Abstract
Purpose
Cystic lymphangioma of the pancreas was first recognized in 1913 as a form of benign cyst. It is extremely rare, accounting for less than 1% of the lymphangiomas.
Case report
Herein, we report a case of cystic pancreatic lymphangioma diagnosed in a 51-year-old female patient who was hospitalized for a colicky upper abdominal pain for a month. Radiological imaging revealed a large multiloculated cystic pancreatic mass with enhancing septations. The patient underwent distal pancreatectomy, and the histological examination showed cystic lymphangioma.
Conclusion
Although very uncommon, cystic lymphangioma should be placed in the differential diagnosis list of pancreatic cystic lesions, at least about the multi-septated ones in asymptomatic female patients which are discovered incidentally.
Background
Lymphangioma is a benign cystic malformation of the lymphatic vessels that usually occur in the children’s head and neck area. The abdominal organs are a rare site for cystic lymphangioma, and the pancreas is also a very rare site of origin.Citation1–Citation3 We would like to report a 51-year-old female case with a large cystic lymphangioma of the pancreas misdiagnosed as mucinous cystic neoplasm in radiology and review the histological differential diagnoses.
Case report
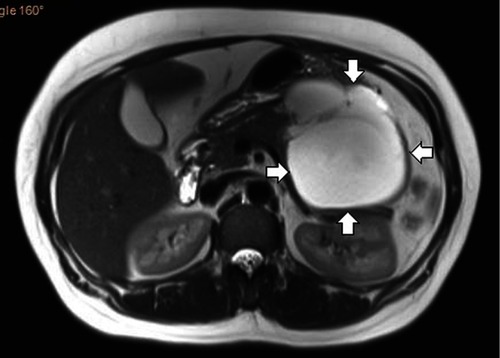
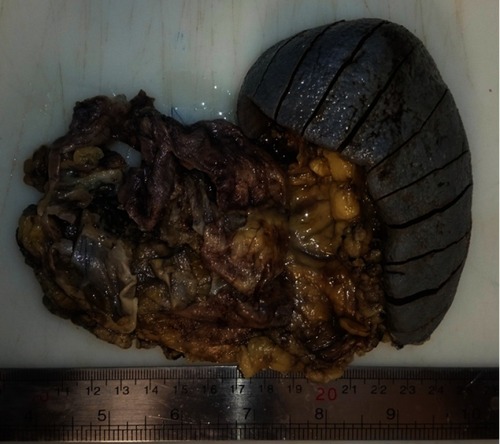
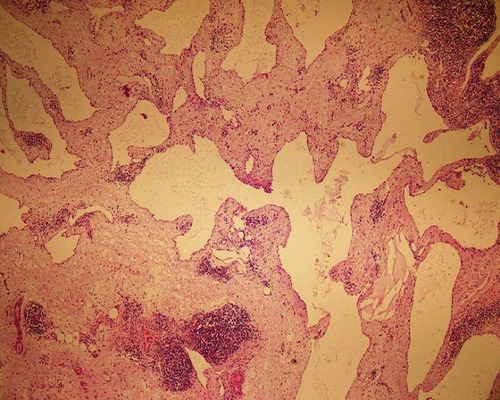
A 51-year-old woman presented with colicky upper abdominal pain for a month. The patient had a medical history that included diabetes mellitus, hypothyroidism (taking medication for them) and hysterectomy (2 years earlier). There was no history of jaundice, weight loss, and loss of appetite. Personal and social history was non-contributory. General physical examination was unremarkable, and her abdomen was soft without any tenderness or mass palpation. Laboratory investigation just showed uncontrolled blood sugar and mild elevation of liver enzymes. Abdominal sonography showed a lobulated and multicystic mass in the retroperitoneum and at the site of the body and tail of the pancreas. Spiral CT scan and MRI of the abdomen revealed a large well-defined multiloculated cystic mass, measuring 11×10 cm with fine septation in the body and tail of the pancreas without any connection to the pancreatic duct, suspicious for a mucinous cystadenoma (). The patient underwent distal pancreatectomy and splenectomy. Splenectomy with pre-operative immunization was done due to the assurance of complete excision of the mass. On pathologic examination, grossly there was a multiloculated gray cystic mass in the body and tail of the pancreas, filled with brown watery fluid (). Histological examination showed multiple large irregular cystic spaces lined by the endothelial cells with pinkish smooth fluid in the lumen and extensive lymphoid aggregation and lymphoid follicles between them, consisting of cystic lymphangioma (). The patient is well without any complication after about 3 months postoperatively. A written informed consent has been provided by the patient for publishing the case report and the publication of the accompanying images. Also, our institutional approval is not required to publish the case details.
