Abstract
A typical patient with chronic obstructive pulmonary disease has small airway disease, which often responds to bronchodilators. If the patient is obese, he or she may be further compromised and not tolerate being in the supine position. We present a case of a patient with history of chronic obstructive pulmonary disease and obstructive sleep apnea with acute renal failure and urosepsis scheduled for an emergent debridement of Fournier’s gangrene. In this patient, the fiberoptic intubation was performed in semi-Fowler’s position, and tracheomalacia was observed.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Case report
A 54-year-old man who weighed 168 kg and was 1.75 m tall (body mass index, 56 kg/m2), with a history of chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea on continuous positive airway pressure for 10 years at home was admitted to the emergency department with acute renal failure and sepsis. He was scheduled for an emergent debridement of Fournier’s gangrene.
The emergency physician consulted anesthesiology for intubation because of respiratory failure. As a result of the patient’s history of COPD, he was unable to compensate for the metabolic acidosis that was secondary to his sepsis. Other past medical history included coronary artery disease treated with percutaneous coronary intervention and stenting, a 30 pack-year smoking history, and morbid obesity.
Physical examination in the emergency department revealed respiratory distress, tachypnea, and diffuse bilateral wheezing. Airway assessment showed a mouth opening of three finger-breadths, Mallampati airway classification 3, and a thyromental distance of 6 cm with a neck circumference of 44 cm. In the sitting position, the patient’s blood oxygen saturation was 99% on a fraction of inspired oxygen of 0.5. When the patient positioned supine, he became cyanotic, with blood oxygen saturation ~85% on a fraction of inspired oxygen of 0.5, with increased intensity during inspiration with coarse, low-pitched wheezing and dyspnea. He received bronchodilators without improvement of the wheezing.
After assessing the patient, the anesthetic plan was discussed with the patient and the surgical team. An elevated prothrombin time of 24 seconds (international normalized ratio, 3.6) and septic shock contraindicated regional anesthesia. Out of concern for maintaining the patient’s airway, it was felt that a general anesthetic with an awake fiberoptic endotracheal intubation in the operating room was the safest way to proceed. The surgical team would be immediately available for a surgical airway in case of an emergency.
In the operating room, the fiberoptic intubation was performed in the semi-Fowler’s position (45°) after bilateral superior laryngeal nerve block and transtracheal instillation of 4% lidocaine. During bronchoscopy, tracheomalacia was observed. The wheezing was completely resolved after insertion of an endotracheal tube, which stented the airway open and improved air entry. Debridement of the Fournier’s gangrene proceeded. As a result of underlying septic shock with hypotension, the patient needed vasoactive agents (phenylephrine). Intraoperative arterial blood gas showed a pH of 7.26, a partial pressure of carbon dioxide of 34 mmHg, a partial pressure of oxygen of 320 mmHg, HCO3− levels of 16.0, base excess −11, and a blood oxygen saturation of 100%. At the conclusion of surgery, the patient remained intubated and transferred to the intensive care unit for further management. In the intensive care unit, the patient was treated with antibiotics and inotropic support for septic shock. Patient was receiving pressure-regulated volume control ventilation in the intensive care unit with a fraction of inspired oxygen of 1.0, a respiratory rate of 20 breaths per minute, a peak inspiratory pressure of 25 mmHg, and a positive end-expiratory pressure if 7 mmHg. The patient developed acute respiratory distress syndrome postoperatively. A computed tomography scan of the chest showed bilateral infiltrates in lung bases as a result of sepsis. On fifth postoperative day, the patient succumbed to multiorgan dysfunction, including hepatic, renal, cardiac, and pulmonary systems related to Fournier’s gangrene and sepsis syndrome.
