Abstract
A 56-year-old woman had an yellow-white retinal lesion superior to the optic disc. Optical coherence tomography demonstrated the mass with a snowball configuration and smooth surface. Autofluorescence disclosed revealed moderate hypoautofluorescence. Ultrasonography showed no calcification. Visual field examination showed an enlargement of the blind spot corresponding to the predominantly superotemporal juxtapapillary extension of the lesion. Eight months later, the lesion spontaneously resolved. Presumed solitary circumscribed retinal astrocytic proliferation (PSCRAP) is a benign stable retinal tumor, but PSCRAP has been reported to resolve spontaneously here. It differs from other white or yellow-white lesions of the retina in important ways that enable the ophthalmologist to reassure the patient as to its benign prognosis.
Introduction
The retina is made up of specialized neurons and glial cells.Citation1 In cases of retinal injuries, the glial cells become reactive and form a glial scar so clinically significant that involves multiple differential diagnoses and is associated with changes in the retinal architecture.Citation1 Massive retinal gliosis is rare and develops in long-standing eye diseases or trauma, but normally not assume tumor proportions and is generally not considered in the differential diagnosis of glial tumors.Citation1,Citation2 Recently, a rare retinal lesion has been described, known as the presumed circumscribed solitary proliferation of retinal astrocytes (PSCRAP), with its own characteristics that make it unique and that usually remains stable in size since diagnosis.Citation4 We report a clinical case of PSCRAP that experienced spontaneous regression 8 months after it was detected, leaving normal retina at the site of the lesion.
Clinical case
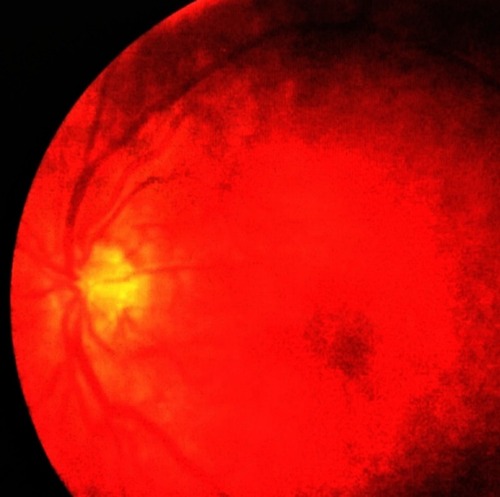
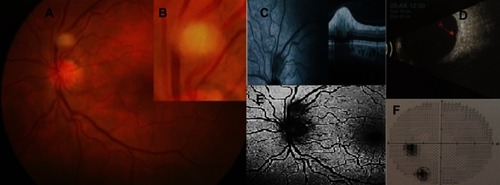
A 56-year-old woman was referred for an incidental retinal lesion in the left eye. She had no history of tuberous sclerosis complex (TSC) or neurofibromatosis type 1. She had no ocular symptoms. On examination, her visual acuity was 20/20 in both eyes. No significant finding was observed on anterior segment examination. Intraocular pressure was 12 mmHg bilaterally. She had no afferent pupillary defect and had normal color vision in both eyes. Ophthalmoscopy revealed a yellow-white lesion of one-fourth of papillary diameter and the edges slightly blurred located between the superior temporal vein and artery blood vessels close to the optic nerve (). Neither feeder nor draining vessels were observed and there were no network vessels in the lesion. Fundus examination of the right eye was normal. The patient refused fluorescein angiography. Optical coherence spectral tomography (SD-OCT) showed a hyperreflective mass on the RPE with a smooth, well-defined border in form of a snowball and a slight optical acoustic shadow (). B scan ultrasonography showed an elevated mass without calcifications (). Fundus autofluorescence showed mild hypoautofluorescence with a small nidus of hyperautofluorescence (). Visual field examination showed an enlargement of the blind spot corresponding to the predominantly superotemporal juxtapapillary extension of the lesion (). Eight months after the first visit, the lesion spontaneously regressed leaving a retina of normal appearance (). The authors confirm that written informed consent has been provided by the patient to have the case details and any accompanying images published and institutional approval was required to publish the case details.
Figure 1 (A) Fundus photo on presentation showing a yellow-white mass in the retina, abruptly elevated without vessels distributed amongst the lesion. (B) High magnification image of (A). We can see details of the shape and boundary features of the lesion. (C) OCT-SD: hyperreflective smooth surface elevated retinal mass with optical shadow posterior to the lesion. (D) Ultrasound shows a mass without calcifications (arrow). (E) Fundus autofluorescence shows mild hypoautofluorescence with a small nidus of hyperautofluorescence. (F) Visual fields analysis showed an enlarged blind spot because the lesion is almost attached to the optic nerve. The visual field shows a large scotoma away from the blind spot not related to PSCRAP (encircling).