Discussion
Lymphangioma is a malformation of the lymphatic system that usually involves young children. Different mechanisms of lymphangioma include failure of the lymphatic system to connect with or separate from the venous system and abnormal budding of the lymphatic system from the cardinal vein. It could also be secondary due to infections, chronic inflammations, obstructions, trauma, and radiological treatment, but the exact underlying cause is unknown in most cases. Recently, the possible impact of lymphangiogenic growth factors on the development of lymphangiomas has been discussed.Citation1–Citation3
The most frequently reported sites are the head and neck (75%), axilla (20%), and other organs (5%).Citation2 Abdominal lymphangiomas are rare benign cystic tumors that can become locally invasive and often require resection. Most tumors were located in the mesenteric region, and less frequently in the mesocolic, greater omental, and retroperitoneal regions, the small intestinal and gastric walls, and the peritoneum. A variety of other sites have been described including the mediastinum, pleura, pericardium, groin, bones, and abdomen. In the abdomen, the mesentery and retroperitoneum are the most common sites.Citation4 Cystic lymphangioma of the pancreas was first identified in 1913 by Koch as a form of benign cyst. It is extremely rare, accounting for less than 1% of lymphangiomas. Frequently occurring in the pancreatic tail, the disease is reported more often in females in all age groups.Citation5
Although often asymptomatic, they can present with a palpable abdominal mass and non-specific gastrointestinal symptoms such as abdominal pain and nausea/vomiting.Citation6 Pancreatic pseudocyst, hydatid cyst, serous and mucinous cystadenoma, intraductal papillary mucinous neoplasm, congenital cyst, rare pancreatic ductal carcinoma (cystic carcinoma of the Wirsung’s Duct), and congenital neoplasms are among the differential diagnosis of pancreatic lymphangioma.Citation4 For distinction between cystic lymphangioma and other differentials, diagnostic tools such as plain abdominal films, abdominal CT, and MRI may be helpful. Plain abdominal X-rays may show dislocation of the intestines, and CT and MRI could help determine the preoperative location of the mass, and assist determining the possibility of communication between the mass and an adjacent structure, the size of the mass and likely complications of the surgery. However, these modalities do not assure a completely precise diagnosis. It is still considered a difficult task to exactly diagnose pancreatic cystic lymphangioma before a surgical procedure,Citation4,Citation5 but the final diagnosis is just made by tissue examination.Citation7
Histologically, there are 3 types of lymphangioma (capillary, cavernous, and cystic). Lymphangiomas may be composed of small and large communicating cysts (cystic lymphangioma) or sponge-like areas composed of small cavernous spaces (cavernous lymphangioma). Sub-classification into capillary, cavernous, or cystic types based on the vessel size is of no clinical significance and is no longer recommended.Citation8
Histologically, there are many differential diagnoses when we have a benign pancreatic cystic lesion. Pseudocysts are the most common type of cystic lesions of the pancreas; there is no epithelial lining, and the adjacent stroma may be hypercellular and may mimic ovarian-type stroma. Any epithelial component within the cyst wall suggests an alternative diagnosis to pseudocyst.Citation9,Citation10
Intraductal papillary mucinous neoplasms (IPMNs) were thought to be very rare, but in recent years, better identification of this neoplasm has led to an increase in its known incidence. Microscopically, papillae with 3 distinct morphologic patterns can be seen: Gastric-foveolar or null type, villous-intestinal type, and pancreatobiliary type.Citation10,Citation11
Mucinous cystic neoplasms (MCN) are supposedly de novo cystic tumors seen almost solely in perimenopausal female patients and mostly appear in the body or tail of the pancreas. MCNs are composed of thick-walled multilocular cysts that can become very large. Microscopically, the cysts are lined by tall, columnar, mucin-producing epithelium that is similar to endocervical epithelium.Citation10,Citation12 In , the characteristics of pancreatic mucinous neoplasm and cystic lymphangioma are presented.
