Abstract
Renal cell carcinoma (RCC) is a common malignancy with high metastatic potential, primarily due to its extensive vascularity. Common sites of metastasis include lungs, bone, lymph nodes, liver, and brain. However, rare cases of metastasis to other sites including inguinal lymph nodes, peritoneum/mesentery, and orbit have been published in the literature. Herein, a unique case involving metastasis of RCC to the uvula is presented. The patient is a 55-year-old White female with a past medical history of stage 3 (T3aN0M0) RCC s/p nephrectomy 3 years prior to presentation. She had symptoms of a foreign body sensation at the back of her throat, and oropharyngeal examination revealed uvular erythematous mass with vascularity. Uvular biopsy and complete excision were performed, which revealed metastatic RCC. Palate biopsy was negative and revealed only squamous mucosa with mild chronic inflammation. To our knowledge, there is only one other documented case of RCC metastasis to the uvula in the literature.
Introduction
Renal cell carcinoma (RCC) is a common malignancy with high metastatic potential, primarily due to its extensive vascularity. In 2017, there were ~64,000 estimated new cases of RCC in the US (representing 3.8% of all new cancer cases), resulting in 14,400 estimated deaths. Approximately 9,500 of these estimated deaths were noted to be in males, while ~5,000 were in females.Citation1 Globally, RCC accounts for ~2% of all malignancies, with ~189,000 new cases annually. In the US, epidemiological data have shown that the incidence rates are higher among the African Americans compared to Caucasians. Established risk factors for RCC include tobacco, obesity (as measured by BMI), chronic hepatitis C, ionizing radiation, and end stage renal disease (ESRD).Citation2 Histopathological subtypes of RCC include clear cell (60%–70%), papillary (5%–15%), chromophobic (5%–10%), oncocytic (5%–10%), and collecting duct (<1%).Citation3 Common sites of metastasis include lungs, bone, lymph nodes, liver, and brain. However, there have been rare cases of metastases to other sites including inguinal lymph nodes, peritoneum/mesentery, and orbit published in the literature.Citation4–Citation6 Herein, a rare case involving metastasis of RCC to the uvula is presented.
Case presentation
This case report is about a 55-year-old White female with a PMH of RCC diagnosed 3 years prior to presentation with uvular metastasis. She was noted to have stage 3 RCC at the time of presentation (T3aN0M0). She had renal ultrasound that showed large 9.2 cm solid right renal mass without hydronephrosis and underwent right nephrectomy that revealed grade 3 clear cell carcinoma with extension of the mass into the renal sinus fat and some vascular invasion into the renal sinus, without renal vein invasion. Approximately 1 year after nephrectomy, computed tomography (CT) showed small nodule along the anterior aspect of the uncinate process of the pancreas, and biopsy revealed grade 2 metastatic RCC. Celiac axis lymph nodes were negative, and the patient underwent the Whipple procedure.
A year later, the patient reported having persistent headaches, which started ~3 months prior to visit. She had also reported having vertical diplopia on upward gaze. CT of the head and sinuses was taken, which revealed a 2.2 cm circumscribed mass of the left ethmoid sinus. Magnetic resonance imaging (MRI) was taken for further evaluation, which showed a well circumscribed, intensely enhancing mass 2.3 cm in diameter in the left nasal cavity, bulging into the left maxillary sinus. Stereotactic CT-guided endoscopic sinus surgery was performed, which showed that the mass extended into the maxillary sinus and was causing a dehiscent lamina papyracea. A large maxillary antrostomy and sphenoidectomy was required to resect the tumor completely. A septal perforation was visualized which was thought to be from extension of the tumor in the nasal cavity onto the septum. Embolization was performed by interventional radiology prior to endoscopic sinus surgery and resulted in successful preoperative embolization of bilateral internal maxillary arteries. Frozen sections were sent to pathology and confirmed RCC of the left ethmoid and nasal cavity. Following surgical resection of ethmoid mass, the patient underwent intensity-modulated radiation therapy to the ethmoid sinus area via tomotherapy for a total dose of 3,900 cGy. Chemotherapy treatment included sunitinib, which was stopped based on the predicted lack of response on molecular profiling test results, and later everolimus, which was stopped due to grade 3 fatigue and severe mucositis.
