Abstract
Purpose
This study aimed to demonstrate the clinical usefulness of measuring the macular ganglion cell complex (GCC) for the early detection of axonal loss in eyes with bilateral retrobulbar optic neuropathies.
Patients and methods
We retrospectively reviewed the medical records of three patients with bilateral toxic, ischemic, or infiltrative retrobulbar optic neuropathy.
Results
No relative afferent pupillary defect was detected in any patients. The results of the fundus examinations were unremarkable at the initial presentation except for slight optic disk pallor in the right eye of Case 3. Magnetic resonance imaging showed no abnormal findings in Cases 1 and 2. Measurement of the macular GCC clarified the presence of axonal loss in all three cases with diagnostic uncertainty. Although reduction in the macular GCC thickness was not observed initially in Case 2, it became evident later when both optic disks still appeared normal.
Conclusion
A reduction in the macular GCC thickness seemed to precede the appearance of optic disk pallor and occurs regardless of toxic, ischemic, or infiltrative retrobulbar optic neuropathy. The current case series suggested that measurement of the macular GCC facilitated early differentiation between bilateral retrobulbar optic neuropathy and nonorganic visual loss, which can otherwise be challenging in some cases.
Introduction
Patients with retrobulbar optic neuropathy can present with medically unexplained visual loss requiring differentiation from nonorganic visual loss.Citation1 The only objective sign of this organic disorder might be a relative afferent pupillary defect (RAPD) in the affected eye; however, an RAPD might not be detected when the optic neuropathy is bilateral and symmetric. In the current case series, we retrospectively reviewed three patients with bilateral retrobulbar optic neuropathies, including toxic, ischemic, and infiltrative optic neuropathies.Citation2–Citation5 We showed the clinical usefulness of measuring the macular ganglion cell complex (GCC) for the early detection of axonal loss in eyes with bilateral retrobulbar optic neuropathies.
Case series
Case 1
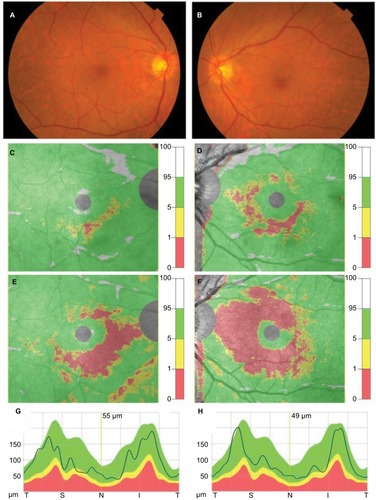
A 72-year-old man presented with gradual bilateral visual loss during the previous 1 month. He presented with best-corrected visual acuities (BCVAs) of 0.2 and 0.08 in the right and left eyes (OD and OS, respectively), with no RAPD. The results of a fundus examination were unremarkable in both eyes (“oculus uterque” or OU) (). When the GCC thickness was measured by optical coherence tomography (OCT) (RS-3000 Advance OCT; Nidek, Gamagori, Japan), there was a slight reduction in the papillomacular bundles OU (). The reduction in the papillomacular bundles worsened during the follow-up period (), but no changes in circumpapillary retinal nerve fiber layer (cpRNFL) parameters were observed (). Goldmann perimetry showed central scotomas and temporal depressions OU. The results of contrast-enhanced magnetic resonance imaging (MRI) of the brain and orbits with fat suppression were normal. The medical history included nontuberculous mycobacterial pulmonary infections, which had been treated daily with 750 mg of ethambutol for 16 months. When bilateral toxic optic neuropathy was diagnosed, the ethambutol was discontinued to minimize any additional toxic effects. Sixteen months after the initial presentation, his BCVAs were 0.8 OD and 0.5 OS.
Figure 1 Fundus photographs and results of measurement of the macular GCC and cpRNFL obtained from Case 1.
Abbreviations: GCC, ganglion cell complex; cpRNFL, circumpapillary retinal nerve fiber layer; T, temporal; S, superior, N, nasal; I, inferior.
Case 2
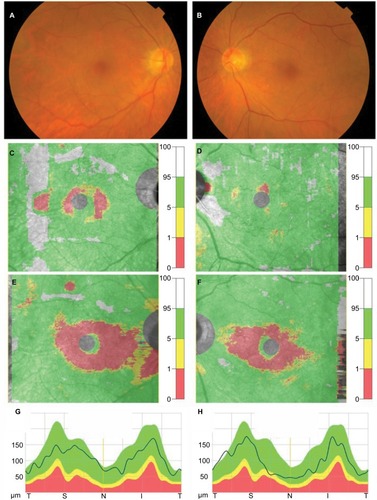
An 83-year-old man presented with sudden bilateral visual loss 2 weeks previously. He presented with BCVAs of 0.03 OU and no RAPD. The results of a fundus examination were unremarkable OU, except for retinal arteriolosclerosis OU (). OCT showed that the reduction in the macular GCC thickness was not apparent at the initial presentation (). It became evident 1 month later when both optic disks still appeared normal (), but no changes in cpRNFL parameters were observed (). Goldmann perimetry showed central scotomas OU. The results of MRI of the brain and orbits with fat suppression were normal. The medical history included end-stage renal disease, anemia, and hypertension, and he had been undergoing hemodialysis. Posterior ischemic optic neuropathy was diagnosed OU. Four months after the initial presentation, his BCVAs were 0.01 OU.