Table 1 Comparison of characteristics of pancreatic mucinous neoplasm and cystic lymphangioma
Serous cystadenoma (SCA) is a benign neoplasm composed of uniform glycogen-rich epithelial cells that form countless small cysts containing serous fluid. Nearly, two-thirds of SCAs arise in the body-tail region of the pancreas and are seen prevalently in female patients. The lesions usually present as large masses and the cut surface shows numerous, tightly packed, small, thin-walled cysts (spongelike or honeycomb appearance) organized around a central stellate scar. Microscopically, the single layer of cuboidal or flattened cells lining the small cysts has well-defined cytoplasmic borders, pale to clear cytoplasm, and small, round uniform nuclei with dense, homogeneous chromatin and inconspicuous nucleoli.Citation10,Citation13
Lymphoepithelial cysts are multilocular (60%) or unilocular (40%) cystic lesions mostly seen in older adults with a male predominance. They can be seen in any component of the pancreas and often project into the peripancreatic tissues. Microscopically, the cysts are lined by well-differentiated stratified squamous epithelium, usually with keratinization.Citation10
Rarely, hydatid cysts, necrotic tuberculosis infections, and other entities can occur in the pancreas and mimic primary cystic neoplasms.Citation10
The majority of cystic tumors of the pancreas are slow-growing and asymptomatic. Several studies reported that no imaging studies are adequately accurate to differentiate between the benign, premalignant, and malignant lesions.Citation14,Citation15 Percutaneous or endoscopic aspiration has the potential to spill malignant cells with the possibility of reducing survival, so it is not usually recommended to use these invasive and expensive diagnostic procedures.Citation15 In the absence of a good radiologic or pathologic test to preoperatively determine the diagnosis, clinical characteristics such as age, gender, the presence of symptoms, cyst size, or location might be helpful.Citation14 No specific symptom was meaningfully associated with the possibility of malignancy although increasing anorexia, jaundice, and weight loss (10–40%) may be associated with malignant changes.Citation16,Citation17 Older patients are more likely to have premalignant or malignant cystic pancreatic neoplasms. The overall incidence of malignancy is higher in men.Citation15 High values of CEA and CA 19–9 show a high positive predictive value for pancreatic malignancy or pre-malignancy in the preoperative assessment of pancreatic cystic mass (70–100%).Citation16,Citation18 The presence of a solid component, invading outside the pancreas, or pancreatic duct obstruction through endoscopic ultrasound is highly indicative of malignancy.Citation15,Citation19–Citation21 Some authors suggest that the size of the cystic lesion is an indicator of its malignant potential, lesions larger than 2 cm in size merit aggressive management due to the higher risk of malignant potential.Citation17,Citation22,Citation23
The treatment of choice of pancreatic lymphangioma is complete surgical resection with a very low chance of recurrence and the overall prognosis is excellent.Citation31 Partial resection is associated with a high recurrence rate, 50% in one series after a mean follow-up period of 2 years. Although lymphangioma is a benign tumor, it often behaves in an aggressive manner and can grow to an enormous size. Therefore, resection of the adjacent organs may be required to accomplish complete excision.Citation32
Conclusion
Although very uncommon, cystic lymphangioma should be placed in the differential diagnosis list of pancreatic cystic lesions, at least about the multiseptated ones in asymptomatic female patients, which are discovered incidentally. Clinical and radiological characteristics are not helpful in preoperative diagnosis of pancreatic lymphangioma and differentiation with mucinous neoplasm. Pathological examination is necessary for definite diagnosis.