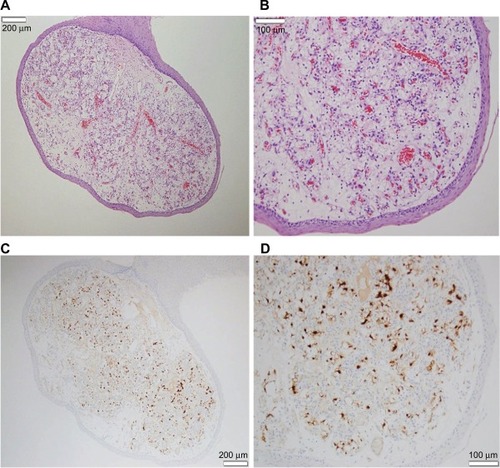
Approximately a year after left ethmoid sinus metastasectomy, metastasis to the uvula was detected. The patient presented with vague nasal symptoms such as congestion, and MRI of the sinuses was negative for any tumor. Examination of the oropharynx by otorhinolaryngology revealed a uvular erythematous mass with vascularity, ~2 mm in size, and a 2 mm papillomatous lesion in the left hard palate. Positron emission tomography/CT looking for the extent of disease at this time showed no focal fluorodeoxyglucose (FDG) avid abnormalities in the region of the uvula, but did show moderately FDG avid 1.2 cm noncalcified nodule medially in the left suprahilar region, later found on biopsy to be bronchial carcinoid. Uvular biopsy and complete excision were performed by otorhinolaryngology surgery, which revealed metastatic RCC (). Palate biopsy was negative and revealed only squamous mucosa with mild chronic inflammation. The patient was restarted on a lower dose of everolimus, which she tolerated well without experiencing any of the previously mentioned side effects. Everolimus was continued until recent disease progression with new lung metastases visualized on CT, at which time the patient was switched to pazopanib, an oral vascular endothelial tyrosine kinase inhibitor.
Figure 1 Slides of metastatic renal cell carcinoma (RCC) to the uvula.
Copyright/ethics
Written informed consent has been provided by the patient to have the details of her case and accompanying image published.
Discussion
RCC originates from the renal cortex and comprises the majority of primary renal malignancies. Classically, RCC presents with flank pain, hematuria, and a palpable renal mass; however, this only occurs in a minority of patients with RCC and typically indicates the presence of an advanced disease state. Our index case presented with complaints of flank pain, which prompted renal ultrasound that showed a solid renal mass, with nephrectomy revealing a stage 3 (T3aN0M0) carcinoma at presentation. Paraneoplastic symptoms involving RCC can include anemia, hypercalcemia, fever, hepatic dysfunction, and erythrocytosis. Initial radiographic testing includes either CT or ultrasound, and MRI can also be utilized to determine the involvement of inferior vena cava.
This case gives a unique presentation of RCC metastasizing to the uvula, which differs from more common areas of metastasis including lungs, brain, bone, lymph nodes, and liver. Metastasis of RCC to the paranasal sinuses is rare; however, there have been multiple documented case reports describing RCC spread to the nasal septum as well as to the maxillary and ethmoid sinuses.Citation7 RCC is the most common malignancy that metastasizes to this region.Citation8,Citation9 The most common path via which RCC cells spread to the sinonasal region includes that via the inferior vena cava–heart–maxillary artery as well as via the avalvular vertebral venous plexus and the intracranial venous plexus.Citation9 The most common sinonasal sites of metastasis include the maxillary sinuses (36%), ethmoid sinuses (25%), frontal and sphenoid sinuses (17%), and the nasal cavity (11%).Citation9 Of note, in our index case, metastasis of RCC to the ethmoid sinus was seen (and surgically resected) prior to the detection of RCC metastasis to the uvula. There have also been multiple documented cases and literature reviews of RCC metastasis to the tongue.Citation10 To our knowledge, there is only one other documented case of RCC metastasis to the uvula in the literature.Citation11
Metastasis of RCC to the head and neck region is rare.Citation12,Citation13 Sinonasal malignancies are typically primary neoplasms, with metastatic tumors being rare; however, RCC is the most common malignancy to metastasize to this region. An analysis of 412 metastatic lesions to the oral soft tissues showed that RCC mainly metastasized to the tongue compared to the other oral soft tissues, with a total of 19 cases.Citation14 However, the oral cavity in general is an uncommon site for metastasis, as only 1% of all malignant oral tumors are composed of metastatic lesions. A literature review performed by Azam et alCitation12 revealed a total of 28 cases that presented with tongue metastases prior to the diagnosis of primary RCC. This is in part due to the fact that metastatic lingual lesions present with ulcerating, polypoid, or vegetating lesions similar to primary malignancies of the tongue.Citation12 Thus, in cases in which an oral ulcerating lesion is seen, it is always important to make histopathological diagnosis instead of clinical diagnosis based on appearance, as the prognosis and treatment will vary significantly based on the type of malignancy. This is also particularly true for masses presenting with a hypervascular structure, and preoperative diagnosis can allow for the preparation for increased bleeding during surgical excision. In our index case presentation, the diagnosis of RCC was made ~2 years prior to the detection of metastatic ethmoid mass and ~3 years prior to the detection of the metastatic uvular mass. Possible routes of spread include arterial, venous, and lymphatic circulation.
