Abstract
Toxoplasmosis complicating lung cancer has been described only rarely. Here, we report a case of acute Toxoplasma gondii infection in a patient with squamous lung cancer. A 64-year-old woman was admitted to our hospital with a history of cough of 6 months’ duration and chest pain of 1 week’s duration. Further examination revealed multiple swollen lymph nodes, palpable on the top of the right collarbone and without tenderness. The chest X-ray, bronchoscopy, and computed tomography scan confirmed squamous carcinoma of the right lung. The Wright-stained bronchoalveolar-lavage fluid cytology diagnosis was positive for T. gondii and tachyzoites were detected. All of them were of free type (ectocytic), without intracellular parasites. Serological examination revealed that the anti-T. gondii immunoglobulin (Ig) M and IgG antibodies were positive. Unfortunately the patient did not continue treatment and was lost to follow-up. Toxoplasmosis is a life-threatening opportunistic infection in patients with lung cancer. Prompt recognition of T. gondii infection among cancer patients with subsequent targeted treatment of toxoplasmosis could help alleviate symptoms and improve survival.
Introduction
Toxoplasma gondii infection, “toxoplasmosis”, is relatively common, and the prevalence of carrying the dormant, cystic form has been reported as 40% in Europe, 20%–50% in Africa,Citation1 and 10%–30% in the People’s Republic of China.Citation1,Citation2 Most people who carry T. gondii are healthy, but for those with HIV or cancer toxoplasmosis can be life-threatening. Toxoplasmosis has been reported to increase the fatality rate of Hodgkin’s disease, leukemia, myeloma, melanoma, AIDS, and brain cancer.Citation2–Citation12 Although toxoplasmosis is known to complicate pneumonia and other respiratory diseases,Citation12–Citation20 its role in lung cancer has not been adequately described. Here, we describe a case of toxoplasmosis presenting with non-small-cell lung cancer for the purpose of making screening and treatment recommendations.
Case presentation
A 64-year-old Chinese woman was admitted to our hospital with a history of nonproductive cough (without hemoptysis) of 6 months’ duration and chest pain of 1 week’s duration. She had lived in a rural area with a cat for many years. She had no history of eating raw or undercooked foods and she was uncertain whether she had ever drunk unpasteurized goat’s milk. Her medical history was unremarkable. She did not have shortness of breath, fever or sweats, weight loss, or a history of smoking. Physical examination revealed multiple swollen lymph nodes palpable on the top of the right collarbone, without tenderness. Temperature, respiration, heart rate, and abdominal examination showed no abnormalities. Other systemic examinations were within normal limits.
The chest radiograph showed bilateral prominence and right hila adenopathy. Computed tomography scan of the lung showed space-occupying lesions in the lower right lobe confirming centrally located carcinoma. We also observed significant enlargement of the lymph nodes in the right hilar areas and mediastinum, which we considered malignant. The patient also had pneumonia in the right lung. Bronchoscopy suggested that tracheal carina was broadened; the ridge between upper right lobe and middle bronchus was widened, as was the ridge between middle right lobe and lower lobe bronchus. Bronchoscopy also showed the right posterior basal bronchus suffered from compressed bronchostenosis. Squamous carcinoma cells were found in the bronchial brushing. There was no evidence of distant metastasis. Echocardiography suggested pulmonary hypertension. Pulmonary ventilation and small-airway function were mildly blocked.