Acknowledgment
The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran, and Center for Development of Clinical Research of Nemazee Hospital and Dr. Nasrin Shokrpour for editorial assistance.
Disclosure
The authors report no conflicts of interest in this work.
References
- Wiegand S, Eivazi B, Barth PJ, et al. Pathogenesis of lymphangiomas. Virchows Arch. 2008;453(1):1–8. doi:10.1007/s00428-008-0611-z18500536
- Losanoff JE, Richman BW, El-Sherif A, Rider KD, Jones JW. Mesenteric cystic lymphangioma. J Am Coll Surg. 2003;196(4):598–603. doi:10.1016/S1072-7515(02)01755-612691938
- Allen JG, Riall TS, Cameron JL, Askin FB, Hruban RH, Campbell KA. Abdominal lymphangiomas in adults. J Gastrointest Surg. 2006;10(5):746–751. doi:10.1016/j.gassur.2005.10.01516713549
- Mousavi SR, Moradi A, Sobhiyeh MR, et al. A patient with cystic lymphangioma in pancreas. Gastroenterol Hepatol Bed Bench. 2013;6(3):159–164.24834265
- Colovic RB, Grubor NM, Micev MT, Atkinson HD, Rankovic VI, Jagodic MM. Cystic lymphangioma of the pancreas. World J Gastroenterol. 2008;14(44):6873–6875. doi:10.3748/wjg.14.687319058318
- Black T, Guy CD, Burbridge RA. Retroperitoneal cystic lymphangioma diagnosed by endoscopic ultrasound-guided fine needle aspiration. Clin Endosc. 2013;46(5):595–597. doi:10.5946/ce.2013.46.5.59524143329
- Igarashi A, Maruo Y, Ito T, et al. Huge cystic lymphangioma of the pancreas: report of a case. Surg Today. 2001;31(8):743–746. doi:10.1007/s00595017008411510617
- Schneider G, Seidel R, Altmeyer K, et al. Lymphangioma of the pancreas and the duodenal wall: MR imaging findings. Eur Radiol. 2001;11(11):2232–2235. doi:10.1007/s00330010084611702164
- Klöppel G. Pseudocysts and other non-neoplastic cysts of the pancreas. Semin Diagn Pathol. 2000;17(1):7–15.10721803
- Basturk O, Coban I, Adsay NV. Pancreatic cysts: pathologic classification, differential diagnosis, and clinical implications. Arch Pathol Lab Med. 2009;133(3):423–438. doi:10.1043/1543-2165-133.3.42319260748
- Adsay NV. The “new kid on the block”: intraductal papillary mucinous neoplasms of the pancreas: current concepts and controversies. Surgery. 2003;133(5):459–463. doi:10.1067/msy.2003.12712773972
- Albores-Saavedra J, Gould EW, Angeles-Angeles A, Henson DE. Cystic tumors of the pancreas. Pathol Annu. 1990;25 Pt 2:19–50.2202959
- Compton CC. Serous cystic tumors of the pancreas. Semin Diagn Pathol. 2000;17(1):43–55.10721806
- Spinelli KS, Fromwiller TE, Daniel RA, et al. Cystic pancreatic neoplasms: observe or operate. Ann Surg. 2004;239:651–657. doi:10.1097/01.sla.0000124299.57430.ce15082969
- Atef E, El Nakeeb A, El Hanafy E, El Hemaly M, Hamdy E, El-Geidie A. Pancreatic cystic neoplasms: predictors of malignant behavior and management. Saudi J Gastroenterol. 2013;19(1):45–53. doi:10.4103/1319-3767.10592723319038
- Garcea G, Ong SL, Rajesh A, et al. Cystic lesions of the pancreas. A diagnostic and management dilemma. Pancreatology. 2008;8(3):236–251. doi:10.1159/00013427918497542