Discussion
Presumed circumscribed solitary proliferation of retinal astrocytes has recently been described as a small, solitary, well-defined lesion described in the middle ages of life and more frequent in males.Citation3 The lesion is opaque and is a benign retinal tumor abruptly elevated. It is not associated with exudation and lack of intrinsic or perilesional vascular flow.Citation3 This report describes an unusual case which demonstrates disappearance of typical PSCRAP 8 months after diagnosis, leaving a normal appearance of the retina. Only in one patient described by Shields et al,Citation3 the lesion disappeared spontaneously within 1 year. This case was described as the spontaneous disappearance of hyperplasia of astrocytes, before the use of the term presumed circumscribed solitary proliferation of retinal astrocytes.Citation3,Citation4 Shields et alCitation5 consider that the PSCRAP derived from the RPE or deep retina and not in the inner layers as they thought in the first description.Citation3,Citation5 Goldberg and RajaCitation6 also consider that the lesion arises from the deep retina or RPE, whereas with OCT angiography characteristics of the lesion show a lack of intrinsic or paralesional vascular flow, indicating that this lesion is fibrous and likely derived from the RPE or deep retina and not the retinal astrocytes.Citation6 The differential diagnosis includes true tumors of astrocytic as astrocytic hamartoma (AH) and acquired retinal astrocytoma, and diagnosis as retinoblastoma, retinocytoma, simple congenital RPE hamartoma, myelinated fibers, granuloma and reactive gliosis.Citation1,Citation7 AH is a benign tumor that is composed of a proliferation of well-differentiated astrocytes, which is usually diagnosed at early ages of life associated with tuberous sclerosis or as isolated case. It can occur as a calcified or non-calcified variety, and often a combination of the two. The lesions are usually multiple or bilateral and tend to be located peripapillary.Citation1,Citation7,Citation8 Our patient did not have any personal or family sign of tuberous sclerosis complex. An identical tumor is occasionally seen in patients with neurofibromatosis type 1.Citation1 Although AH is considered a stable lesion, spontaneous regression has been described.Citation9 AH presents a diagnostic challenge because of the variable clinical presentation. Four types of AH on SD-OCT have been well described: type 1, flat and within the nerve fiber layer. Type 2 slight elevation with retinal traction. Type 3 typical “moth-eaten” areas caused by calcification, and type 4 with optically empty intralesional cavities ().Citation10 None of them were similar to our case. Acquired astrocytoma of the retina typically appears as a solitary mass with abundant intrinsic vessels, tends to be progressive, and may be associated with exudation or exudative retinal detachment.Citation1,Citation8 Diffuse or nodular glial proliferation can appear with chronic inflammation, ocular trauma, Coats’ disease, retinal hemangioblastoma, or congenital malformations.Citation1 Reactive gliosis can occur in a chronic retinal detachment area or with a scleral buckling in retinal detachment surgery and the gliosis can be extensive simulating tumors.Citation1,Citation2 The immature retina in preterm infants may predispose to the formation of reactive nodular hyperplasia of astrocytes that regress in about 6 months.Citation11 Myelination of the nerve fiber layer is benign, idiopathic, and appears as a chalk-white, sharply demarcated patches on the superficial retina. SD-OCT shows a thickened nerve fiber layer with hyperreflectivity likely due to myelin.Citation12 In summary, PSCRAP is a benign lesion that can regress without visual loss or other alterations. The main importance lies in its differentiation from lesions that can have serious ocular and systemic implications.
Table 1 Showing differences between PSCRAP and AH
Disclosure
The author reports no conflicts of interest in this work.
References
- Shields JA, Shields CL. Glial tumors of the retina. The 2009 king Khaled Memorial Lecture. Saudi J Ophthalmol. 2009;23(3–4):197–201. doi:10.1016/j.sjopt.2009.10.00323960860
- Houston SK, Bourne TD, Lopes MB, et al. Bilateral massive retinal gliosis associated with retinopathy of prematurity. Arch Pathol Lab Med. 2009;133(8):1242–1245. doi:10.1043/1543-2165-133.8.124219653718
- Shields JA, Bianciotto CG, Kivela T. Presumed solitary circumscribed retinal astrocytic proliferation. Arch Ophthalmol. 2011;129(9):1189–1194. doi:10.1001/archophthalmol.2011.21121911666
- Demirci H, Shields CL, Shields JA, et al. Spontaneous disappearance of presumed retinal astrocytic hyperplasia. Retina. 2002;22(2):237–239.11927865
- Shields CL, Roe R, Yannuzzi LA, et al. Solitary circumscribed “pearl white” retinal mass (so-called retinal astrocytic proliferation) resides in deep retina or beneath retina: findings on multimodal imaging in 4 cases. Retin Cases Brief Rep. 2017;11(1):18–23. doi:10.1097/ICB.000000000000027826752524
- Goldberg RA, Raja KM. Presumed solitary circumscribed retinal astrocytic proliferation in the fovea with OCT angiography: a misnomer. Ophthalmic Surg Lasers Imaging Retina. 2018;49(3):212–214. doi:10.3928/23258160-20180221-1129554391
- Schwartz SG, Harbour JW. Spectral-domain optical coherence tomography of presumed solitary circumscribed retinal astrocytic proliferation versus astrocytic hamartoma. Ophthalmic Surg Lasers Imaging Retina. 2015;46(5):586–588. doi:10.3928/23258160-20150521-1326057765
- Kimoto K, Kishi D, Kono H, et al. Diagnosis of an isolated retinal astrocytic hamartoma aided by optical coherence tomography. Acta Ophthalmol. 2008;86(8):921–922. doi:10.1111/j.1600-0420.2007.01141.x19086931
- Moschos MM, Chamot L, Schalenbourg A, et al. Spontaneous regression of an isolated retinal astrocytic hamartoma. Retina. 2005;25(1):81–82.15655446
- Serafino M, Pichi F, Giuliari GP, et al. Retinal astrocytic hamartoma: spectral-domain optical coherence tomography classification and correlation with tuberous sclerosis complex. J Am Assoc Pediatr Ophthalmol Strabismus. 2016;36(6):1199–1208.
- Moshfeghi DM. Presumed transient reactive astrocytic hyperplasia in immature retina. Retina. 2006;26:S69–73. doi:10.1097/01.iae.0000225380.53113.0116946684
- Shelton JB, Digre KB, Gilman J, et al. Characteristics of myelinated retinal nerve fiber layer in ophthalmic imaging: findings on autofluorescence, fluorescein angiographic, infrared, optical coherence tomographic, and red-free images. JAMA Ophthalmol. 2013;131(1):107–109. doi:10.1001/jamaophthalmol.2013.56023307221