In a review performed by Hirshberg et alCitation15 analyzing 157 cases of metastases to the oral mucosa, there were a total of 21 cases of metastatic RCC. Out of these 21 cases, only two had metastasized to the palate as compared to other oral sites, and there were no documented cases of metastases to the uvula, as was seen in our index case.
RCC metastasis to the head and neck region including the paranasal sinuses and the lingual area also typically predicts poor survival, and the treatment can include surgical excision of metastatic lesions and radiotherapy for palliation of pain, control of bleeding, and management of dysphagia. This is particularly important for larger metastatic lesions, as continued metastatic tumor enlargement can potentially lead to airway obstruction. In our index case, surgical excision was used to remove the uvular mass after being detected on MRI. Adjuvant radiation therapy can also be used with palliative intent. In our index case, surgical resection was followed by intensity-modulated radiation therapy to the ethmoid sinus area via tomotherapy, with a total dose of 3,900 cGy. Embolization of vascular lesions seen in certain head and neck tissues (including the tongue) has been discussed and was utilized in our index case for embolization of internal maxillary arteries prior to endoscopic sinus surgical excision of ethmoid mass, but was not required prior to surgical excision of the uvular metastatic lesion.
Acknowledgments
The authors like to thank Dr Ashley Flowers, Department of Pathology, Louisiana State University Health, for providing the histopathology figures for the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- SiegelRLMillerKDJemalACancer statistics, 2017CA Cancer J Clin201767173028055103
- LindbladPEpidemiology of renal cell carcinomaScand J Surg2004932889615285559
- RiniBICampbellSCEscudierBRenal cell carcinomaLancet200937396691119113219269025
- ChaudhryQSBhattyTAKhanZOsmanEMRenal cell carcinoma: atypical metastasis to inguinal lymph nodesUrol Ann201791808228216937
- StaderiniFCianchiFBadilBA unique presentation of renal clear cell carcinoma with atypical metastasesInt J Surg Case Rep201511293225911241
- SountoulidesPMetaxaLCindoloLAtypical presentations and rare metastatic sites of renal cell carcinoma: a review of case reportsJ Med Case Rep2011542921888643
- SinghJBahetiVYadavSSMathurROccult renal cell carcinoma manifesting as nasal mass and epistaxisRev Urol201416314514825337047
- ZiariMShenSAmatoRJTheBSMetastatic renal cell carcinoma to the nose and ethmoid sinusUrology2006671199
- RalliMAltissimiGTurchettaRRiganteMMetastatic renal cell carcinoma presenting as a paranasal sinus mass: the importance of differential diagnosisCase Rep Otolaryngol200620179242374
- LangEEPatilNWalshRMLeaderMWalshMAA case of renal cell carcinoma metastatic to the nose and tongueEar Nose Throat J200382538238312789766
- LansiganNCJrBenischBMSidotiJSRenal cell carcinoma presenting as metastasis to the uvulaUrology1973244494514753080
- AzamFAbubakerrMGollinsSTongue metastasis as an initial presentation of renal cell carcinoma: a case report and literature reviewJ Med Case Rep2008224918657269
- AltuntasOPetekkayaISusluNGulluIRenal cell carcinoma metastatic to the tongue: a case report and review of the literatureJ Oral Maxillofac Surg20157361227123025843819
- IraniSMetastasis to the oral soft tissues: a review of 412 casesJ Int Soc Prev Community Dent20166539340127891304
- HirshbergALeibovichPBuchnerAMetastases to the oral mucosa: analysis of 157 casesJ Oral Pathol Med19932293853908301602