- Fernandez-del Castillo C, Targarona J, Thayer SP, Rattner DW, Brugge WR, Warshaw AL. Incidental pancreatic cysts: clinicopathologic characteristics and comparison with symptomatic patients. Arch Surg. 2003;138(4):427–423. discussion 433–424. doi:10.1001/archsurg.138.4.427
- Naveed S, Qari H, Banday T, Altaf A, Para M. Mucinous cystic neoplasms of pancreas. Gastroenterol Res. 2014;7(2):44–50. doi:10.14740/gr600e
- Sahani DV, Kadavigere R, Saokar A, Fernandez-del Castillo C, Brugge WR, Hahn PF. Cystic pancreatic lesions: a simple imaging-based classification system for guiding management. Radiographics. 2005;25(6):1471–1484. doi:10.1148/rg.25604516116284129
- Lee CJ, Scheiman J, Anderson MA, et al. Risk of malignancy in resected cystic tumors of the pancreas ≤3 or = cm in Size: is it safe to observe asymptomatic patients? A multi-institutional report. J Gastrointest Surg. 2008;12:234–242. doi:10.1007/s11605-007-0381-y18040749
- Javle M, Shah P, Yu J, et al. Cystic Pancreatic Tumors (CPT): predictors of malignant behavior. J Surg Oncol. 2007;95:221–228. doi:10.1002/jso.2064817323335
- Silas AM, Morrin MM, Raptopoulos V, Keogan MT. Intraductal papillary mucinous tumours of the pancreas. AJR. 2001;176:179–185. doi:10.2214/ajr.176.1.176017911133563
- Sarr MG, Kendrick ML, Nagorney DM, Thompson GB, Farley DR, Farnell M. Cystic neoplasm of the pancreas: benign to malignant epithelial neoplasms. Surg Clin North Am. 2001;81:497–509. doi:10.1016/s0039-6109(05)70139-011459267
- Choi JH, Seo DW, Song TJ, et al. Long-term outcomes after endoscopic ultrasound-guided ablation of pancreatic cysts. Endoscopy. 2017;49(9):866–873. doi:10.1055/s-0043-11003028511236
- Pak LM, D’Angelica MI, DeMatteo RP, et al. Natural history of patients followed radiographically with mucinous cysts of the pancreas. J Gastrointest Surg. 2017;21(10):1599–1605. doi:10.1007/s11605-016-3338-128516310
- Joshi U, Poudel P, Ghimire RK, Basnet B. Pancreatic pseudocyst or mucinous cystadenocarcinoma of pancreas? A diagnostic dilemma. Clin Case Rep. 2017;5(4):501–504. doi:10.1002/ccr3.88728396777
- Leung TK, Lee CM, Shen LK, Chen YY. Differential diagnosis of cystic lymphangioma of the pancreas based on imaging features. J Formos Med Assoc. 2006;105(6):512–517. doi:10.1016/S0929-6646(09)60193-516801041
- Carvalho D, Costa M, Russo P, Simas L, Baptista T, Ramos G. Cystic pancreatic lymphangioma - Diagnostic role of endoscopic ultrasound. GE Port J Gastroenterol. 2016;23(5):254–258. doi:10.1016/j.jpge.2016.01.00628868471
- Viscosi F, Fleres F, Mazzeo C, Vulcano I, Cucinotta E. Cystic lymphangioma of the pancreas: a hard diagnostic challenge between pancreatic cystic lesions-review of recent literature. Gland Surg. 2018;7(5):487–492. doi:10.21037/gs.2018.04.0230505770
- Sohn BK, Cho CH, Chae HD. Cystic lymphangioma of the pancreas. J Korean Surg Soc. 2011;81(2):141–145. doi:10.4174/jkss.2011.81.2.14122066114
- Cherk M, Nikfarjam M, Christophi C. Retroperitoneal lymphangioma. Asian J Surg. 2006;29(1):51–54. doi:10.1016/S1015-9584(09)60297-916428102
- Dalla Bona E, Beltrame V, Blandamura S, Liessi F, Sperti C. Huge cystic lymphangioma of the pancreas mimicking pancreatic cystic neoplasm. Case Rep Med. 2012;2012:951358. doi:10.1155/2012/95135823197988