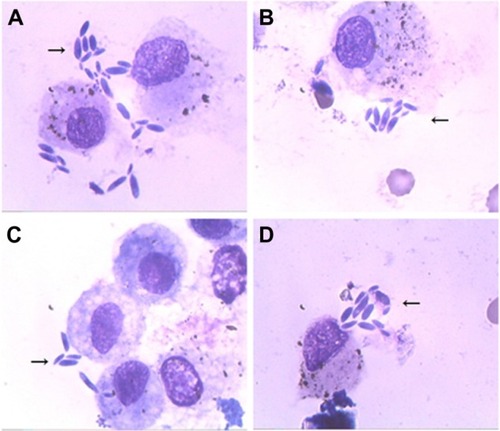
Laboratory testing demonstrated no obvious abnormality except the carcinoembryonic antigen level was at 8.21 ng/mL (reference interval: 0–5 ng/mL). Exfoliative cytology examination of the hydrothorax did not detect tumor cells. Interestingly, the Wright-stained bronchoalveolar-lavage (BAL) fluid cytology diagnosis was positive for T. gondii (), and many crescent-shaped tachyzoites were detected in clumps around host cells (indicated by an arrow in each of ). Individual elongated bodies averaged 4–7 μm in length, with a pointed anterior end and rounded posterior end; one side was slightly flattened, the other side bulged. The nucleus was situated toward the center. All of the tachyzoites were extracellular (ectocytic); no intracellular parasite was evident. Serological examination revealed that anti-T. gondii immunoglobulin (Ig) M and IgG antibodies were positive. Other lab tests were unremarkable. The leukocyte count was 5.64×109/L (41.8% lymphocytes, 52.1% neutrophils, 5.3% monocytes), and liver function tests were within the normal ranges (albumin 42.8 g/L, total bilirubin 10.10 μmol/L, direct bilirubin 2.5 μmol/L, alanine aminotransferase [ALT] 7.0 IU/L, aspartate transaminase [AST] 17.0 IU/L). Serology testing for HIV was negative.
Figure 1 Wright-stained bronchoalveolar lavage fluid smears.
Upon diagnosis of lung cancer, the patient decided to forgo any kind of treatment and we subsequently lost contact with her.
Discussion
T. gondii is an obligate intracellular protozoan.Citation15 The life-cycle of T. gondii is divided into five stages: trophozoite, cyst, schizont, gametophyte, and oocyst. Final maturation to sexual maturity occurs only in the intestines of cats. The main route of infection of T. gondii is fecal–oral transmission. It also can be transmitted to the fetus through the placenta. Generally, eosinophilia is not typical when infected with the protozoan. Clinical manifestations are complicated and atypical, and most infections are latent or acute. Differential diagnosis relies mainly on direct detection of Toxoplasma tachyzoites in BAL or by serological techniques.
Among healthy people, toxoplasmosis is generally mild and self-limiting, but among neonates and cancer patients, this opportunistic infection is serious, often fatal. Many cases of pulmonary toxoplasmosis have been described in patients with hematologic malignancies and solid tumors, but none in lung cancer, as far as we are aware.
We discovered a rare case of T. gondii infection in a lung cancer patient, with diagnosis of infection based on tachyzoites present in BAL and positive T. gondii-specific IgM antibody, and diagnosis of squamous lung cancer based on chest X-ray, bronchoscopy, and computed tomography scan.
Other investigators have described pulmonary toxoplasmosis in those with HIV or cancer,Citation13–Citation20 although not in lung cancer. A French nationwide study reviewed 64 cases of BAL-confirmed pulmonary toxoplasmosis among patients with HIV infection; 30 (47%) of the 64 cases were responsive to toxoplasmosis treatment, while 24 patients (37%) died of toxoplasmosis. Israelsky and Remington, in the USA, have also reported improved outcomes resulting from treatment of T. gondii infection among immune compromised patients.Citation5 They reported improvement in 68% of patients for whom the diagnosis was made early enough to begin treatment.Citation5 De Salvador-Guillouët et al reported a case of severe acute primary pulmonary toxoplasmosis in an immunocompetent of 19-year-old French man with BAL-confirmed tachyzoites.Citation14 Leal et al reported a similar case in Brazil.Citation19 In their paper, Leal et al also reviewed nine other cases of T. gondii pneumonia. Most of these cases had positive IgM and IgG T. gondii-specific antibodies and tachyzoite in BAL fluid. Fortunately most of these patients responded to treatment and made a full recovery.