Discussion
Difficulties encountered in tracheal intubation in obese patients are associated with high morbidity and mortality related to anesthesia.Citation1 Increased risk of difficult intubation in obese patients is associated with decreased thyromental distance (<6 cm), increased neck circumference (>40 cm), increased body mass index (>35 kg/m2), and a Mallampati airway grade higher than 2.Citation2,Citation3 Optimal care includes identifying the risk for airway difficulties and planning an approach for securing the airway.Citation4,Citation5
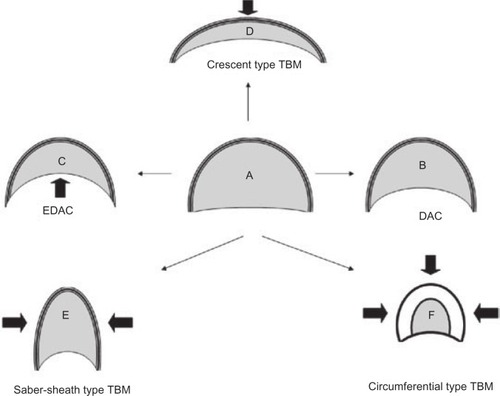
Tracheomalacia is characterized by the flaccidity of the supporting cartilage and hypotonic myoelastic elements. These factors cause tracheal collapse, especially during times of increased airflow associated with increased airway dynamic pressure changes, such as coughing ().Citation6 It is also associated with intermittent or continuous dyspnea, difficulty in clearing secretions, cough, wheezing, pneumonia, and recurrent bronchitis.
Figure 1 Airway dynamics: tracheomalacia.
The etiology includes genetic causes (polychondritis), posttraumatic (long-term tracheal intubation, tracheostomy, closed chest trauma, after lung transplantation), COPD, chronic external compression of the trachea (malignancy, benign tumors, cysts, abscesses, and aortic aneurysms), and vascular rings.Citation6 Tracheomalacia related to chronic obstructive lung disease causes high-grade, chronic, long-segment airway obstruction.Citation7 The incidence of tracheomalacia is 3% in patients with COPD.Citation8
In patients with a difficult airway with Mallampati airway grade higher than two, increased neck circumference (>40 cm), with elevated body mass index (>35 kg/m2) and a history of COPD unresponsive to bronchodilator therapy, the risk of tracheomalacia is elevated, and awake fiberoptic intubation is the best option for securing the airway. In the index patient, the endotracheal tube functioned as a stent and relieved the obstruction caused by tracheomalacia.
Flexible bronchoscopy is the gold standard method of diagnosing tracheomalacia, but it is not always feasible in settings with limited resources. In the absence of other modalities for diagnosis, fluoroscopy should be considered in the setting of persistent respiratory symptoms compatible with the clinical picture of tracheomalacia.Citation9
Wheezing in morbidly obese COPD patients is not always caused by small airway disease. In this case, the patient had tracheomalacia and the solution for this was awake fiberoptic intubation.
Acknowledgments
The authors thank Dr Joseph SchianodiCola, Chairman, Department of Anesthesiology, New York Methodist Hospital, for providing general support to write this paper.
Disclosure
The authors report no conflicts of interest in this work.
References
- ShigaTWajimaZInoueTSakamotoAPredicting difficult intubation in apparently normal patients: a meta-analysis of bedside screening test performanceAnesthesiology2005103242943716052126
- GonzalezHMinvilleVDelanoueKMazerollesMConcinaDFourcadeOThe importance of increased neck circumference to intubation difficulties in obese patientsAnesth Analg200810641132113618349184
- BrodskyJBLemmensHJBrock-UtneJGVierraMSaidmanLJMorbid obesity and tracheal intubationAnesth Analg200294373273611867407
- BenumofJLManagement of the difficult adult airway. With special emphasis on awake tracheal intubationAnesthesiology1991756108711101824555
- LienhartAAuroyYPéquignotFSurvey of anesthesia-related mortality in FranceAnesthesiology200610561087109717122571
- MurguSDColtHGTracheobronchomalacia and excessive dynamic airway collapseRespirology200611438840616771908
- GaissertHABurnsJThe compromised airway: tumors, strictures, and tracheomalaciaSurg Clin North Am20109051065108920955884
- HasegawaIBoisellePMRaptopoulosVHatabuHTracheomalacia incidentally detected on CT pulmonary angiography of patients with suspected pulmonary embolismAJR Am J Roentgenol200318161505150914627565
- SanchezMOGreerMCMastersIBChangABA comparison of fluoroscopic airway screening with flexible bronchoscopy for diagnosing tracheomalaciaPediatr Pulmonol2012471636721830315