Figure 2 Fundus photographs and results of measurement of the macular GCC and cpRNFL obtained from Case 2.
Abbreviations: GCC, ganglion cell complex; cpRNFL, circumpapillary retinal nerve fiber layer; T, temporal; S, superior, N, nasal; I, inferior.
Case 3
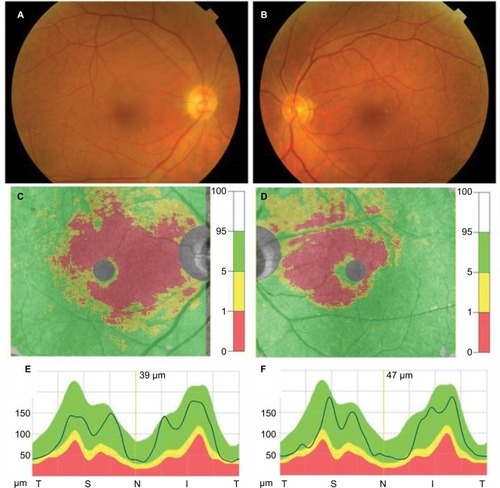
A 58-year-old man presented with gradual bilateral visual loss over the previous 2 months. He presented with BCVAs of 0.15 OD and 0.5 OS with no RAPD. The results of a fundus examination were unremarkable OU, except for slight optic disk pallor OD (). OCT showed decreased papillomacular bundles OU (), but no changes in cpRNFL parameters were observed (). Goldmann perimetry showed a paracentral scotoma OD. Contrast-enhanced MRI of the brain and orbits with fat suppression showed enlargement and gadolinium enhancement of the bilateral optic nerves. Analysis of the cerebrospinal fluid led to the diagnosis of lymphoplasmacytic lymphoma, which was treated with intrathecal and systemic chemotherapy. Infiltrative optic neuropathy was diagnosed. Four months after the initial presentation, his BCVAs were 0.15 OD and 0.4 OS.
Figure 3 Fundus photographs and results of measurement of the macular GCC and cpRNFL obtained from Case 3.
Abbreviations: GCC, ganglion cell complex; cpRNFL, circumpapillary retinal nerve fiber layer; T, temporal; S, superior, N, nasal; I, inferior.
Ethics statement
Written informed consent has been provided by the patients to have the case details and any accompanying images published.
Discussion
Retrobulbar optic neuropathy OU can be challenging to diagnose. First, RAPD might not be detected in cases with retrobulbar optic neuropathy OU. Second, although optic disk pallor usually develops over time, the optic disk might appear normal initially. Third, the presence of normal optic nerves on MRI images does not rule out a diagnosis of retrobulbar optic neuropathy.Citation2–Citation4,Citation6 In the current case series, an RAPD was not detected in any patient. The fundus examinations were unremarkable at initial presentation, and no abnormalities were seen on the MRI images in Cases 1 and 2.
The patterns of macular GCC loss might provide an objective measure of optic nerve damage in patients with chiasmal compression.Citation7,Citation8 In the current case series, measurements of the macular GCC were useful to clarify the presence of axonal loss in cases with diagnostic uncertainty. Although reduction in the macular GCC was not observed 2 weeks after the onset in Case 2, it became evident 6 weeks after the onset when both optic disks still appeared normal. The reduction in the macular GCC thickness seemed to precede the appearance of optic disk pallor and occurred regardless of the type of optic neuropathy.
Conclusion
The current case series suggested that measurement of the macular GCC can facilitate early differentiation between retro-bulbar optic neuropathy OU and nonorganic visual loss, which can otherwise be challenging in some cases. However, we must always keep in mind that the macular GCC should be evaluated after taking a careful medical history and fundus examination.
Acknowledgments
The authors thank Lynda Charters for her contribution to the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- MillerNRRetrobulbar optic neuropathies: an overviewBrownCLWalsh and Hoyt’s Clinical Neuro-Opthalmology4th edBaltimoreWilliams & Wilkins1982272278
- GrzybowskiAZülsdorffMWilhelmHTonagelFToxic optic neuropathies: an updated reviewActa Ophthalmol201593540241025159832
- BiousseVNewmanNJIschemic optic neuropathiesN Engl J Med2015372252428243626083207
- HayrehSSPosterior ischaemic optic neuropathy: clinical features, pathogenesis, and managementEye (Lond)200418111188120615534605
- KimJLMendozaPRRashidAHayekBGrossniklausHEOptic nerve lymphoma: report of two cases and review of the literatureSurv Ophthalmol201560215316525595061
- RizzoJFAndreoliCMRabinovJDUse of magnetic resonance imaging to differentiate optic neuritis and nonarteritic anterior ischemic optic neuropathyOphthalmology200210991679168412208717
- YumHRParkSHParkHYShinSYMacular ganglion cell analysis determined by Cirrus HD optical coherence tomography for early detection of chiasmal compressionPLoS One2016114e015306427049647
- TiegerMGHedgesTRHoJGanglion cell complex loss in chiasmal compression by brain tumorsJ Neuroophthalmol201737171228192385