Clinicians should be aware of toxoplasmosis complicating lung cancer, as toxoplasmosis is readily treatable. Indeed, in some countries T. gondii serology is ordered routinely during examination of cancer patients, with BAL fluid being the material of choice for diagnosing pulmonary toxoplasmosis as well as lung biopsies.Citation16–Citation18
We report a case of toxoplasmosis complicating squamous cell lung cancer in the People’s Republic of China. We recommend consideration of periodic monitoring of T. gondii infection in lung cancer patients in order to improve treatment and increase survival.
Acknowledgments
We would like to thank Dr Lisa Herrinton (Division of Research, Kaiser Permanente, Oakland, CA, USA) and Dr Changyu Zheng (National Institute of Dental and Craniofacial Research, National Institute of Health, Bethesda, MD, USA) for editing this manuscript. This study was funded by the Technology Development Program of Jilin Province (no 200705178).
Disclosure
The authors report no conflict of interest in this work.
References
- FurtadoJMSmithJRBelfortRJrGatteyDWinthropKLToxoplasmosis: a global threatJ Glob Infect Dis20113328128421887062
- ZhouPChenZLiHLToxoplasma gondii infection in humans in ChinaParasit Vectors2011416521864327
- CareyRMKimballACArmstrongDLiebermanPHToxoplasmosis. Clinical experiences in a cancer hospitalAm J Med197354130384509169
- DarcyFSantoroFToxoplasmosisKierszenbaumFParasitic Infections and the Immune SystemNew York, NYAcademic Press1994163201
- IsraelskyDMRemingtonJSToxoplasmosis in patients with cancerClin Infect Dis199317Suppl 2S423S4358274608
- EdvinssonBLappalainenMAnttilaVJPaetauAEvengårdBToxoplasmosis in immunocompromized patientsScand J Infect Dis200941536837119229764
- ScerraSCoignard-BiehlerHLanternierFDisseminated toxoplasmosis in non-allografted patients with hematologic malignancies: report of two cases and literature reviewEur J Clin Microbiol Infect Dis201332101259126823595587
- VietzkeWMZeldermanAHGrimleyPHWelsmisMPToxoplasmosis complicating malignancy. Experience at the National Cancer InstituteCancer19682158168274296934
- LazenbyGBOpportunistic infections in women with HIV AIDSClin Obstet Gynecol201255492793723090461
- BenitoNMorenoAMiroJMTorresAPulmonary infections in HIV-infected patients: an update in the 21st centuryEur Respir J201239373074521885385
- PupaiboolJLimperAHOther HIV-associated pneumoniasClin Chest Med201334224325423702174
- TokmanSHuangLEvaluation of respiratory diseaseClin Chest Med201334219120423702170
- RabaudCMayTLucetJCLeportCAmbroise-ThomasPCantonPPulmonary toxoplasmosis in patients infected with human immunodeficiency virus: a French National SurveyClin Infect Dis1996236124912548953067
- De Salvador-GuillouëtFAjzenbergDChaillou-OpitzSSevere pneumonia during primary infection with an atypical strain of Toxoplasma gondii in an immunocompetent young manJ Infect2006532e47e5016352339
- BlackMWBoothroydJCLytic cycle of Toxoplasma gondiiMicrobiol Mol Biol Rev200064360762310974128
- PomeroyCFiliceGAPulmonary toxoplasmosis: a reviewClin Infect Dis19921448638701576281
- SingALeitritzLRoggenkampAPulmonary toxoplasmosis in bone marrow transplant recipients: report of two cases and reviewClin Infect Dis199929242943310476754
- OksenhendlerECadranelJSarfatiCToxoplasma gondii pneumonia in patients with the acquired immunodeficiency syndromeAm J Med1990885N18N21N
- LealFECavazzanaCLde AndradeHFJrGalisteoAJrde MendonçaJSKallasEGToxoplasma gondii pneumonia in immunocompetent subjects: case report and reviewClin Infect Dis2007446e62e6617304443
- VijayanVKParasitic lung infectionsCurr Opin Pulm Med200915327428219276810
