomes in Iranian womenTaiwan J Obstet Gynecol200746623624117962102
- BhatMRameshaKNSarmaSPMenonSSowminiCVGaneshKSDeterminants of gestational diabetes mellitus: a case control study in a district tertiary care hospital in south IndiaInt J Diabetes Dev Ctries2010302919620535313
- ScottALovemanEMcIntyreLWaughNScreening for gestational diabetes: a systematic review and economic evaluationHealth Technol Assess2002611116112433317
- MosesRGriffithsRDavisWGestational diabetes: do all women need to be tested?Aust N Z J Obstet Gynaecol19953543873898717560